Introduction
Hypertrophy of the inferior turbinate can contribute to significant nasal obstruction. When medical management has proved unhelpful, a variety of surgical techniques have been described to reduce the turbinate. These include reduction or excisional approaches, such as submucosal diathermy, microdebrider-assisted submucosal resection, outfracture, cryosurgery, and partial or total turbinectomy. Submucosal diathermy to the inferior turbinate is a frequently performed procedure for turbinate reduction, with few complications.
A case of a patulous nasolacrimal duct with reflux of air and mucus on to the ocular surface following submucosal diathermy to the inferior turbinate is described. The need to consider nasolacrimal duct system complications during the pre-operative discussion is emphasised.
Case report
A 33-year-old male patient presented to a tertiary bi-disciplinary nasolacrimal clinic with a history of a bubbling sensation and mucoid discharge from the right medial canthus on blowing the nose and sneezing. He had undergone an otherwise uneventful revision septoplasty, submucosal diathermy to both inferior turbinates, bilateral antral washout and left intranasal antrostomy a few months earlier, at another hospital, for nasal obstruction with associated hyposmia and post-nasal drip. He was a non-smoker and there were no symptoms of allergic rhinitis. There was no previous history of epiphora or other nasolacrimal symptoms.
Endoscopic examination demonstrated a markedly reduced inferior turbinate remnant on the right side with scarring immediately adjacent to a widely open nasolacrimal duct opening (Figure 1) into the apex of the inferior meatus.
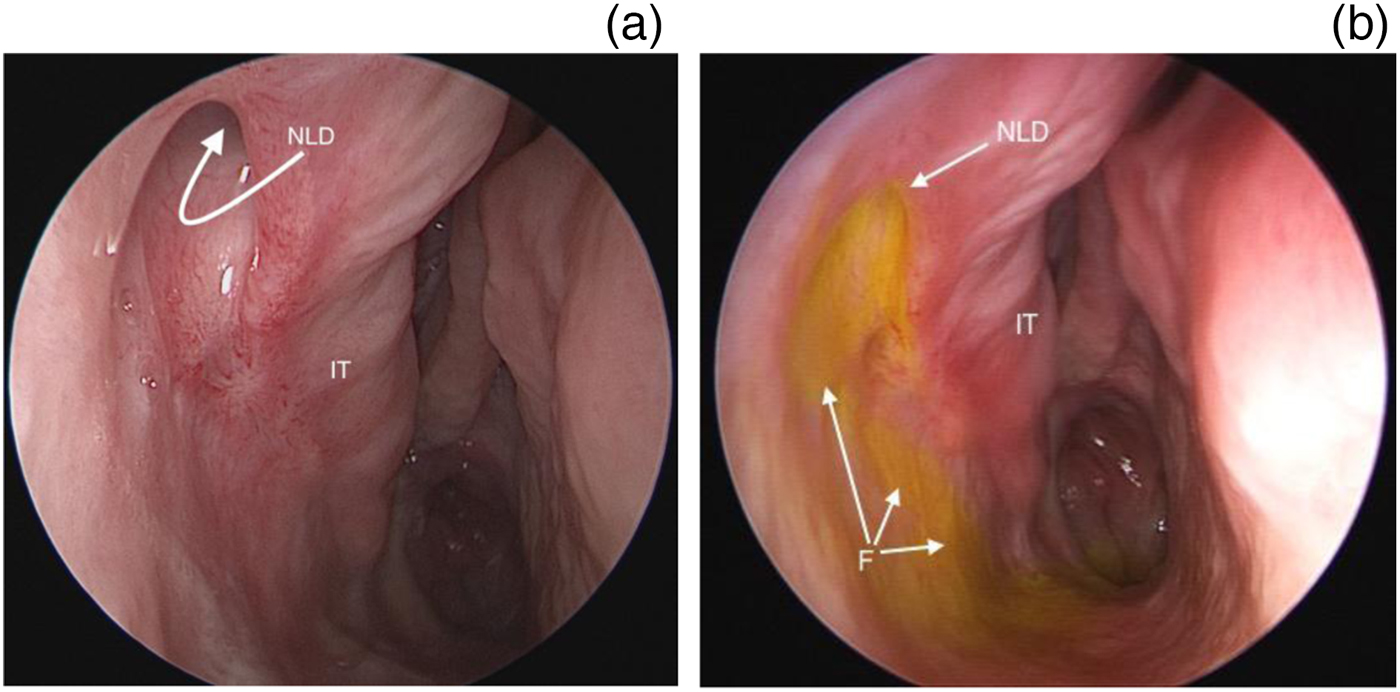
Fig. 1. Endoscopic views of right nostril (a) before and (b) after fluorescein application topically to the ocular surface. A scarred and lateralised inferior turbinate remnant (‘IT’) can clearly be seen, with a patulous nasolacrimal duct opening (‘NLD’) visible anteriorly and a fluorescein trail (‘F’) flowing freely into nasal cavity.
Nasolacrimal probing and irrigation demonstrated free flow into the nasal cavity. Fluorescein applied topically to the eye cleared immediately into the nose. The contralateral nasolacrimal system syringing (Figure 2) indicated patency, but there was no visible spontaneous clearance of fluorescein into the inferior meatus at the same time point as that seen on the right side.
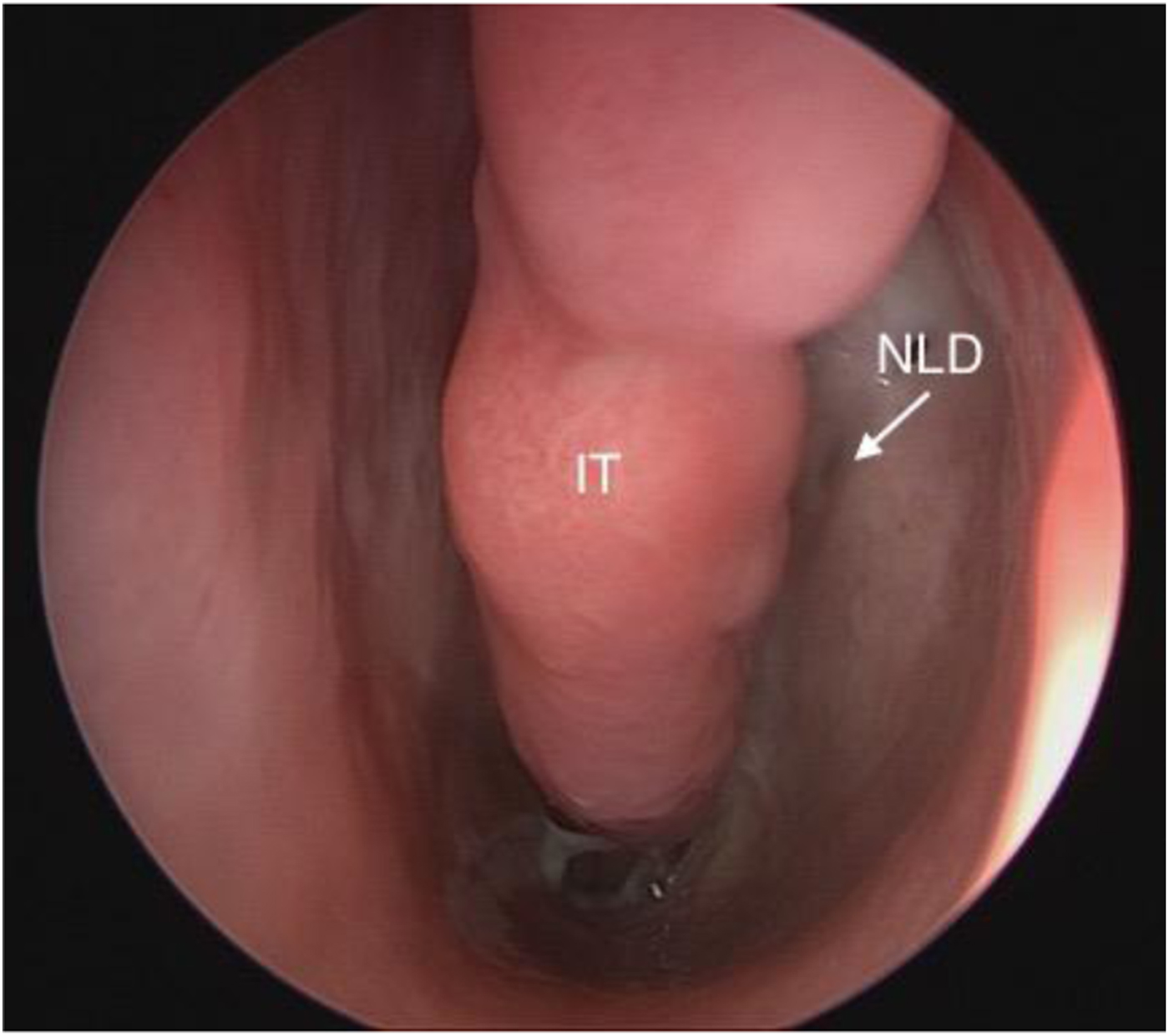
Fig. 2. Endoscopic view of left nostril, showing a surgically reduced inferior turbinate (‘IT’), and a visible and normal nasolacrimal duct opening (‘NLD’). In contrast to Figure 1, no fluorescein clearance can be seen at an identical time point to Figure 1, indicating effective function of the valve of Hasner.
Computed tomographic dacryocystography demonstrated an air-filled nasolacrimal sac and duct, in continuity with the nasal cavity. The bony lateral nasal wall was intact radiologically.
Although the patient found the symptoms a nuisance, he elected to adopt an expectant approach, having been reassured as to the absence of a more serious underlying aetiology.
Discussion
The nasolacrimal duct extends from the base of the lacrimal sac to the inferior meatus of the nose. The inferior orifice varies greatly from a round opening at the highest part of the inferior turbinate to a more slit-like arrangement at varying levels on the lateral wall. The mucosal and submucosal linings of the nasolacrimal duct create a number of indentations or corrugations that are visible with contrast imaging and which may have a valvular-like function. The most constant and well-developed of these valve-like features is the valve of Hasner, located at the lower end of the duct as it enters the inferior meatus. This valve is thought to prevent the upward escape of air and liquids towards the lacrimal sac when blowing the nose.Reference Bron, Tripathi and Tripathi1
Hypertrophy of the inferior turbinate can contribute to significant nasal obstruction. When medical management has proved unhelpful, a variety of surgical techniques have been described. These include reduction or excisional approaches, such as submucosal diathermy, microdebrider-assisted submucosal resection, outfracture, cryosurgery, and partial or total turbinectomy.Reference Williams, Fisher and Golding-Wood2
Submucosal diathermy to the inferior turbinate was popularised by Simpson and Groves.Reference Simpson and Groves3 It is a widely practised procedure,Reference Talat, El-Sabawy, Baky and Raheem4 used to reduce the size of the chronically engorged inferior turbinate, with reported symptom improvements in 55–72 per cent of patients.Reference Von Haacke and Hardcastle5 The technique involves using a monopolar coagulating current to create inflammation, and subsequent fibrosis and shrinkage, of the inferior turbinate soft tissues.Reference Woodhead, Wickham, Smelt and MacDonald6 Haemorrhage is the most common complication; this is usually self-limiting, but, rarely, severe haemorrhage requiring massive blood transfusion and arterial ligation has been reported.Reference Premachandra, Bull and Mackay7 Other complications include synechiae formation, nasal crusting and atrophic rhinitis.Reference White and Murray8 Sequestration of the inferior turbinate requiring surgical debridementReference Williams, Fisher and Golding-Wood2 and extensive bony necrosis has been reported in the literature.Reference Keh, Shakeel, Chapman and Maini9
The endoscopic photographs of this case suggest that there has been more than just a mucosal response to submucosal diathermy, and indicate probable sequestration and shedding of part of the inferior turbinate itself. Whilst fibrosis of the tissues at the lower end of the nasolacrimal duct could be expected to lead to stenosis of the nasolacrimal duct stoma and obstructive epiphora, in this case the post-procedural scarring has resulted in the destruction of the valve of Hasner and an unusual patulous, valveless opening to the lower nasolacrimal duct, with free communication between the nasal cavity and the lacrimal sac.
Computed tomographic dacryocystographyReference Waite, Whittet and Shun-Shin10 can prove helpful in providing anatomical and structural details, relating the site of nasolacrimal obstruction to nasal and sinus pathology and anatomical variation. In this case, it confirmed the clinical impression of an exaggerated patency of the nasolacrimal apparatus following the scarring effects of surgery to the inferior turbinate bone.
This communication appears to have led to the free retrograde reflux of both air and mucus from the nasal cavity directly to the surface of the eye. This effect is similar to that which may occasionally occur following dacryocystorhinostomy, or more commonly following canalicular bypass procedures, where a direct communication is deliberately created to overcome nasolacrimal obstructive symptoms.Reference Biro, Murchison, Pribitkin, Rosen and Bilyk11
• Submucosal diathermy to the inferior turbinate is a frequently performed procedure for hypertrophied inferior turbinate, with minimal complications
• Submucosal diathermy can cause troublesome scarring around the nasolacrimal duct opening
• Patulous nasolacrimal duct stoma with reflux of air and mucus on to the ocular surface is a newly recognised complication of submucosal diathermy
• This complication should be considered in pre-operative discussion
Conclusion
To our knowledge, there have been no previous reports of a symptomatic patulous nasolacrimal duct stoma following submucosal diathermy to the inferior turbinate. This novel complication therefore provides a further reminder of the potential for nasolacrimal drainage system complications and of the importance of a considered pre-operative discussion.
Competing interests
None declared




