Introduction
Written communication used in varying forms plays a key role in extending the work done in many psychological therapies (Bolton, Reference Bolton2004). Although initially attributed to narrative therapy (Parry and Doan, Reference Parry and Doan1994; White and Epston, Reference White and Epston1990), therapeutic letters are now more formally recognized for their use in cognitive analytical therapy (CAT) (Ryle and Kerr, Reference Ryle and Kerr2003; Ryle et al., Reference Ryle, Bolton, Howlett, Lago and Wright2004), but are also used in cognitive and behavioural (Schmidt et al., Reference Schmidt, Wade and Treasure2014; Tchanturia and Hambrook, Reference Tchanturia and Hambrook2010), family (Bacigalupe, Reference Bacigalupe1996; Wojcik and Iverson, Reference Wojcik and Iverson1989) and individual psychodynamic therapies (Ingrassia, Reference Ingrassia2003). Goodbye letters, written by the therapist to the patient, are typically shared in the penultimate therapy session (Denman, Reference Denman2001).
Despite their use in clinical practice, there is surprisingly little research on how goodbye letters may relate to treatment outcomes and/or the qualities that make goodbye letters useful. In the only study investigating the key components of goodbye letters, Turpin et al. (Reference Turpin, Adu-White, Barnes, Chalmers-Woods, Delisser, Dudley and Mesbahi2011) identified 17 ‘ingredients’ that ought to be included in therapist written goodbye letters, based on questionnaire responses from 18 trainee CAT therapists. The ingredients were concerned with both the content and structure of the letters, as well as the style in which they should be written. Although attempts have been made to develop an audit tool for the rating of patient written goodbye letters in CAT (McCombie and Petit, Reference McCombie and Petit2011), no standardized tool currently exists for assessing the quality of therapists’ written goodbye letters. The lack of quantitative research examining the impact of goodbye letters on therapeutic outcomes may then be in part due to the absence of both empirically based guidance on how to write goodbye letters, and standardized tools to assess their quality.
Findings from a small body of qualitative research do provide anecdotal evidence for the use of goodbye letters, with semi-structured interview studies suggesting that goodbye letters are generally well received by patients and have a positive impact when used as part of psychodynamic interpersonal therapy with imprisoned women (n = 13; Walker et al., Reference Walker, Shaw, Turpin, Roberts, Reid and Abel2016) and with patients with irritable bowel syndrome (n = 5; Howlett and Guthrie, Reference Howlett and Guthrie2001). When used in CAT for patients with depression (n = 8), therapist and patient written goodbye letters were experienced both positively and negatively by participants (Hamill et al., Reference Hamill, Ried and Reynolds2008). Goodbye letters facilitated reflection on the therapy process and marked the termination of therapy. In a study involving nine patients who had received CAT for a variety of presenting problems, participants found goodbye letters useful in documenting their progress (Rayner et al., Reference Rayner, Thompson and Walsh2011). In a study exploring 17 patients’ experiences of receiving psychological therapy for anorexia nervosa (AN), all participants who received goodbye letters considered them to be personal and felt that they provided a helpful summary that could be shared with others (Lose et al., Reference Lose, Davies, Renwick, Kenyon, Treasure and Schmidt2014). Participants made reference to the clear and succinct nature of letters and their ability to put 20 weeks of therapy into perspective. These studies suggest that most patients find goodbye letters useful, with only a minority of patients, most of whom experienced difficulties with the therapy overall, reporting a negative experience.
In the absence of evidence supporting a preferred psychological treatment for adults with AN and suboptimal outcomes of psychological therapy for AN (Zipfel et al., Reference Zipfel, Giel, Bulik, Hay and Schmidt2015; Brockmeyer et al., Reference Brockmeyer, Friederich and Schmidt2017; NICE, 2017), increasing attention is being paid to the specific components of therapy that may be beneficial or detrimental to the treatment process. Recently, our group investigated associations between the quality of case formulation letters and treatment outcomes in patients with AN treated with Maudsley Anorexia Nervosa Treatment for Adults (MANTRA). A reflective writing style and attention to the development of AN were positively associated with treatment acceptability and treatment outcomes (Allen et al., Reference Allen, O’Hara, Bartholdy, Renwick, Keyes, Lose and Loomes2016). However, to date, no study has empirically investigated the impact of goodbye letters on clinical outcomes for patients with AN or otherwise.
This study aimed to examine whether the quality of goodbye letters was associated with improvements in body mass index (BMI) and eating disorder symptomology in adults with AN, taking part in a randomized controlled clinical trial of two psychological treatments for AN. A novel goodbye letter rating scheme (referred to as letter rating scheme) was developed and used to determine goodbye letter quality. ‘Quality’ was defined as total and item score ratings based on the goodbye letter rating scheme. Letters were written and given to patients at end-of-treatment, approximately 6 months post-randomization. Treatment outcomes were defined as BMI and global Eating Disorders Examination (EDE) scores at 12 and 24 months post-randomization, as well as the change in BMI and global EDE scores from 12 to 24 months. It was hypothesized that:
(1) Higher total letter quality scores would predict improvements in BMI and EDE scores at 12 and 24 months.
(2) Higher item scores would predict improvements in BMI and EDE scores at 12 and 24 months.
(3) Higher total letter quality scores would predict larger BMI and EDE change scores from 12 to 24 months.
(4) Higher item scores would predict larger BMI and EDE change scores from 12 to 24 months.
Method
Design
This was a correlational, exploratory study that used secondary data from a large multi-centre randomized controlled trial (RCT) fully described elsewhere (Schmidt et al., Reference Schmidt, Renwick, Lose, Kenyon, DeJong, Broadbent and Serpell2013; Schmidt et al., Reference Schmidt, Magill, Renwick, Keyes, Kenyon, Dejong and Yasin2015).
Participants
Participants were adult out-patients (aged 18–60 years) with broadly defined AN (body mass index ≤18.5 kg/m2) who took part in The Maudsley Outpatient Study of Treatments for Anorexia Nervosa and Related Conditions (MOSAIC), a large RCT (n = 142) evaluating first-line psychological treatments for adult out-patients with AN. This RCT compared MANTRA (Schmidt et al., Reference Schmidt, Wade and Treasure2014) to Specialist Supportive Clinical Management (SSCM) (McIntosh et al., Reference McIntosh, Jordan, Bulik, Grilo and Mitchell2010). For full details on inclusion and exclusion criteria, see the study protocol (Schmidt et al., Reference Schmidt, Renwick, Lose, Kenyon, DeJong, Broadbent and Serpell2013).
MANTRA and SSCM are both individual psychotherapies that involve 20–30 weekly sessions and four monthly follow-up sessions. Participants were randomly allocated to receive either SSCM or MANTRA and attended five research assessments: at baseline (pre-randomization), at 3 months (mid-treatment), at 6 months (end of treatment) and at 12 and 24 months (follow-up) post-randomization. Data from baseline and 12- and 24-month follow-up sessions were used in the current study.
Eligible participants in the present study were the 72 patients who were allocated to receive MANTRA plus one patient allocated to SSCM who went on to receive MANTRA due to incompatibilities with the SSCM treatment protocol (n = 73). Analyses were conducted with 41 of these patients who completed treatmentFootnote 1 and so received a goodbye letter written from their therapist (usually in the penultimate or final few sessions); n = 41/73, 56% of the MANTRA sample.
Participant characteristics
Baseline socio-demographic and clinical characteristics for patients who did or did not receive goodbye letters (effectively those who did/did not complete treatment) were compared (see Table 1). No significant differences were found between MANTRA participants with and without goodbye letters on any of these characteristics. As expected, patients who received goodbye letters attended significantly more treatment sessions than those without goodbye letters, t (33.43) = 4.82, p < 0.001.
Table 1. Socio-demographic and clinical characteristics of MANTRA patients with and without a goodbye letter

1t-test; 2Mann–Whitney U-test.
Development of the letter rating scheme
For this research, a 7-item goodbye letter rating scheme was developed and adapted from the MANTRA-Case Formulation Rating Scheme (MANTRA-CFRS); described fully in Allen et al. (Reference Allen, O’Hara, Bartholdy, Renwick, Keyes, Lose and Loomes2016). The adaptations were to shift the focus from formulation letters to goodbye letters. As with the MANTRA-CFRS, letters were assessed for overall quality, as indicated by the total score, as well as specific aspects of structure and content, as indicated by individual item scores. Items 1a to 1c were used to rate letters for structure; including progress made, preventing setbacks and saying goodbye, respectively. Items 2a to 2d were concerned with the quality of letter content and were used to rate letters on the use of collaborative, reflective, empathic and affirming stances, respectively.
A 4-point scale was used for each of the items in the scheme, ranging from 0 (indicating no use of the item quality) to 3 (which indicates strong use). Item ratings are added together to produce a maximum total score of 21. The goodbye letter rating scheme is included in the Appendix (see Supplementary Material).
Adaptations from the MANTRA-CFRS were initially made by the authors U.S. and K.A., with other experienced eating disorders therapists then consulted. Prior to its use with patients from the RCT, the letter rating scheme was then tested on MANTRA goodbye letters written for patients who were not part of the present study, but who were seen as part of routine practice. These goodbye letters were independently co-rated by the authors J.S. and K.A. until agreement was consistently achieved. During this phase of the study, discussions led to small changes and adaptions to the letter rating scheme. A proportion (n = 10) of goodbye letters from the RCT (this study sample) were then rated independently to test the letter rating scheme for inter-rater reliability. Inter-rater reliability was high for total scores (r = 0.92, p < .05) and for individual item scores 1b to 2d (r = 0.77–1.0, p < 0.05). A trend level but non-significant association was found for item 1a (work done and progress made) (r = 0.60; 95% CI, –0.273 to 0.894; p = 0.064), suggesting that inter-rater agreement on this item was not consistently achieved. Further discussions amongst the authors informed more consistent ratings and, once the testing phase was complete, the remaining letters (n = 31) were rated by J.S.
Primary outcome measures
The outcome measures (see below) were assessed at 12- and 24-month follow-ups, and also administered at baseline.
Eating Disorder Examination (Cooper and Fairburn, Reference Cooper and Fairburn1987)
The EDE is a diagnostic interview that provides a measurement of both the severity and range of eating disorder symptoms. It has high inter-rater reliability (Cooper and Fairburn, Reference Cooper and Fairburn1987; Rosen et al., Reference Rosen, Vara, Wendt and Leitenberg1990) and internal consistency (Cooper et al., Reference Cooper, Cooper and Fairburn1989). The global score was used to give an index of eating disorder psychopathology.
Body mass index
BMI was calculated using the standard formula (weight [kg]/height [m]2).
Additional measures
Self-report questionnaires
Self-report questionnaires were used at baseline to assess psychosocial functioning. As patient characteristics may have impacted therapist effort and/or the therapeutic relationship, consideration was given to whether total scores on these measures may act as covariates in analyses. The self-report questionnaires included the Clinical Impairment Assessment (CIA; Bohn and Fairburn, Reference Bohn and Fairburn2008); Emotion Regulation Questionnaire (ERQ; Gross and John, Reference Gross and John2003); Social Comparison Scale (SCS; Allan and Gilbert, Reference Allan and Gilbert1995); Cognitive Flexibility Scale (CFS; Martin and Anderson, Reference Martin and Anderson1998); Depression Anxiety and Stress Scale (DASS-21; Lovibond and Lovibond, Reference Lovibond and Lovibond1995); Obsessive Compulsive Inventory Revised (OCI-R; Foa et al., Reference Foa, Huppert, Leiberg, Langner, Kichic, Hajcak and Salkovskis2002); and Beliefs about Emotions Scale (BES; Rimes and Chalder, Reference Rimes and Chalder2010).
Visual analogue scales
Visual analogue scales were used to examine perceived social support (two-item) and motivation to change (four-item) at baseline. Items on the social support scale assessed the closeness of participants’ relationships with others and the extent to which participants felt able to confide in others. The motivation items were concerned with participants’ perceived importance of change and ability to change (in relation to food and weight, as well as overall). Responses to both social and motivational items could range from 1 to 10 and averages were used to provide overall total social and motivational scores.
Data analysis
Descriptive analyses
Baseline socio-demographic and clinical characteristics for patients who did or did not receive goodbye letters were compared using independent t-tests when data met normality assumptions, and Mann–Whitney U-tests for non-normal data. Means, standard deviations and ranges were obtained for both total and item letter scores. Correlations between letter scores and baseline patient characteristics were then examined.
Hypothesis testing
Linear regression was used to examine associations between goodbye letter total and item scores and total BMI and global EDE scores at 12 and 24 months, respectively (hypotheses 1 and 2).Footnote 2 Changes in global EDE and BMI scores from 12 to 24 months were calculated and simple linear regression was used to investigate associations between both goodbye letter total and item scores and EDE and BMI change scores (hypotheses 3 and 4). Multiple regression was used to examine associations between goodbye letter total and item scores and total BMI and global EDE scores when significant additional predictors were identified. Baseline as opposed to 6-month EDE and BMI scores were considered as potential additional predictors as letters were written at approximately 6 months, with some letters written before or after this time point.
For all analyses, an alpha of p < 0.05 was used. The decision to use an unadjusted value was based upon the potential significance of any findings given the limited evidence on the use of goodbye letters, as well as the relatively small sample size used in this study. Although the risk of type 1 error was increased, this decision increased the probability that factors that influence AN treatment outcomes would be found.
Results
Quality of goodbye letters
Means, standard deviations and ranges for goodbye letter total and item scores are given in Table 2. High mean scores suggest that therapists mostly adhered to the MANTRA model when writing goodbye letters. The mean score for item 2c (affirming stance) was highest, suggesting that affirming statements were present in a large proportion of goodbye letters.
Table 2. Means, standard deviations, ranges, skewness and kurtosis of letter rating scheme total and item scores
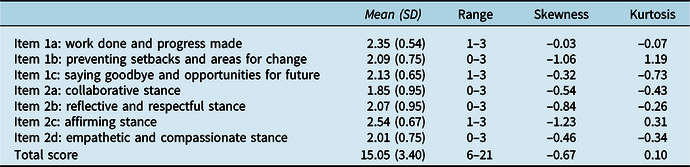
Items 1a to 2d have possible score ranges from 0 to 3, and total scores can range from 0 to 21.
Correlations between total and item scores
Pearson’s correlation was used to check for correlations when data for both variables met the assumption of normality, whereas Spearman’s correlation was used to check for correlations when data for both variables were not normally distributed. As expected, total letter scores correlated positively and significantly with individual item scores (r = 0.47–0.79, p < 0.01) except for item 1a (work done and progress made) which although it showed a slight positive correlation, was not significant (r = 0.261, p = 0.099).
Correlations between total scores and baseline characteristics
Total letter scores did not correlate significantly with baseline scores on the DASS, CIA, CFS or the OCI-R (p > 0.05) as shown in Table 3. A significant negative correlation was found between the total letter and SCS scores (r = –0.33, p = 0.04). The SCS provides a measure of how participants consider themselves in comparison with others, with higher scores indicating feelings of superiority and lower scores indicating feelings of inferiority. This suggests that higher quality letters were written for patients who considered themselves as more inferior to others. Total scores significantly and positively correlated with BES scores (r = 0.36, p = 0.019). Higher scores on the BES indicate stronger beliefs about thoughts and feelings being unacceptable. This suggests that therapists wrote higher quality goodbye letters for patients who held stronger beliefs that emotions are unacceptable. A significant negative correlation was found between total scores and overall social support scale scores (r = –0.38, p = 0.016), suggesting that higher quality letters were written for patients with lower perceived social support.
Table 3. Correlations between goodbye letter total and item scores and patient baseline psychosocial characteristics
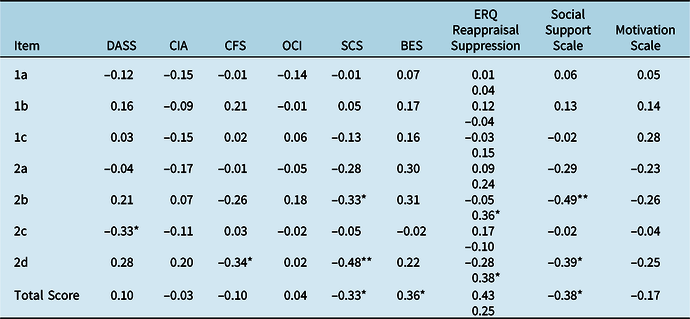
*p < 0.05, **p < 0.01.
Correlations between item scores and baseline characteristics
Higher scores on items 2b and 2d (reflective and empathetic stances) correlated significantly and negatively with overall social support scale scores (r = –0.49, p = 0.001 and r = –0.39, p = 0.013), suggesting that more reflective and empathetic statements were used in letters written for patients who had lower perceived social support.
Higher scores on items 2b and 2d also correlated significantly and negatively with SCS scores (r = –0.33, p = 0.04 and r = –0.48, p = 0.002), suggesting that therapists adopted more reflective and empathic positions in letters written for patients who considered themselves negatively in comparison with others.
In addition, scores on items 2b and 2d correlated positively and significantly with scores on the suppression scale of the ERQ (r = 0.36, p = 0.022 and r = 0.38, p = 0.014), suggesting that more reflective and empathetic statements were used in letters written for patients who supressed their emotions.
Scores on item 2d correlated negatively and significantly with CFS scores (r = –0.34, p = 0.031). As higher scores on the CFS indicate better cognitive flexibility, this suggests that therapists adopted more empathetic stances in letters written for patients who had lower cognitive flexibility skills.
Higher scores on the item 2c (affirming stance) correlated significantly and negatively with total scores on the DASS (r = –0.33, p = 0.035). As higher scores on the DASS are indicative of higher levels of depression, anxiety and stress, this suggests that more affirming statements were used in letters written for patients who reported lower levels of depression, anxiety and stress.
Descriptive statistics for total BMI and EDE at 12 and 24 months
Mean BMI increased from 17.82 (SD = 1.79) to 18.37 (SD = 2.09) from 12 to 24 months, and mean EDE scores decreased from 2.17 (SD = 1.43) to 2.08 (SD = 1.33) during these time periods.
Descriptive statistics for EDE and BMI change scores from 12 to 24 months
Change in BMI and global EDE scores from 12 to 24 months were computed by subtracting 12-month scores from 24-month scores. The mean BMI change score was 0.36 (SD = 1.11) and the mean EDE change score was –0.005 (SD = 0.71).
Correlations between EDE and BMI scores at 12 and 24 months
Total BMI and EDE scores at 12 months were not significantly correlated (r = –0.17, p = 0.310) nor were total BMI and EDE scores at 24 months (r = –0.11, p = 0.539).
Hypothesis testing
Hypothesis 1
As BMI at baseline was a significant predictor of BMI at 12 months (β = 0.507, 95% CI: 0.092, 0.922; p = 0.018), it was included in the regression models testing effects of goodbye letter scores on 12-month BMI. This model was significant [F (2,35) = 5.469, p = 0.009] and total letter scores were significantly associated with BMI at 12 months after the adjustment for baseline BMI (β = 0.170; 95% CI: 0.003, 0.337; p = 0.047). Every one unit increase in total letter score was associated with a 0.17 increase in BMI score at 12 months. BMI at baseline and total letter scores explained 23.8% of the variance in BMI scores at 12 months.
As no significant associations were found between total BMI scores at 12 months and scores on either the BES (β = –1.784; 95% CI, –0.048, 0.048; p = 0.999), SCS (β = –0.002; 95% CI, –0.035, 0.031; p = 0.905) or social support scale scores (β = –0.127; 95% CI, –0.399, 0.146; p = 0.351), they were not included as additional predictors in the model.
Non-significant associations were found between total letter scores and BMI scores at 24 months (β = 0.108; 95% CI, –0.127, 0.344; p = 0.356) and between total letter scores and global EDE scores at both 12 (β = 0.039; 95% CI, –0.107, 0.186; p = 0.591) and 24 months (β = 0.035; 95% CI, –0.119, 0.189; p = 0.646), with the pattern of results not altered by adjustment for baseline variables.
Hypothesis 2
In a multiple regression, where BMI at baseline was adjusted for, item 2c (affirming stance) remained a significant predictor of BMI scores at 12 months [F (2,35) = 7.107, p = 0.003]. Controlling for BMI scores at baseline showed a significant adjusted association between item 2c scores and BMI at 12 months (β = 0.1057; 95% CI, 0.249, 1.866; p = 0.012). Every unit increase in item 2c scores predicted a 1.057 increase in BMI scores at 12 months. BMI at baseline and item 2c scores accounted for 28.9% of the variance in BMI scores at 12 months.
Although scores on the DASS were significantly and negatively correlated with scores on item 2c, no association was found between DASS total scores and BMI at 12 months (β = 0.056; 95% CI, –0.067, 0.189; p = 0.393), and as such, DASS total scores were not included as an additional predictor. No other item scores were significant in predicting 12- or 24-month BMI scores.
As EDE at baseline was a significant predictor of EDE scores at 12 months (β = 0.816; 95% CI 0.653, 0.979; p < 0.001), it was included as a predictor of 12-month EDE scores alongside letter item scores. No item scores predicted EDE scores significantly at 12 or 24 months once baseline EDE scores were accounted for, although item 1b (preventing setbacks and identifying areas for change) did significantly predict 12-month EDE scores when not adjusting for baseline values (p = .026).
Hypothesis 3
There was no statistically significant relationship between total letter scores and BMI change scores (β = –0.002; 95% CI, –0.144, 0.141; p = 0.980) or total letter scores and EDE change scores (β = –0.006; 95% CI, –0.097, 0.086; p = 0.901).
Hypothesis 4
Item scores were not significant in predicting BMI or EDE change scores.
Discussion
This study aimed to determine whether higher quality goodbye letters were associated with treatment outcomes for adult out-patients with AN who had received MANTRA. Hypothesis 1 was partly confirmed as higher quality goodbye letters (total scores) were significantly associated with BMI at 12 months. However, the significance of this association was not maintained at 24 months, nor found between the overall quality of goodbye letters and reductions in EDE scores at 12 or 24 months. Hypothesis 2 was also partly confirmed, as letters that had a stronger use of an affirming stance (item 2c) were associated with higher BMI scores at 12 months. Letters that paid more attention to preventing setbacks and identifying areas for change (item 1b) showed a significant unadjusted association with BMI scores at 12 months. However, after BMI at baseline was controlled for, this association was no longer significant. No other item scores were significantly associated with increases in either BMI or EDE scores at 12 or 24 months. Hypotheses 3 and 4 were not supported, with letter scores not predicting changes in BMI or EDE from 12 to 24 months.
The finding that higher quality goodbye letters were associated with greater increases in BMI at 12 months suggests that paying attention to the overall quality of goodbye letters, including both the structure and style of the letter, may be associated with benefits that extend beyond the end of therapy and impact longer term treatment outcomes for patients with AN. These results are in line with qualitative findings from patients and therapists that attest to the multiple benefits of goodbye letters used in MANTRA (Lose et al., Reference Lose, Davies, Renwick, Kenyon, Treasure and Schmidt2014; Waterman-Collins et al., Reference Waterman-Collins, Renwick, Lose, Kenyon, Davies, Serpell and Schmidt2014), CAT (Hamill et al., Reference Hamill, Ried and Reynolds2008; Rayner et al., Reference Rayner, Thompson and Walsh2011) and PIT (Walker et al., Reference Walker, Shaw, Turpin, Roberts, Reid and Abel2016). Although findings from these studies suggest that goodbye letters are valued for a number of different reasons, until now links between goodbye letters and treatment outcomes at follow-up had not been identified. Given the time and effort required to write goodbye letters (Howlett and Guthrie, Reference Howlett and Guthrie2001; Waterman-Collins et al., Reference Waterman-Collins, Renwick, Lose, Kenyon, Davies, Serpell and Schmidt2014), these findings may provide some assurance that the time spent is worthwhile, although further research is needed to confirm this.
The mechanisms by which goodbye letters impact treatment outcomes at follow-up may be understood when considering findings of the study by Howlett and Guthrie (Reference Howlett and Guthrie2001). Here, 12 months after treatment end, patients reported that goodbye letters ‘could be used to keep the therapy and therapist alive once the sessions were over’. This suggests that letters may reflect latent constructs such as the therapeutic process or the interpersonal qualities of the therapists themselves, and help patients to remember treatment content beyond the end of regular sessions. In this respect, goodbye letters may also serve as a helpful tool in assessing, or at the very least, gaining a sense of, the overall quality of therapy.
The non-significant relationship between overall letter quality and BMI at 24 months may be explained by a number of factors. It is possible that the effects of goodbye letters, or the qualities that they represent, wane over time, perhaps representing reductions in motivation due to patients no longer being actively involved in therapy. Importantly, findings show that for MANTRA patients, improvements in both BMI and eating disorder symptomology are either maintained or improve at 24 months (Schmidt et al., Reference Schmidt, Ryan, Bartholdy, Renwick, Keyes, O’Hara and Dejong2016). Thus, our pattern of results may not reflect a deterioration in symptoms after 12 months but rather, a shift in how letter quality relates to outcomes over time. Although letters may be associated with BMI improvements at 12 months, other factors may predict longer term outcomes, such as relationships or experiences that develop after therapy ends.
It is interesting that overall letter quality did not predict EDE scores at either 12 or 24 months. It could be that overall letter quality (and possibly, the overall quality of MANTRA therapy) may have a more profound impact on weight gain as opposed to eating disorder symptomology. It is certainly established that, while BMI and eating disorder symptoms both improve with effective therapy, the degree to which these symptoms change together is variable, with improvements in BMI not necessarily being associated with concurrent improvements in EDE scores (and vice versa) (Byrne et al., Reference Byrne, Wade, Hay, Touyz, Fairburn, Treasure and Fursland2017; Schmidt et al., Reference Schmidt, Ryan, Bartholdy, Renwick, Keyes, O’Hara and Dejong2016). Similarly, in this study, BMI and EDE scores at 12 and 24 months were not significantly correlated. The possibility that different treatment components predict improvements in BMI relative to EDE scores deserves further research attention.
Only one item, affirming stance, was significantly associated with increases in BMI at 12 months. This suggests that using an affirming tone to connote positive changes at the end of treatment, both in goodbye letters or during the treatment process in general, may be particularly important in influencing weight outcomes after treatment for patients who have received MANTRA. The use of an affirming stance is an explicit part of the motivational style of MANTRA (Treasure and Schmidt, Reference Treasure and Schmidt2013). Interestingly, findings from recent process evaluation studies suggest that patients significantly prefer MANTRA to SSCM (Schmidt et al., Reference Schmidt, Magill, Renwick, Keyes, Kenyon, Dejong and Yasin2015) with patients finding MANTRA’s focus on cognitive interpersonal factors, rather than nutrition, helpful in their recovery process (Zainal et al., Reference Zainal, Renwick, Keyes, Lose, Kenyon, DeJong and Johnson-Sabine2016). Findings from the present study suggest that some aspects of the MANTRA motivational style may continue to influence treatment outcomes beyond the end of therapy. Specifically praising effort rather than performance, as outlined in the affirming stance item in the letter rating scheme, is supported by research on the ‘Growth Mindset’ theory, with findings showing that in children and young people praising effort rather than performance leads to greater achievement and better outcomes (Kamins and Dweck, Reference Kamins and Dweck1999). It is interesting to note that in formulation letters, a reflective and respectful tone was associated with later improvements in eating disorder symptomology (Allen et al., Reference Allen, O’Hara, Bartholdy, Renwick, Keyes, Lose and Loomes2016). Thus, different aspects of the therapeutic style may be useful at different times during the therapeutic process. This finding should also be considered in relation to the correlational findings between baseline patient characteristics and item scores. More affirming statements were used for those patients who had lower levels of depression, anxiety and stress at baseline. As increases in BMI at 12 months may also be influenced by lower anxiety, depression and stress symptomology at baseline, these findings should be interpreted with some caution.
It is perhaps to be expected that neither total nor item letter scores were significantly associated with changes in BMI and EDE from 12 to 24 months, as findings from a number of studies show that BMI increases most rapidly during and shortly after therapy, before subsequently decelerating over longer follow-up periods (Schmidt et al., Reference Schmidt, Ryan, Bartholdy, Renwick, Keyes, O’Hara and Dejong2016). Change scores then reflected minimal and for some no change over the period of 12 to 24 months, making a significant linear relationship more difficult to detect.
Correlations between baseline characteristics and goodbye letter scores suggested that higher quality letters were written for patients who considered themselves more inferior to others, held stronger beliefs that emotions are unacceptable and had lower perceived social support. More reflective and empathic statements were used in letters to patients who considered themselves negatively in comparison with others, had lower perceived social support and suppressed their emotions. More empathic stances were used in letters to those who had lower cognitive flexibility skills. Conversely, more affirming statements were used in letters to patients who reported lower levels of depression, anxiety and stress. These findings suggest that goodbye letters are written with the individual characteristics of the patient in mind, and that therapists may try to ‘match’ their language and style to these characteristics. Therapists may use reflective, empathic language as part of their attempt to support and connect with patients presenting with higher levels of psychosocial difficulties, and may use more affirming statements for patients with marked depressive or anxiety symptoms who may be unable to hear these. Further research is needed to explore these themes further.
The results of this study must be interpreted with respect to several limitations. First, as an exploratory study with multiple hypotheses, there is an increased chance of a type 1 error. However, as the first quantitative study investigating the impact of goodbye letters, these results can be considered as a starting point for future research. Replication is needed in another AN sample who have received MANTRA. Secondly, there may be a number of confounding predictors that influence treatment outcomes for patients with AN that were not controlled for in this study. In order to isolate letter effects, future research may benefit from giving consideration to additional variables (e.g. illness severity and duration, psychiatric co-morbidity and age) that may influence treatment outcomes, although this study did try to consider confounders at baseline. Third, the sample size was small and patients who did not complete MANTRA could not be included in analyses. Fourth, this study did not include a comparison group (e.g. MANTRA patients with and without letters) which prevented firm conclusions from being made about the effects of goodbye letters on outcomes. As letters are a core part of MANTRA, and are not routinely written as part of other psychological treatments for AN, including a comparison group would require adapting usual therapy protocols so as to more clearly assess the impact of therapist letters. Conversely, strengths of the study include development of a novel letter rating scheme with attention to inter-rater reliability, an extended follow-up period, and attention to baseline covariates.
The findings from this research provide evidence for the therapeutic benefits of therapist written goodbye letters used as part of MANTRA in the treatment of AN. For this sample of patients with AN, both the overall quality of goodbye letters and the use of an affirming stance specific to MANTRA were associated with improvements in BMI at 12 months post-randomization. However, neither the overall quality nor the style of goodbye letters predicted improvements in BMI at 24 months, or reductions in eating disorder symptomology at either 12 or 24 months post-randomization. Findings from this study suggest that it may be important for therapists to pay attention to the overall quality as well as the specific style of goodbye letters, but additional research is needed to replicate these findings.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1352465820000089
Acknowledgements
The authors are grateful to the participants and therapists who took part in the trial from which these data were collected.
Financial support
This project was supported by a National Institute for Health Research (NIHR) Programme Grant for Applied Research (RP-PG-0606-1043) and an NIHR Research for Patient Benefit (RfPB) grant (PB-PG-0613-31050). Ulrike Schmidt is supported by a National Institute of Health Research (NIHR) Senior Investigator Award. She receives salary support from the NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Ethical statements
Ethical approval for the study was obtained from National Research Ethics Service, NHS REC (reference no. 10/H0714/9), Central London REC 4 and Royal Free Hospital, London. The authors state that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, and its most recent revision.






Comments
No Comments have been published for this article.