Introduction
Patient safety is one of the most vital and critical challenges facing the health care system. The concept of patient safety is the prevention of damage to the patient in care systems, prevention of human and systematic errors, learning from previous mistakes, and developing a patient safety culture among health care providers, systems, and patients.Reference Bost, Crilly, Wallis, Patterson and Chaboyer 1 , Reference Dojmi Di Delupis, Mancini, Di Nota and Pisanelli 2
Nowadays, Emergency Medical Services (EMS) staff, due to having first contact with emergency patients, have a vital role in the health care system; EMS staff are able to consider the principles of handover, prevent medical systems errors, and prevent damage to patients. Improving patient safety and health care quality is placed at the core of their professional activities.Reference Bost, Crilly, Wallis, Patterson and Chaboyer 1 One of the key components in improving patient safety is continuity in patient care. Delivery of the patient from EMS staff to the emergency department (ED) is now a global initiative to promote continuity in health care.Reference Lally 3 Benson et al mention that patient handover is a process of sharing information in order to ensure the safety and continuity of care quality for patients according to different standards.Reference Benson, Rippin-Sisler, Jabusch and Keast 4 As the patient is transferred between EMS staff and the ED, the transfer of updated, complete, and accurate information is essential.Reference Lally 3
Communication during patient handover between health care providers may not contain all the necessary data or some information may not be well understood. These gaps in communication can cause serious damage in continuity of care and cause potential risks for patients. Correct information transfer in health care systems is a critical component in the continuing safety health care for patients.Reference Strople and Ottani 5 , Reference Vidyarthi, Arora and Schnipper 6 In the field of emergency care, data associated with patient’s heart and breathing are essential. Safety Committee of USA said the poor transfer of information is the leading cause of 65% of irrecoverable events and 90% of the underlying cause.Reference Singer and Dean 7
Proper information transfer is perquisite to prevention of many medical errors and ensures high quality of health care. Knowing what information needs to be communicated is one of the issues that causes serious challenges to patient handover in the ED. Since a part of patient care’s time is dedicated to the handover, data delivery processes in emergency cases should include necessary data, relevant to patient care according to the patient’s conditions and needs, which ensures the safety and high quality of patient health care.Reference Strople and Ottani 5 Transferring of more or less data, information of low quality, not enough time for questions and answers, the lack of a standard tool for handover, and harassment during handover are several obstacles to providing an effective handover; therefore, these items are contained in the standard handover tools.Reference Horwitz, Moin and Krunholz 8 , Reference Welsh, Flanagan and Ebright 9
Patient handover is a global concern because there is currently no standard and effective way to improve communication during patient handover. Different strategies have been implemented and are being studied, one of which is the framework designated by the acronym “ISBAR.” The Identify, Situation, Background, Assessment, and Recommendation (ISBAR) tool may improve safety in handover by providing a template which creates a clear picture of the patient’s clinical issues while also defining outstanding issues and tasks. It aids communication by offering an expected pattern of transferred information so errors or omitted information become clear. Studies on ISBAR have shown that it can have a substantial impact on improving the quality of handover. It is a well received, easy to remember tool and has been shown to reduce rates of adverse events.Reference Hohenhaus, Powell and Hohenhaus 10 , Reference Woodhall, Vertacnik and McLaughlin 11
Currently in Iran, the majority of patient handovers and transfers of the necessary information in the ED are carried out orally and using a sheet, without following a standard instruction. In the current study, the ISBAR tool for improvement of patient handover is taught to EMS staff and Emergency Medicine Assistants (EMAs) in the ED. The situation of handover before and after ISBAR training is audited.
Methods
This is a clinical audit which was carried out in Imam Hossein Hospital, affiliated to Shahid Beheshti University of Medical Sciences, Tehran, Iran during 2016. The handover of trauma patients between EMS staff and EMAs in the ED was surveyed. The ISBAR tool was selected for this study ahead of other handover tools as it is the most extensively studied.Reference Thompson, Collett and Langbart 12
Study Setting
Imam Hossein Educational Hospital is a governmental hospital located in the center of Iran (City of Tehran), was founded in March 1985, which was later affiliated to Shahid Beheshti University of Medical Sciences. Imam Hossein Hospital had been very active in rendering services to the war-front combat troops during the 8-year imposed war with the Iraqi forces. Currently, Imam Hossein Hospital is a 570-bed educational and general medical/surgical referral hospital with 59,000 m2 area and includes: general surgery, internal medicine, pediatrics, obstetrics and gynecology, neurology, infectious diseases, neurosurgery, ophthalmology, orthopedics, oncology, radiology, emergency, psychiatric, dialysis, and pathology wards, as well as intensive care unit/ICU, neonatal intensive care unit/NICU, coronary care unit/CCU, operating rooms, clinics, and a clinical laboratory. The ED of Imam Hossein Hospital is one of the most active and crowded wards, which admits approximately 6,000 cases per month. In this department, EMAs were trained for a 3-year period, and annually approximately 50 emergency specialists are graduated. It’s worth noting that training of EMAs was initiated in 2000 in Iran, and this hospital was one of the pioneer hospitals. Only men can be a member of EMS in Iran, which their education is limited to EMS (with two or four years training in the Medical Universities), nursing, and rarely general physician. In Iran, people call 125 for ambulance and EMS; EMS staff bring emergency patients to the ED and deliver to residency EMAs.
Phases of Study
The study was divided into three phases, as follows:
Phase 1: Collection of pre-ISBAR baseline data (Weeks 1-4). In the first four weeks of the clinical term, baseline data of 178 patient handovers between EMS staff and EMAs were collected in a subtle manner by an emergency medicine specialist according to the ISBAR tool.
Phase 2: Education session (Weeks 5-8). In Phase 2, participants attended a 1-hour education session focusing on the importance of effective handover and the use of the ISBAR communication tool. The education session was held at eight separate times (each session lasted 20 minutes) to maximize EMS staff and EMA attendance. A pamphlet was provided to those who attended the session. Each session was conducted by the director of the ED at Imam Hossein Hospital, assisted by two study authors. Participants were given two weeks to gain familiarity and proficiency with the ISBAR tool and were encouraged to use the ISBAR tool at handover meetings.
Phase 3: Collection of post-ISBAR data (Weeks 9-12). In Phase 3, after training in ISBAR tools, the clinical handover between EMS staff and EMAs for 168 trauma patients admitted to the ED was audited in a subtle manner by an emergency medicine specialist according to the ISBAR tool.
Study End Points
The primary study endpoints were recorded by chart review, including change in perception of structure and consistency of handover, confidence in the handover process, and EMS staff and EMA impression on patient care and safety. The items of this chart review were prepared based on the ISBAR standards, and two researchers were completing this chart by attending the handover process location.
Statistical Analysis
Statistical analyses were done by using the program SSPS version 18.0 (SPSS, Inc.; Chicago, Illinois USA). The pre-ISBAR and post-ISBAR surveys were analyzed with a Mann-Whitney U and chi-square tests to establish any change in handover. Because all quantitative parameters according to the Kolmogorov-Smirnov test had normal distributions, independent t-test was used for comparison of continuous parameters between Phase 1 and Phase 3. The results are expressed as a mean (standard deviation [SD]) and number (percent). P values less than .05 were considered statistically significant.
Ethical Consideration
The study followed the principles of the Declaration of Helsinki and was approved by the Medical Ethics Review Board of Shahid Beheshti University of Medical Sciences. The confidentiality and anonymity of collected data were guaranteed. Doing this study, diagnosis and treatment of trauma patients was not impaired.
Results
In the first four weeks of the clinical term (Phase 1), baseline data of 178 patient handovers between EMS staff (n=150) and EMAs (n=150) were collected. Some who participated in 178 handovers in Phase 1 and Phase 3 were the same. Also, it’s worth noting that in Iran, only men can be a member of EMS staff. Due to some incomplete data, 150 handovers were included in the analysis.
In Phase 2, all EMS staff and EMAs affiliated to Imam Hossein Hospital formally attended the education session.
In Phase 3, after ISBAR training, the clinical handover between EMS staff and EMAs for other 168 trauma patients admitted to the ED was audited. Complete data for 150 handovers were analyzed.
Demographic data of EMS staff, EMAs, and trauma patients is shown in Table 1. There were no significant differences between Phase 1 and Phase 3 regarding demographic data. It was noticeable that in Phase 1 and Phase 3, all trauma patients were transferred to the hospital by ambulance.
Table 1 Demographic Data of EMS Staff, EMAs, and Trauma Patients
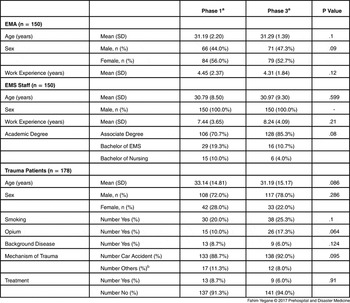
Abbreviations: EMA, Emergency Medical Assistant; EMS, Emergency Medical Services; ISBAR, Identify, Situation, Background, Assessment, and Recommendation.
a Phase 1: Pre-ISBAR baseline data (Weeks 1-4); Phase 3: Post-ISBAR data (Weeks 9-12).
b Others: Falling, Stabbed, Gun Bullet, Struggle.
Detailed data on “Identify” before and after the education session about the ISBAR tool is demonstrated in Table 2. Presenting of the patient’s name and age significantly increased after receiving education about the ISBAR tool.
Table 2 Data on “Identify” Items Before and After Education Session about ISBAR Tool Handover

Abbreviations: EMA, Emergency Medical Assistant; ISBAR, Identify, Situation, Background, Assessment, and Recommendation.
a Phase 1: Pre-ISBAR baseline data (Weeks 1-4); Phase 3: Post-ISBAR data (Weeks 9-12).
Detailed data on “Situation” before and after the education session about the ISBAR tool is shown in Table 3. Presenting of reason for the emergency call and the possible changes that occurred in the patient’s condition in comparison to the scene significantly increased after receiving education about the ISBAR tool by the prehospital team leader.
Table 3 Data on “Situation” Items Before and After Education Session about ISBAR Tool Handover

Abbreviations: EMA, Emergency Medical Assistant; ISBAR, Identify, Situation, Background, Assessment, and Recommendation.
a Phase 1: Pre-ISBAR baseline data (Weeks 1-4); Phase 3: Post-ISBAR data (Weeks 9-12).
Detailed data on “Background” before and after the education session about the ISBAR tool is shown in Table 4. Presenting of the patient’s history, any home therapy, and any allergies significantly increased after receiving education about the ISBAR tool by the prehospital team leader.
Table 4 Data on “Background” Items Before and After Education Session about ISBAR Tool Handover

Abbreviations: EMA, Emergency Medical Assistant; ISBAR, Identify, Situation, Background, Assessment, and Recommendation.
a Phase 1: Pre-ISBAR baseline data (Weeks 1-4); Phase 3: Post-ISBAR data (Weeks 9-12).
Detailed data on “Assessment” before and after the education session about the ISBAR tool is shown in Table 5. Presenting the brief synopsis of treatment significantly increased after receiving education about the ISBAR tool by the prehospital team leader.
Table 5 Data on “Assessment” Items Before and After Education Session about ISBAR Tool Handover
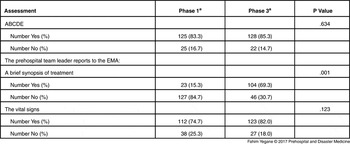
Abbreviations: EMA, Emergency Medical Assistant; ISBAR, Identify, Situation, Background, Assessment, and Recommendation.
a Phase 1: Pre-ISBAR baseline data (Weeks 1-4); Phase 3: Post-ISBAR data (Weeks 9-12).
Detailed data on “Recommendation” before and after the education session about the ISBAR tool is shown in Table 6. The EMA summarized the information received from the team leader of the prehospital team significantly more after receiving education about the ISBAR tool. It was shown that in Phase 1, none of handover followed completely the order I-S-B-A-R (0.0%), but in Phase 3, after education, 65.3 % of handover followed completely the order I-S-B-A-R.
Table 6 Data on “Recommendation” Items Before and After Education Session about ISBAR Tool Handover
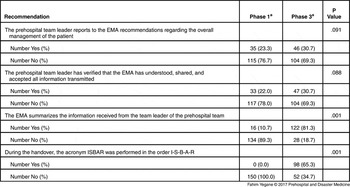
Abbreviations: EMA, Emergency Medical Assistant; ISBAR, Identify, Situation, Background, Assessment, and Recommendation.
a Phase 1: Pre-ISBAR baseline data (Weeks 1-4); Phase 3: Post-ISBAR data (Weeks 9-12).
Discussion
Clinical audit of handover in the ED in the present study showed that the ISBAR tool was not initially considered among EMS staff and EMAs in trauma patient handover. The first phase demonstrated weak handover in the ED. However, after education, there was significant improvement in handover. In other words, before education sessions, none of the handovers (0.0%) completely followed the order I-S-B-A-R, but after the education session, 65.3% of the handovers followed completely the order I-S-B-A-R. Also, in the current survey, all items of ISBAR increased after education, while 10 items had statistically significant increases. These items included:
-
∙ The patient is introduced by name;
-
∙ The patient’s date of birth is reported;
-
∙ The prehospital team leader presents the clinical situation compared to the current condition on arrival;
-
∙ The prehospital team leader reports to the EMA: the reason for the emergency call, the patient’s past history, any home therapy, or any allergies;
-
∙ The prehospital team leader reports to the triage nurse: a brief synopsis of treatment;
-
∙ The EMA summarizes the information received from the team leader of the prehospital team; and
-
∙ During the handover, the acronym ISBAR was performed in the order I-S-B-A-R.
Several factors may affect the poor handover and non-compliance with standard guidelines of the ISBAR tool. Some information may not always be available at the time of delivering patients or, alternatively, some patients may not be able to communicate fully to provide their own medical history.
While education of using a standard tool and appropriate instructions for handover can improve the delivery of essential information, there is no consensus about the exact contents of effective delivery. A number of studies have identified critical components and contents of a handover tool.Reference Hohenhaus, Powell and Hohenhaus 10 - Reference Thompson, Collett and Langbart 12 In this study, the ISBAR standard tool was used to ensure the delivery of high quality of handover.
Despite the availability of standardized guidelines for the safe delivery of patients during handover, a limited number of EMS staff and EMAs in this study were familiar with such instructions, and also among them, a more limited number adhered to these instructions in Phase 1. Experience in this study showed that the handover of trauma patients may be considered as “hit and miss,” which Ahmed et al also confirmed this situation.Reference Ahmed, Mehmood, Rehman, Ilyas and Khan 13 However, in this study, it is difficult to calculate the profit of improving the handover, but it is unlikely that improved handover be dangerous for patients. It’s believe that the transfer of information between clinical teams can lead to improved performance without the need for a major reallocation of resources and data. It is essential that all physicians in the ED receive all necessary information and assure that the delivery of patients is done in a comprehensive and safe manner. Quickly adapting to the standard instructions for handover and trying to routinely use these instructions can lead to continuous improvement in the quality of patient handover.
Previous studies have suggested that using a standard tool can improve patient handover quality and reduce the number of errors. A number of studies have reported that for improvement of the quality and effectiveness of health care, the handover must be done by a standard tool.Reference Arora and Johnson 14 , Reference Yee, Wong and Turner 15
Medical staff need knowledge and skills of handover to ensure the safety and effectiveness of patient delivery. This can be through formal teaching sessions and workshops.Reference Marshall, Harrison and Flanagan 16 It’s recommend that education of medical staff about the standard handovers should be carried out in the hospital. This is a useful way of promoting learning within hospital.Reference Ferran, Metcalfe and O’Doherty 17 Holding handover training sessions is an excellent opportunity for medical staff in different categories to develop communication, presentation, leadership, teamwork, and problem-solving skills.
Standard tools for patient handover should be supported by providing guarantees such as improving hospital facilities. Attendance of several medical specialty staff should be encouraged in patient handover sessions. A trained physician should be responsible for the accuracy of the information recorded on the handover sheets, while EMS staff should be responsible for the preparation and presentation of clinical data on patient handover.
Changes in delivery methods in the clinical environment may occur. These findings showed that the introduction of a standard handover tool, combined with education, can improve adherence to these tools. The lack of formality and acceptance from medical staff, without continuing education in handover, may cause the current findings to be short-lived.
Simplification, effectiveness, summarizing, and standardization of reports during handover can be used to promote accurate and effective service delivery to patients, and lack of standardization will probably have a negative impact on patient safety. Di Delupis et al analyzed 240 prehospital handovers in the ED according to the ISBAR tool. The findings showed the lack of consideration of the ISBAR tool in the ED was consistent with the current finding.Reference Lally 3 Di Delupis et al indicated that poor oral information from prehospital emergency providers to the ED is used to give the written report to the triage nurse without responsibility for information sharing.Reference Lally 3 It could be mentioned that patient handover was safely performed by transferring the clinical information in an accurate, concise, complete, specific, relevant, and timely manner.
Although in this study the implications of compliance with the ISBAR tool in patient handover was not investigated, after providing ISBAR education, a greater number of handover processes followed the standard ISBAR. Based on previous studies that observed the benefits of standard guidelines, it is suggested that standard handover in the ED ensures that accurate and complete information is delivered in all areas of patient health care, where a patient needs fast and complex health care. Previous studies have shown that patient safety delivered in compliance with standard guidelines can help patient health care and safety and facilitate continuity of information.Reference Riesenberg, Leisch and Cunningham 18
Limitations
Time pressure for health care provision and other responsibilities, resistance to change, and cultural and language differences among patients, along with working pressure, low knowledge about health and treatment, lack of financial resources and personnel, lack of knowledge about how to improve the health system, and lack of fundamental and applicable information for this project are some limitations of the current study. Although the education of the ISBAR tool improved the clinical information transmission, it cannot definitely say that any possible progress in the quality of handover has a positive effect on patient safety. The other limitation for this study is that it was conducted at a single hospital and may not have external validity.
It is recommended in future studies that the consequences of the implementation of the ISBAR on the quality of health care of patients be evaluated. It is proposed that future studies should compare different types of standard handover tools in patient safety in the ED. Due to the effectiveness of teaching, it is better to continue education in future studies to ensure more long-term impacts. It is suggested that further studies be performed with larger sample sizes and in different hospitals in Iran.
Conclusion
The current clinical audit showed that patient handover in the ED did not initially follow the ISBAR standard guideline. After providing education as pamphlets and lectures to EMS staff and EMAs, a high percentage of patient handovers were conducted in accordance with the ISBAR instructions.
Acknowledgements
The authors thank the Emergency Department, Shahid Beheshti University of Medical Sciences for facilities and technical assistance. This work was part of specialty Thesis of Emergency Medicine, which was approved and financially supported by the Vice-Chancellor of Research and Technology, Shahid Beheshti University of Medical Sciences. The authors also gratefully acknowledge the cooperation of the participating subjects, without whom this investigation would not have been possible. Finally, the authors thank Kirk Allen as a native English speaker for assistance in revising the English.








