Introduction
Issues related to the nosology of mental disorders remains at the forefront of clinical science and practice (Regier et al. Reference Regier, Kuhl and Kupfer2013; Cuthbert, Reference Cuthbert2014; Insel, Reference Insel2014). Although the identification of new ways of conceptualizing mental disorders is a topic that cuts across diagnostic categories, there has been particular interest in developing innovative classification schemes for eating disorders (EDs) (for reviews, see Keel et al. Reference Keel, Brown, Holland and Bodell2012; Wildes & Marcus, Reference Wildes and Marcus2013). Indeed, researchers have contended that there are ‘few mental disorders for which novel conceptualizations are needed more’ than for EDs (Wildes et al. Reference Wildes, Forbush and Markon2013, p. 1031). Here we present the first application of network analysis to identify ‘causal’ systemsFootnote 1 Footnote † of ED symptoms in a community-recruited sample of adults with EDs; we conclude by discussing diagnostic and treatment implications.
Limitations with categorical conceptualizations of EDs
The publication of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013) led to several improvements in ED diagnoses compared with previous editions. Specifically, binge eating disorder (BED) was recognized as an official diagnostic category and the frequency criteria for bulimia nervosa (BN) and BED were lowered, which reduced the prevalence of subthreshold diagnoses (and provided full-threshold diagnoses to more individuals who were suffering from serious, clinically significant EDs). However, as we describe below, remaining issues with current ED categorizations pose certain limitations to their validity and clinical utility.
First, one of the most common ED diagnoses is ‘other specified feeding or eating disorder’ (OSFED), which is comprised of various clinically significant ED symptom constellations. Recent studies indicate that approximately 30–60% of persons with DSM-5 EDs are diagnosed with an OSFED (Allen et al. Reference Allen, Byrne, Oddy and Crosby2013; Stice et al. Reference Stice, Marti and Rohde2013); other research indicates that it is not possible to distinguish full-threshold EDs from OSFEDs on the basis of psychosocial impairment or genetic risk factors (Fairweather-Schmidt & Wade, Reference Fairweather-Schmidt and Wade2014). As a result of relegating OSFEDs to a ‘residual’ diagnostic category, there are few studies describing its long-term course and outcome, and even fewer treatment studies (for a review of this issue, see Fairburn & Bohn, Reference Fairburn and Bohn2005).
Second, there is substantial symptom overlap across ED diagnoses. Few symptoms distinguish among ED diagnoses; thus, a change in a single symptom (e.g. weight gain or loss) can lead to a change in diagnosis [e.g. anorexia nervosa (AN) to BN or vice versa]. Finally – due to symptom overlap among EDs – diagnostic ‘migration’ is common with approximately 30–50% of individuals with an ED being diagnosed with a different ED at follow-up (Eddy et al. Reference Eddy, Dorer, Franko, Tahilani, Thompson-Brenner and Herzog2008; Castellini et al. Reference Castellini, Lo Sauro, Mannucci, Ravaldi, Rotella, Faravelli and Ricca2011; Allen et al. Reference Allen, Byrne, Oddy and Crosby2013). Taken together, these issues indicate that it may be more clinically and scientifically informative to elucidate EDs at the symptom-level (rather than at the level of predefined diagnostic groupings of disorders).
Are all ED symptoms created equally?
The DSM-5 considers ED symptoms to be interchangeable. Within each ED diagnosis, certain criteria can be met in more than one way. For example, criterion B for AN can be met if a person endorses: (1) intense fear of gaining weight or becoming fat, even though underweight; or (2) persistent behaviors that interfere with weight gain. Criterion B for BN can be met if the person engages in one (or more) of the following to compensate for binge-eating episodes at least once per week for 3 months: (1) fasting; (2) excessive exercise; (3) self-induced vomiting; (4) laxative, diuretic, enema, suppository, or syrup of ipecac use; or (5) insulin omission (for persons with diabetes mellitus) or misuse of thyroid medication. Similarly, BED requires a person to meet three out of five behavioral or cognitive symptoms associated with binge-eating episodes (criterion B).
Grouping symptoms as ‘equivalent’, for the purpose of determining whether someone meets a specific criterion for a diagnosis makes sense if the behaviors and cognitions that count toward the criterion are functionally equivalent. Yet, there are few empirical studies to indicate whether symptoms actually are similar in terms of their clinical utility, reliability and validity. Published research studies indicate that certain criterion B symptoms of BED, including: eating much more rapidly than normal (criterion B1) and eating alone because of being embarrassed by how much one is eating (criterion B4), do not load on a latent binge eating factor (Forbush et al. Reference Forbush, Wildes, Pollack, Dunbar, Luo, Patterson, Pollpeter, Stone, Bright and Watson2013). Other research indicates that these same criteria have lower reliabilities (κ) compared with other symptoms of BED (Brody et al. Reference Brody, Walsh and Devlin1994), which suggests that these symptoms are weaker than other criterion B symptoms in predicting diagnoses.
With regard to BN, Thelen et al. (Reference Thelen, Farmer, Wonderlich and Smith1991) found that self-reported laxative and diuretic use did not predict future diagnosis. These authors attributed the lack of predictive validity to the low base rates of these behaviors in their sample, and suggested that although these behaviors are rare, they are still clinically important. Recently, however, Hovrud & De Young (Reference Hovrud and De Young2015) tested a community sample of individuals with EDs, and found that nearly half of the variance in psychosocial impairment was uniquely accounted for by binge-eating frequency, weight/shape concerns and dietary restriction. Purging frequency (which included self-induced vomiting and misuse of laxatives or diuretics) and fear of ‘fatness’ were not unique predictors of impairment. Rather than suggesting that purging is an unimportant symptom, these studies highlight the possibility that certain ED symptoms may be more ‘central’ than others in terms of predicting other clinically relevant variables, such as impairment and relapse.
Trans-diagnostic models of ED psychopathology
In contrast to the DSM system, Fairburn's enhanced cognitive–behavioral model of EDs (CBT-E; Fairburn et al. Reference Fairburn, Cooper, Shafran and Fairburn2008) theorizes that overvaluation of weight, shape or their control represents the ‘core’ psychopathology shared across all EDs. In this context, the term ‘overvaluation’ refers to basing one's self-worth on one's body weight or shape, and/or ability to exert strict control over one's eating. An important feature of CBT-E is that overvaluation is theorized to lead to – and reinforce – further expressions of ED psychopathology.
Tabri et al. (Reference Tabri, Murray, Thomas, Franko, Herzog and Eddy2015) tested the theory underlying CBT-E in a large sample of individuals with EDs who were tested weekly over a 2-year period. Their findings indicated that overvaluation on a given week led to increases in non-compensatory weight-control behaviors the following week, and vice versa. The results of Tabri et al. (Reference Tabri, Murray, Thomas, Franko, Herzog and Eddy2015) were the same regardless of ED diagnosis, which provided support for the trans-diagnostic nature of the CBT-E model. These data suggested that: (1) ED symptoms function similarly across ED diagnoses, and (2) certain ED symptoms are mutually self-reinforcing.
Application of network analysis to ED psychopathology
The study of Tabri et al. (Reference Tabri, Murray, Thomas, Franko, Herzog and Eddy2015) provides insights into the temporal sequencing of two key DSM symptom clusters (‘overvaluation’ and non-compensatory weight control behaviors). However, additional studies are needed to identify patterns of interaction among symptoms across the full range of ED behaviors. Network analysis is a relatively new statistical technique that is ideally suited to understanding the dynamic interactions among psychopathological symptoms (Borsboom & Cramer, Reference Borsboom and Cramer2013). From the network perspective, individual symptoms are represented as nodes and connections are placed between symptoms that tend to co-occur, forming a web-like structure (or network) of a particular psychopathology. Symptom nodes in the network are viewed as inter-connected clusters that may or may not share an underlying, latent cause. For example, if one symptom within the network arises (e.g. prolonged fasting – which leads to increased physiological hunger drives), that symptom may activate other symptoms within the network (e.g. large eating episodes).
Network analysis is also able to test important chains of symptoms, such as those postulated in the CBT-E model. For example, ‘overvaluation’ of weight, shape or their control might directly lead to efforts to restrain one's eating (i.e. fasting), which over time leads to a negative energy balance that directly precipitates binge-eating episodes. Binge eating may, in turn, feedback to overvaluation due to actual or feared weight gain (i.e. overvaluation → fasting → binge-eating → overvaluation).
Finally, as we previously described, it appears that not all ED symptoms were created equally. Network analysis offers powerful insights into this issue by identifying the most central symptom(s), which has (have) many connections to other symptoms, and peripheral symptoms, which have few or no connections to other symptoms in the network. Because central symptoms activate many other symptom ‘nodes’ within the network, they represent symptoms that are particularly clinically important and may represent good treatment targets.
Current study
Based on our literature review and previous theoretical models of ED psychopathology, we hypothesized that symptoms that reflect body dissatisfaction or overvaluation of weight, shape or their control would represent the most impactful (central) symptoms within the ED ‘network’.
Method
Participants
Participants were recruited from the community to take part in an ongoing longitudinal study of ED psychopathology and co-morbidity course and maintenance. Participants were recruited from fliers, newspaper advertisements, bus advertisements and mass emails sent to faculty, staff and students at two large universities in the Midwest of the USA. The current study reports data from participants’ baseline (initial) study visit.
Because a goal of the larger study for which these data were collected was to test the longitudinal course of both full- and subthreshold EDs, our inclusion/exclusion criteria were intentionally broad to identify a representative community sample of individuals with EDs. Inclusion criteria were: (1) aged ⩾14 years; (2) endorsement of at least two symptoms of an ED on the Eating Disorder Diagnostic Scale (Stice et al. Reference Stice, Telch and Rizvi2000); (3) a score ⩾16 on the Clinical Impairment Assessment Questionnaire (CIA; Bohn et al. Reference Bohn, Doll, Cooper, O'Connor, Palmer and Fairburn2008) or diagnosis of a current full-threshold DSM-5 ED; and (4) body mass index (BMI) ⩾14 kg/m2. A cut score of 16 was chosen on the CIA because this score has optimal sensitivity and specificity for distinguishing ED cases from non-cases (Bohn et al. Reference Bohn, Doll, Cooper, O'Connor, Palmer and Fairburn2008). We chose 14 years as the lower age limit because the peak age of ED onset is mid-adolescence to early adulthood and EDs are rare among younger adolescents and children (Swanson et al. Reference Swanson, Crow, Le Grange, Swendsen and Merikangas2011). Exclusion criteria were assessed using a screening questionnaire, and included: (1) BMI < 14 kg/m2; (2) intellectual developmental disability, neurological disorder, or current psychosis; (3) inability to read/write fluently in English.
Participants (n = 143; 77.6% women) ranged in age from 18 to 55 years, with a mean age of 25.0 (s.d. = 7.7) years. Participants’ BMI ranged from 15.9 to 56.98 kg/m2 (mean = 27.53, s.d. = 8.2 kg/m2). Participants self-reported the following ethnic and racial identities (participants were allowed to select multiple categories): Caucasian (67.1%), Asian (15.4%), African-American (7.7%), multi-racial (5.6%), Native American or Alaskan Native (2.1%), Hawaiian or Pacific Islander (0.7%), or another race or ethnicity (3.5%); 9.1% of participants identified as Hispanic (of any race). Most participants were employed (n = 97; 67.8%) and had ⩾12 years of education (n = 142; 99.3%; note: these data were missing for one participant).
ED diagnoses were applied using DSM-5 criteria. Participants were diagnosed with the following current EDs: AN (n = 4; 2.8%), BN (n = 58; 40.6%), BED (n = 7; 4.9%), or an OSFED (n = 74; 51.7%). The mean self-reported duration of an ED was 7.80 (s.d. = 6.97) years. Few participants were receiving psychotherapy/counseling (n = 31; 27.1%) or were prescribed psychotropic medications (n = 26; 18.2%).
Procedure
The institutional review board approved all study procedures. Baseline procedures took place in person, and participants provided their written, informed consent prior to engaging in study-related procedures. Participants’ weight and height were measured using a digital scale and wall-mounted stadiometer. Interviewers were trained research clinicians with a minimum bachelor's-level education, and were supervised by the first author (K.T.F.) during weekly diagnostic consensus meetings. Interviews were audiotaped (with participants’ written permission); we randomly selected 10% of interviews that were rated by an independent research clinician to establish diagnostic reliability.
Measures
Psychiatric diagnoses
The Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-I; First et al. Reference First, Spitzer, Gibbon and Williams2007 revision) was adjusted for DSM-5 criteria to derive ED diagnoses. Inter-rater reliabilities for ED diagnoses were excellent (Conger's κ = 0.89 for AN and OSFED to κ = 0.90 for BN and BED).
Eating Pathology Symptoms Inventory (EPSI)
The EPSI is a 45-item self-report measure that was developed to comprehensively assess clinically relevant dimensions of ED psychopathology (Forbush et al. Reference Forbush, Wildes, Pollack, Dunbar, Luo, Patterson, Pollpeter, Stone, Bright and Watson2013). EPSI items reflect the frequency of various ED cognitions (e.g. ‘I wished the shape of my body was different’) and behaviors (e.g. ‘I made myself vomit in order to lose weight’). Each item is rated on a five-point Likert scale that ranges from 0 (never) to 4 (very often). The EPSI has eight factor-analytically derived scales, including: Body Dissatisfaction, Binge Eating, Cognitive Restraint, Purging, Excessive Exercise, Restricting, Muscle Building, and Negative Attitudes toward Obesity. The EPSI has demonstrated evidence for strong convergent and discriminant validity, and good-to-excellent internal consistency and test–retest reliability across a range of different samples (Forbush et al. Reference Forbush, Wildes, Pollack, Dunbar, Luo, Patterson, Pollpeter, Stone, Bright and Watson2013, Reference Forbush, Wildes and Hunt2014). Moreover, the eight-factor structure of the EPSI has replicated between Western and non-Western cultures (Tang et al. Reference Tang, Forbush and Lui2015). We chose to use the EPSI, rather than DSM-5 ED symptoms, because within the SCID-I there are numerous symptoms embedded within a single criterion. Because it is possible that certain symptoms within a DSM-5 criterion may have stronger or weaker importance in the overall network, we chose to use a better-differentiated symptom measure.
Statistical analyses
SPSS (IBM Corp., 2011) and AgreeStat (Advanced Analytics LLC, 2010) were used to compute descriptive analyses and Conger's κ, respectively. The R package qgraph (Epskamp et al. Reference Epskamp, Cramer, Waldorp, Schmittmann and Borsboom2012) was used to compute measures of centrality (see description in the next paragraph). Each ‘node’ represented one of the 45 EPSI items. We used a weighted association networkFootnote 2 that reflected the Pearson's zero-order correlation strength between pairs of items in the EPSI. A potential concern with using Pearson's correlations is that there is a possibility that they may result in biased estimates for rank-ordered (ordinal) scales. To address this concern, we reanalysed the network using the ‘cor_auto()’ function in qgraph to determine whether the assumption of multivariate normality (required for Pearson's r) was violated. Results showed that the same set of nodes was highly central regardless of correlation choice, and the interpretation of findings did not change as a result of whether Pearson's or polychoric correlations were used. We chose to use Pearson's r because this approach is consistent with recent network studies of psychopathology (Bringmann et al. Reference Bringmann, Lemmens, Huibers, Borsboom and Tuerlinckx2015; McNally et al. Reference McNally, Robinaugh, Wu, Wang, Deserno and Borsboom2015).
Following McNally et al. (Reference McNally, Robinaugh, Wu, Wang, Deserno and Borsboom2015), each correlation, or edge, represented the strength of association between two symptoms. Consistent with prior literature (McNally et al. Reference McNally, Robinaugh, Wu, Wang, Deserno and Borsboom2015), we computed the following centrality measures: strength, closeness, and ‘betweenness’. For all centrality measures, higher values reflect a node's greater importance to the network. ‘Strength’ represents the summed weights of connections to a particular node from other nodes.
‘Closeness centrality’ is defined as the inverse of the sum of distances from a particular node to all other nodes in the network. Note that ‘distance’ is the number of links (edges) that are traversed from one node to the next. Closeness centrality is an index of how ‘quickly’ information (or, in this case, ED symptomatology) flows through a network to reach a given node (Borgatti, Reference Borgatti2005). Therefore, high closeness indicates a short average distance between a given node and all other nodes in the network.
Betweenness centrality measures the number of times a node appears in the shortest path between two other nodes. A node is said to be high in betweenness centrality if it lies along many shortest paths, and a node is said to be low in betweenness centrality if it lies along few shortest paths. Manipulating (removing) nodes with high betweenness centrality would slow or halt the flow of information through the network (Borgatti, Reference Borgatti2005).
Finally, we used key player analysis (Borgatti, Reference Borgatti2008) as another way to define ‘importance’ by identifying which node(s) that, when removed from the network, resulted in maximal fracturing of the network into several smaller components. By fracturing a connected network into smaller, disconnected components one can disrupt the spread of information through the network. Although measures of centrality and key player analysis are both ways to identify ‘important’ nodes within the network, key player analysis identifies nodes that maintain the cohesiveness of the network. In other words, ‘key players’ are the nodes that, when removed, would result in a residual network with the least amount of cohesion possible. Removing nodes with high centrality, however, does not necessarily reduce the cohesion of the network into smaller sets of components. Thus, measures of centrality and key player analysis provide different and unique information about potential clinical applications.
The optimal set of ‘key players’ is determined by a measure known as ‘fragmentation’, which is defined as the ratio between the number of pairs of nodes that are not connected once the set of key players have been removed, and the total number of pairs in the original fully connected network (i.e. prior to the removal of the set of key players). The minimum fragmentation value of zero indicates that the network consists of a single component (i.e. it has not fractured), and the maximum fragmentation value of one indicates that the network has been completely fractured, solely consisting of isolates, or nodes with no connections (Borgatti, Reference Borgatti2006).
Ethical standards
All procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Results
Fig. 1 shows the suppressed network that contains links with correlations ⩾0.30. Abbreviations are used to designate each of the 45 EPSI items (see Table 1); these abbreviations are used in the figures depicting the centrality values of nodes.

Fig. 1. Eating disorders network. Each node represents an item on the Eating Pathology Symptoms Inventory (EPSI), and each link represents the zero-order correlation between each pair of items. Only links with r ⩾ 0.30 are shown. The thickness of a link represents the magnitude of the correlation. Abbreviations for each node are provided in Table 1. Louvain community detection (Blondel et al. Reference Blondel, Guillaume, Lamboitte and Lefebvre2008) was used to identify the presence of densely connected subgroups of nodes within the network (Newman, Reference Newman2006) or ‘communities’. Louvain community detection revealed the presence of seven ‘communities’, which approximated the covariance structure of the EPSI (Forbush et al. Reference Forbush, Wildes, Pollack, Dunbar, Luo, Patterson, Pollpeter, Stone, Bright and Watson2013). These communities reflected: Restricting (Community 1); Muscle Building scale items that assess protein supplement and steroid misuse (Community 2); Body Dissatisfaction (Community 3); Excessive Exercise, Cognitive Restraint, and an item that reflects desire for increased muscularity (Community 4); Negative Attitudes toward Obesity (Community 5); purging behaviors, excluding self-induced vomiting (Community 6); and binge eating items, plus the self-induced vomiting item (Community 7).
Table 1. Abbreviations for EPSI items a
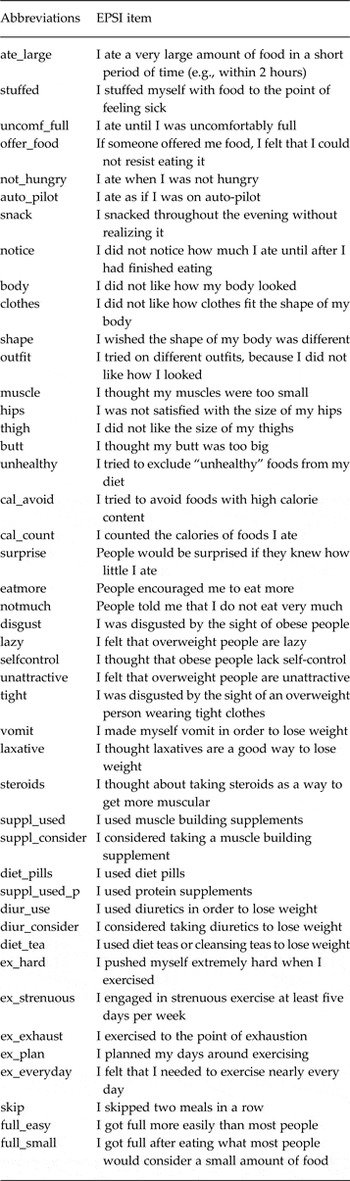
EPSI, Eating Pathology Symptoms Inventory.
a To download a copy of the EPSI, please visit https://psych.ku.edu/kelsie-t-forbush. Please note that the EPSI is free for non-commercial research or clinical use. Any modification of items must be approved in writing from the copyright holder (Kelsie Forbush). Copyright 2011 Kelsie Forbush.
As shown in the centrality plots (Fig. 2), EPSI items that have the highest strength (in descending order) include: trying on different outfits because one did not like how one looked (outfit), excessive exercise (ex_hard), eating when not physically hungry (not_hungry), being disgusted by the sight of obese people (disgust), and not liking how one's body looked (body). Nodes that had the highest closeness centrality (in descending order) included: trying on different outfits because one did not like how one looked (outfit), trying to avoid foods with high calorie content (cal_avoid), not liking how clothes fit the shape of one's body (clothes), not liking how one's body looked (body), and not liking the size of one's thighs (thigh).

Fig. 2. Centrality measures for the eating disorders network representing the betweenness, closeness and strength of each node. Abbreviations for each node are provided in Table 1.
Nodes that had the highest betweenness centrality (in descending order) included: trying on different outfits because one did not like how one looked (outfit), considered taking diuretics to lose weight (diur_consider), excessive exercise (ex_hard), trying to avoid foods with high calorie content (cal_avoid), and planned one's days around exercising (ex_plan). It is noteworthy that trying on different outfits (outfit) emerged as the symptom with the highest value on all three centrality measures, suggesting that this symptom is of particular importance in the ED network.
In the key player analysis we attempted to find a set of nodes whose removal would partition the network into smaller, disconnected components. The optimal set of three nodes included: people encouraged me to eat more (eatmore), the need to exercise nearly every day (ex_everyday), and trying to avoid foods with high calorie content (cal_avoid). Note that this is not an ordered set, meaning one node in the set is not more ‘important’ than another. Rather, together the nodes represent the set of three nodes that maximally disconnects the network, as evident by a fragmentation value of 0.79. This set of three nodes provided maximal fragmentation with the minimum number of nodes in the set; smaller sets did not produce more fragmentation, and larger sets produced only incremental increases in fragmentation.
Discussion
This project was the first to use network analysis to identify interactive systems of ED symptoms. We hypothesized that symptoms that reflected body dissatisfaction or overvaluation of weight, shape or their control would represent the most central symptoms within the network. Our results supported our hypothesis; body checking (as indicated by trying on different outfits because one did not like how one looked) and various other body dissatisfaction items emerged as some of the most important symptoms within the network, which was reflected by their high values on measures of strength, closeness and betweenness. In support of these findings, Lavender et al. (Reference Lavender, De Young, Wonderlich, Crosby, Engel, Mitchell, Crow, Peterson and Le Grange2013) found that daily body-checking frequency was associated with increased dietary restriction on the same (and next) day. Other research has shown that the frequency of body checking significantly predicted quality-of-life impairment in both mental and physical health, above-and-beyond depression symptoms and relevant demographic variables (Latner et al. Reference Latner, Mond, Vallance, Gleaves and Buckett2012).
Given that body checking emerged as one of the most important nodes within the network, it may be useful for future diagnostic conceptualizations of EDs to consider including body checking as a symptom. Currently the DSM-5 includes ‘undue influence of body weight or shape on self-evaluation’ as a symptom of both AN and BN, but ‘body checking’ itself is not included as a symptom of EDs. Because it is probably easier to report overt behaviors rather than complex cognitive concepts, the inclusion of body checking within future diagnostic manuals may lead to improved diagnostic validity for persons with limited insight or poor abstract thinking abilities, such as children and adolescents.
Excessive-exercise symptoms had connections to desire for muscle building, and other studies have found positive associations between muscularity concerns and excessive exercise (Furnham et al. Reference Furnham, Badmin and Sneade2002; Tiggemann et al. Reference Tiggemann, Martins and Kirkbride2007), with men reporting higher levels of excessive exercise (albeit for different reasons) than women (Forbush et al. Reference Forbush, Wildes, Pollack, Dunbar, Luo, Patterson, Pollpeter, Stone, Bright and Watson2013, Reference Forbush, Wildes and Hunt2014). Excessive exercise also had connections to symptoms of cognitive restraint, indicating that excessive exercise may trigger (or be triggered by) goals to achieve a bigger or thinner body image ideal. It was noteworthy that certain attitudes toward others’ bodies (e.g. believing that overweight people are unattractive) were connected to excessive-exercise behaviors. Although additional research is needed, findings indicate that reducing dietary restraint and cognitions related to desire for muscularity and negative attitudes toward overweight persons could be important treatment targets for patients with compulsive-exercise patterns. Interestingly, one exercise behavior – feeling the need to exercise nearly every day (ex_everyday) – was identified as a key player (along with eatmore and cal_avoid). We suggest that these key symptoms may be useful for generating hypotheses for future treatment development: interventions targeted at these nodes could create ‘firewalls’ in the symptom network, preventing or at least slowing the cascading of symptoms that might be brought on by certain ‘trigger’ symptoms (i.e. symptoms high in centrality measures).
Similar to Hovrud & De Young (Reference Hovrud and De Young2015), we found that self-induced vomiting had lower ‘importance’ within the network, as indicated by low values of betweenness. Other forms of purging (i.e. diuretic and laxative misuse) had low centrality values compared with other ED symptoms. These data do not indicate that purging behaviors are unworthy of clinical attention; it is clear that purging behaviors have deleterious health consequences. However, our data suggest that purging behaviors have fewer connections to other ED symptoms. For example, although self-induced vomiting was most strongly associated with binge-eating behaviors, it had relatively weak connections to other symptoms within the network. Misuse of diuretics or laxatives was connected to restricting behaviors, with weaker connections to other symptoms. Our results indicate that targeting other, non-purging symptoms in the network could have indirect effects on purging behaviors; directly focusing on reducing binge-eating and restricting behaviors is probably all that is needed to ameliorate purging behaviors. These findings support the DSM-5's classification of purging as a method of compensating for perceived or actual binge-eating episodes.
Certain limitations of this study are worth noting. First, the prevalence of certain ED diagnoses in the current study was low. However, lifetime diagnoses of AN and BED were higher, and other research supports the trans-diagnostic relevance of the EPSI in individuals with low-weight EDs (Forbush et al. Reference Forbush, Wildes, Pollack, Dunbar, Luo, Patterson, Pollpeter, Stone, Bright and Watson2013, Reference Forbush, Wildes and Hunt2014). On the other hand, because Mountford et al. (Reference Mountford, Haase and Waller2007) found that body-checking behavior is less prevalent among individuals with AN (v. BN), it will be important for future studies to replicate our findings in samples with greater numbers of individuals with AN. Second, because our study tested associations among ED symptoms at one point in time, directionality cannot be inferred. Third, although our sample size is low for certain latent variable models, Monte Carlo research indicates that samples between 100 and 200 provide reliable estimates of the data in network analysis (Scott, Reference Scott2012). Fourth, consistent with recent research (McNally et al. Reference McNally, Robinaugh, Wu, Wang, Deserno and Borsboom2015), our study used an association network, but research testing partial correlation networks could be informative because a correlation between two nodes might be high, but only because a third variable causes them both. Finally, although studies have shown high correlations between body checking and body image dissatisfaction (Reas et al. Reference Reas, Whisenhunt, Netemeyer and Williamson2002; Shafran et al. Reference Shafran, Fairburn, Robinson and Lask2004; Shafran et al. Reference Shafran, Lee, Payne and Fairburn2007; Berg et al. Reference Berg, Peterson, Frazier and Crow2012), future research is needed to test whether the specific EPSI Body Dissatisfaction scale item ‘I tried on different outfits because I did not like how my body looked’ is associated with greater body checking or avoidance behaviors. Despite limitations, the current study has several strengths. This study was the first to apply network analysis to understanding ED psychopathology. Our study sample had more ethnic–racial diversity than most other published community samples of individuals with EDs. We also used a measure with good discriminant validity, which provided an opportunity to identify the unique contribution of symptoms within the network (in contrast to diagnostic measures that include numerous symptoms within each criterion).
In conclusion, the results of our study support the key mechanisms delineated in CBT-E, given that the most central symptoms within the network represented overt behavior that reflect overvaluation with weight, shape or their control (i.e. body checking) and body dissatisfaction. We believe our findings may be useful for generating hypotheses to be tested in future treatment studies. For example, although CBT-E already includes techniques to address overvaluation of weight, shape or their control, focused work on body checking is introduced after the first eight sessions of therapy (Fairburn, Reference Fairburn2008). Our findings suggest that it may be informative to test whether introducing body-checking ‘experiments’ earlier in CBT-E improves treatment response, given that rapid, early change among patients with an ED has been shown to be an important predictor of outcome (Agras et al. Reference Agras, Crow, Halmi, Mitchell, Wilson and Kraemer2000; Raykos et al. Reference Raykos, Watson, Fursland, Byrne and Nathan2013). More targeted interventions for reducing body checking may also be useful for producing improved outcomes such as focused mirror exposure, which has shown promise for reducing long-term behavioral and cognitive expressions of overvaluation in non-clinical women with high levels of pre-treatment body dissatisfaction (Jansen et al. Reference Jansen, Voorwinde, Hoebink, Rekkers, Martijn and Mulkens2015). Additional future directions for research include understanding neuropsychological or personality-based mechanisms that underlie associations between body checking and other ED symptoms. Targeted treatments that disrupt mechanisms underlying body checking may lead to reductions in ED symptomatology and improvements in quality of life for individuals with EDs.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S003329171600012X
Acknowledgements
This work was supported by the Clifford B. Kinley Trust, and the University of Kansas New Faculty Research Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Declaration of Interest
None.





