Introduction
Prehospital first responders and other medical personnel historically have treated patients with hypoglycemia with 50% dextrose solution (D50). The D50 is a hypertonic solution of glucose available in prefilled syringes containing 25 grams of glucose in 50 mL of water. Although individual protocols vary, in patients unable to take oral glucose, it is often given as a bolus after initial patient assessment, glucometer confirmation of hypoglycemia, and obtainment of intravenous access.
There are several reasons, both practical and theoretical, that treating hypoglycemia with a bolus of D50, despite long tradition, may not be the right choice. First, there is a nationwide shortage of D50 in the United States, which has affected the ability of Emergency Medical Services (EMS) systems to stock adequate supplies of the solution. It also is relatively more expensive than other glucose-containing solutions. Prefilled 50 mL syringes of D50 are available to the California Contra Costa County EMS system at a cost of $5.58 each, versus $1.62 for a 250 mL bag of 10% dextrose solution (D10), from which a 100 mL aliquot is initially infused. In addition, D50 is more viscous than other intravenous fluids and often requires two hands to administer, preventing paramedics from doing other tasks such as electrocardiograms or neurological assessments, during its administration.
Theoretical reasons to avoid D50 include the potential greater risk of extravasation injury, potential supratherapeutic dosing of glucose causing hyperglycemia, and direct toxic effects of hypertonic dextrose itself.Reference Baker, Rattan and Bruno 1 , Reference Browning, Olson, Stueven and Mateer 2 Animal models have demonstrated the toxic effect of glucose infusions in the settings of cardiac arrest and stroke.Reference Browning, Olson, Stueven and Mateer 2 Experimental data suggests that hyperglycemia is neurotoxic to patients in the setting of acute illness.Reference Baker, Rattan and Bruno 1 , Reference Fahy, Sheehy and Coursin 3 Although no data has linked the use of D50 in the prehospital setting to adverse outcomes, using a lower concentration in a greater total volume of solution might help to mitigate some of the potential risks of D50.
Further, despite its long use, there is little data to support D50 as a given standard. Review of prior literature reveals only one trial comparing D50 to D10 for the treatment of hypoglycemia.Reference Moore and Wollard 4 In a trial of 51 adult hypoglycemic patients with altered mental status treated by paramedics from a large United Kingdom ambulance service, patients were randomized to receive 5 gram (50 mL) intravenous aliquots of D10 or 5 gram (10 mL) intravenous aliquots of D50 to a maximum dose of 25 grams. There was no statistical difference in the main outcome of time to regain normal consciousness, leading researchers to conclude that their D10 protocol was safe and effective. The D10 group received less total glucose and had lower post-treatment glucose levels in the study.
Beginning January 1, 2013, the California Contra Costa County EMS system began using 100 mL of intravenous D10 as its primary intravenous agent to treat hypoglycemia, and collected 18 weeks of clinical and demographic data as part of ongoing quality control measures examining this approach. Previously, D50 had been the first-line intravenous dextrose agent in this system. The decision was made largely due to frequent shortages of D50 and the relative lower cost of D10, as well as the theoretical benefit of not using D50. As a part of the protocol change, and in coordination with study investigators, demographic and clinical data on patients who received D10 in the field were collected prospectively by EMS personal. The goal of this study was to present and analyze the data collected on patients who were hypoglycemic on EMS arrival and received intravenous D10 as their initial treatment, and to position these results in the context of the relevant literature on this approach.
Methods
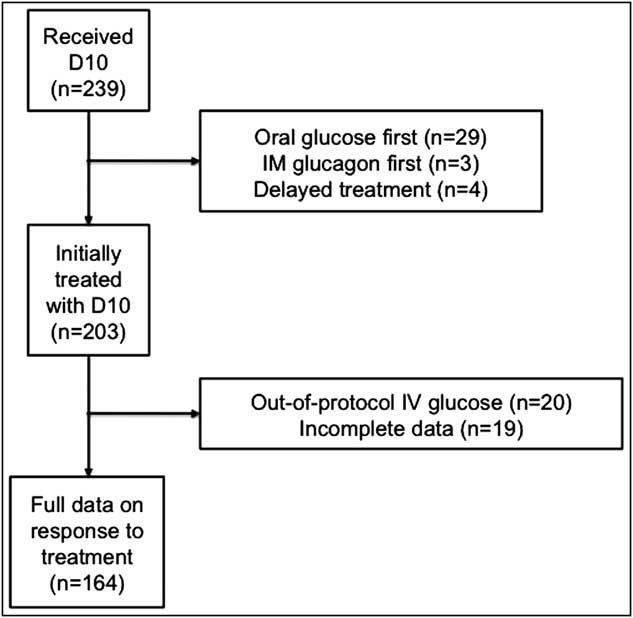
This study was observational and quantitative using prestudy defined indicators. Study investigators were involved in the design of the EMS system's D10 protocol, and EMS personnel in the field recorded study data prospectively during patient encounters. Analysis was focused on patients: (1) who were older than age 18; (2) who displayed symptoms of hypoglycemia on the clinical judgment of paramedics; (3) whose level of consciousness and ability to cooperate did not allow administration of oral glucose; (4) whose blood sugar was below 70 mg/dL as evaluated in the field; and (5) in whom intravenous access could be obtained. Of the 239 patients who were administered D10 by EMS personnel in the 18 weeks of data collection, 203 met these criteria (Figure 1). The remaining 36 patients were excluded by the following criteria: 29 patients received oral glucose initially by paramedics; three patients received intramuscular glucagon; and four patients were euglycemic or hyperglycemic on EMS arrival. Of the 203 patients who met criteria, 20 patients received out-of-protocol IV glucose, for example, in aliquots greater or less than 100 mL. Another 19 patients had incomplete data on response to D10, most commonly because of hospital arrival before repeat glucose value could be obtained. The remaining 164 patients received initial treatment with 100 mL of IV D10 and had repeat glucose measurements recorded.
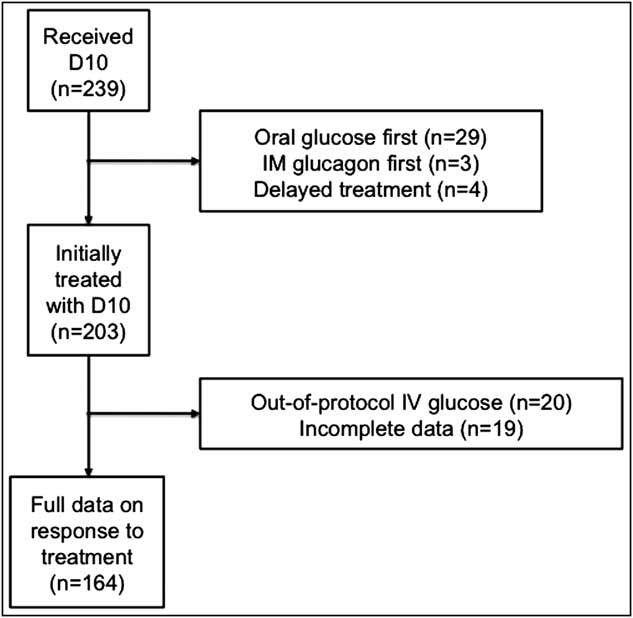
Figure 1 Patient Selection Abbreviations: D10, 10% dextrose solution; IM, intramuscularly.
The outcomes measured included the blood glucose response to initial infusion of 100 mL of D10 as well as repeat infusions if necessary. Given that the point-of-care blood glucose machines used by EMS personnel do not read glucose values lower than 20-25 mg/dL (depending on the machine) and instead indicate “Low,” a glucose value of 20 mg/dL was assumed when comparing relative glucose values for values of “Low” in this analysis. A linear regression line was fit between elapsed time and difference between glucose value on EMS arrival and subsequent recheck after infusion of initial 100 mL of D10. Emergency Medical Services personnel also were instructed to record any adverse events pertaining to glucose administration.
Data analysis was performed using Microsoft Excel (Version 12.3.6, Microsoft Corporation, Redmond, Washington USA). The Institutional Review Board of the Alameda Health System—Highland Hospital approved the study as exempt from review.
Results
The study cohort of 164 patients included 102 men and 62 women with a median age of 68 years and an interquartile range (IQR) of 55 years-80 years (Table 1). The median initial field blood glucose was 38 mg/dL (IQR = 28 mg/dL-47 mg/dL), with subsequent blood glucose median of 98 mg/dL (IQR = 70 mg/dL-135 mg/dL). Elapsed time after D10 administration before recheck was not uniform, with a median time to recheck of eight minutes (IQR = 5 minutes-12 minutes). Of 164 patients, 29 (18%) received an additional dose of intravenous D10 solution in the field due to persistent or recurrent hypoglycemia, and one patient required a third dose.
Table 1 Patient Demographics and Results in Study Cohort

Abbreviation: D10, 10% dextrose solution.
Of the 164 patients analyzed, median change in glucose after D10 administration was 59 mg/dL (IQR = 32 mg/dL-95 mg/dL) (Figure 2). Three patients had a drop in blood glucose after D10 administration: one patient had a drop of 1 mg/dL; one patient had a drop of 10 mg/dL; and one patient had a drop of 19 mg/dL. The patient with the drop of 19 mg/dL had an insulin pump infusing that was not removed by EMS personnel during D10 infusion. The remaining 161 had an elevation of their blood glucose on recheck (maximum rise to 325 mg/dL). Linear regression analysis of elapsed time and difference between initial and repeat glucose values after D10 showed near-zero correlation, which suggested that serum glucose had minimal decay over the study interval. Figure 2 shows the line of best fit for change in blood glucose after administration of D10.

Figure 2 Change in Blood Glucose after 100 mL of D10. Each point on this graph represents a unique patient (n = 164). The y axis of this graph represents the absolute change in blood glucose in mg/dL between the initial value obtained by EMS personnel and the subsequent value obtained after D10 infusion. A positive value indicates that the patient's blood glucose increased and a negative value indicates that the patient's blood glucose decreased. The x axis represents time in minutes that transpired between the initial value obtained by EMS personnel and the subsequent value after D10 infusion for the patient. Each point therefore represents an absolute change in blood glucose during a given time. A line of best fit was applied to these data points using linear regression. The flat slope suggests that there may be little or no short-term decay in blood glucose values after D10 administration. Abbreviations: D10, 10% dextrose solution; EMS, Emergency Medical Services.
There were no reported adverse events related to glucose infusion. Two patients who received intravenous D10 were pronounced dead in the field during the period of study. On review of records by investigators, both patients were unresponsive or in cardiac arrest prior to arrival of EMS personnel, and their deaths were unrelated to dextrose administration.
Discussion
Glucose control in critically-ill patients remains challenging. While not frequently studied in the prehospital setting, evidence on the optimal glucose range in the inpatient setting remains controversial.Reference Fahy, Sheehy and Coursin 3 Hypoglycemia has known neurologic adverse effects in critically-ill patients;Reference Duning, Opiyo and English 5 however, both in animal and patient studies, hyperglycemia also has been shown to negatively affect neurologic outcomes.Reference Baker, Rattan and Bruno 1 , Reference Fahy, Sheehy and Coursin 3 , Reference Nakakimura, Fleischer and Drummond 6 Extrapolating inpatient data to the prehospital setting is problematic for multiple reasons. These include the relatively few monitoring resources and therapeutic interventions available in the prehospital setting, the short duration of time that patients are under EMS care, and the relatively low acuity of patients encountered in the prehospital settingReference Cain, Ackroyd-Stolarz, Alexiadis and Murray 7 compared with the intensive care unit.
Despite limitations of existing data and its relevance to the prehospital setting, the optimal treatment of prehospital hypoglycemia should have several features. First, a prehospital treatment regimen must effectively raise the blood glucose. Second, it must be feasible for prehospital care providers to implement. Third, it must be efficient across at least three dimensions: cost, time, and effort. And finally, it must be safe for patients. The current practice of utilizing D50 in the treatment of acute hypoglycemia has shown efficacy, feasibility, and safety in the limited trial data available.Reference Moore and Wollard 4 , Reference Cain, Ackroyd-Stolarz, Alexiadis and Murray 7 – Reference Patrick, Collier, Hepburn, Steedman, Clarke and Robertson 9 Several authors, however, have raised concerns regarding the potential of D50 to cause harm, despite lack of direct evidence.Reference Browning, Olson, Stueven and Mateer 2 , Reference Hoffman, Schriger, Votey and Luo 10 , Reference Hoffman and Goldfrank 11 In theory, using smaller aliquots of glucose might mitigate concerns regarding the risk of hyperglycemia and a more dilute solution might mitigate risks regarding extravasation injury. The only clinical trial to date comparing D50 to D10 showed no difference in the primary outcome of time to return to Glasgow Coma Scale of 15; however, there were no safety differences identified.Reference Moore and Wollard 4
Reported study data demonstrates that utilizing D10 as the primary intravenous treatment for hypoglycemia is efficacious, with all but three patients demonstrating an increase in their blood glucose after D10 administration. Although a patient-centered outcome such as time to return to normal mental status was not measured, previous trial data shows correlation between increase in serum glucose and return to normal mental status.Reference Moore and Wollard 4 , Reference Collier, Steedman and Patrick 8 , Reference Patrick, Collier, Hepburn, Steedman, Clarke and Robertson 9 Of the study patients, only 29 out of 164 (18%) received a second bolus of D10 in the field; however, some patients who only received one dose of D10 may have received additional dextrose on arrival to hospital, and relative comparison to D50 is not known. No complaints or concerns were noted by paramedics in the field in terms of ease of D10 use and how it compares with D50. Some providers did note that D10 is easier to infuse, owing to its lower viscosity than D50. Economic or resource utilization analysis is not available. The data shows that D10 administration is safe, with no adverse events related to administration in this small series.
The linear regression fit line of repeat blood glucose measurement against elapsed time suggests that there may be little or no short-term decay in blood glucose values after D10 administration. Previous analysis of D50 in healthy volunteers shows that D50 reliably increases serum glucose over the first five minutes after administration; however, by 30 minutes, blood glucose levels consistently approach pretreatment levels.Reference Balantine, Gaeta, Kessler, Bagiella and Lee 12 All of the glucose recheck times were before 30 minutes, allowing that the lack of short-term decay might not have continued if longer-term data were available on study patients. Alternatively, D10 may elicit a less aggressive insulin response than D50 and may paradoxically have a slower decay than D50 from the blood stream. Reported data are inadequate to test this hypothesis and this remains a question for future study.
Limitations
In this study, a case series without any control group is presented, so conclusions are observational. Long-term follow-up after the prehospital setting was not available and economic analysis is not reported. The regression analysis, a simple fit line, is limited and not controlled for associated and possibly influential covariates. In addition, while there were no reported adverse outcomes related to D10 administration and all patients became euglycemic eventually, it is not clear if there were delays to euglycemia in the reported group compared to D50. Finally, in those patients who did require a second, or even a third, dose of D10, it is not possible to ascertain if there were longer-term unfavorable outcomes because of the protocol change.
Conclusions
In addition to practical reasons of cost, availability, and ease of use, theoretical risks of using D50 in the out-of-hospital setting include extravasation injury, direct toxic effects of hypertonic dextrose, and potential neurotoxic effects. The experience of one local EMS system over an 18-week period demonstrates that D10 is a safe, effective, and feasible alternative to D50 in the acute prehospital management of hypoglycemia.
Acknowledgements
The authors would like to thank all of the paramedics who treated patients in the field during the course of this study.