Published online by Cambridge University Press: 26 August 2005
Traditional neuropsychological measures of executive dysfunction (ED) are widely believed to lack adequate sensitivity and selectivity. This may indicate that existing measures are poorly designed and constructed, although an alternative explanation is that executive cognition is multifactorial, such that its assessment necessarily requires administration of multiple measures. This possibility led to the development of a test battery, the Behavioural Assessment of the Dysexecutive Syndrome (BADS). To investigate the sensitivity of the BADS to ED, it and various other measures of ED were administered to 64 persons who had sustained traumatic brain injury. The treating clinical neuropsychologist and occupational therapist for each participant also completed a behavioural rating scale, the Dysexecutive Questionnaire (DEX). Four factors were found to underlie scores on the neuropsychological measures, but few tests were sufficiently powerful to make a significant unique contribution to predicting scores on the DEX. This confirms that multiple tests, drawn from both the BADS and other sources, may be necessary to detect ED in a clinical population. (JINS, 2005, 11, 606–613.)
Executive dysfunction (ED), a collection of functional deficits in the higher-order cognitive skills required to initiate, plan, execute and monitor complex goal-directed activities (Banich, 1997; Tranel et al., 1994), is associated with a range of neurological disorders, especially those involving prefrontal brain regions or diffuse brain damage. A number of neuropsychological instruments are commonly used to assess ED (Lezak, 1995). In group situations these tests are typically sensitive to frontal lobe pathology and many have been shown to discriminate between unimpaired controls and patient groups with a high incidence of ED, such as those with traumatic brain injury (TBI) or dementia. Adequate discriminant validity, however, also requires that the measures discriminate between persons with and without ED, regardless of its etiology or the presence of other cognitive difficulties. This level of analysis has not been widely reported although it is well known that many tests of ED lack specificity, such that performance on them can be impaired by cognitive deficits other than ED. The tests also appear to lack sensitivity. There are numerous reports in the literature of persons who display adequate performances on traditional neuropsychological tests of ED, but who demonstrate ED in everyday life.
This represents a significant difficulty for clinicians required to identify patients with ED. One explanation is that available tests simply lack sensitivity and selectivity, due to inadequacies in design and associated psychometric shortcomings. Many of the tests, for example, are highly structured, time limited and have clear outcome measures, bearing little resemblance to the ill-structured activities that characterize modern lives. They are also necessarily standardized in administration and scoring procedures, with no allowance for the effect that premorbid experiences may have on the degree of novelty or challenge presented by a particular task. Alternatively, the problem may not rest with existing measures at all but, instead, may reflect inadequacies in the conceptualization and operational definition of the concept itself. Rather than reflecting a single entity, it is now widely believed that the term ED refers to a heterogeneous and poorly defined group of cognitive deficits, all leading functionally to so-called executive difficulties (Burgess et al., 1998; Shallice, 2002; Stuss & Alexander, 2000). If so, then there is no reason to expect a single test to be sensitive to all presentations of the disorder, especially in a heterogeneous patient group. Instead, identification of ED may require administration of a battery of subtests, each requiring executive skills but each sensitive to particular aspects of the disorder. This approach, of course, is used to assess other complex cognitive domains such as intelligence and memory.
In accordance with this possibility, Wilson et al. (1996) developed a test battery called the Behavioural Assessment of the Dysexecutive Syndrome (BADS). The six subtests included in the battery were chosen on the basis of ecological validity and each has adequate face validity as a test of ED (Wilson et al., 1998). Performance on each subtest is reduced to a score out of four. These scores are then summed to derive a composite “profile” score, claimed to provide an overall measure of ED. The BADS also includes a 20-item questionnaire about everyday executive problems, the Dysexecutive Questionnaire (DEX), which can be administered to a brain-injured person or to an independent rater familiar with the injured person. In an initial pilot study (Alderman et al., 1993), and a subsequent validation study (Wilson et al., 1996, 1998) the BADS was administered to neurologically intact adults and persons with a variety of neurological disorders including closed head injury (59%), dementia (13%) and stroke (8.5%). The brain-injured participants obtained significantly lower scores both overall and on each subtest, the greatest differentiation between groups being in terms of the composite score. DEX ratings provided by a family member (FM-DEX) were also significantly negatively correlated with all measures from the BADS.
Subsequent research using the BADS has produced mixed results. First, the significant association between FM-DEX ratings and BADS measures has proven difficult to replicate. Several studies have reported low correlations between the FM-DEX and the total BADS score, and nonsignificant or even reversed correlations between the scale and several BADS subtests (Bennett et al., 2005; Evans et al., 1997; Norris & Tate, 2000). Second, FM-DEX ratings have been found to be only moderately associated with DEX scores provided by a clinical neuropsychologist (NP) and occupational therapist (OT), even though ratings provided by both therapists were strongly associated with each other and also significantly correlated with impaired processing speed and the severity of head injury sustained (Bennett et al., 2005), both known to be good predictors of outcome following TBI. While the therapist ratings were significantly associated with the BADS total score in this study, three BADS subtests were not significantly associated with the ratings. Conversely, the degree of association between three of the subtests and the ratings was equally if not more robust than the association between the ratings and the total BADS score.
A final area of interest is that very few studies have examined correlations between the FM-DEX and other neuropsychological tests of ED or between therapist-rated DEX scores and these other existing tests. Thus, the ability of other ED tests to predict scores on the DEX has not been adequately examined. It is possible that one or more existing tests are equally or more sensitive to ED, as identified by DEX ratings, than is the BADS, or that specific subtests from the BADS would be more sensitive if administered in conjunction with other measures. It is also possible, of course, that using therapist rated DEX scores as a gold-standard measure of ED, against which other measures can be assessed, is inappropriate. The data presented in our previous paper, however, showing strong correlations between NP- and OT-DEX ratings and between these ratings and other outcome scores, argues against this possibility (Bennett et al., 2005).
The aim in the present study was to determine, in an adult TBI sample, the degree to which neuropsychological measures claimed to be sensitive to ED, other than those included in the BADS, are associated with DEX rating scores provided by professional therapists, and whether any of these measures, either singly or in combination with individual subtests from the BADS, might predict DEX ratings with reasonable accuracy. The study was conducted using the same persons who participated in the study reported by Bennett et al. (2005). ED is a common consequence of TBI but occurs to varying degrees depending on the nature and location of damage sustained (Levin & Kraus, 1994). A TBI sample was selected as the focus of the study, therefore, to provide the heterogeneity required for correlational analyses. TBI offers the additional advantage of providing a relatively young and premorbidly functionally intact population, which reduces the possibility of spurious associations due to the documented effects of age (Bryan & Luszcz, 2000; Crawford et al., 2000) and intelligence (Ardila et al., 2000; Obonsawin et al., 2002) on some variables sensitive to ED.
There were 64 participants in this study. All were patients at Bethesda Rehabilitation Centre, in Melbourne, Australia. Most (60) were road accident victims, the remainder (4) having sustained workplace accidents. All participants had experienced loss of consciousness following their injury but the duration of post-traumatic amnesia (PTA) ranged from several hours to 100 days (M = 23.28 days, SD = 22.78). Glasgow Coma Scale scores obtained at acute hospital admission were available for 35 participants and ranged from 3 to 15 (M = 7.06, SD = 3.90).
Participants were excluded if they did not speak fluent English or if they were unable to undertake the assessment due to profound motor or cognitive disabilities. There were 47 male and 17 female participants, ranging in age from 17–73 years (M = 32.72, SD = 14.49) and in education from 9–19 years (M = 12, SD = 2.3). All except 5 participants were seen within 1 year of injury (range = 15 days–30 years, MDN = 63 days), 48 being hospitalized at the time of assessment. Information regarding previous difficulties with learning (4), substance use (6), psychopathology (4), neurological illness (2) and head injury (1) was noted, but participants were not excluded on the basis of this information or on the basis of factors like age or time post injury. This meant that as many participants as possible were included in the study, thus maximising the statistical power of the analyses conducted.
Of the 64 participants, 24 had documented damage to anterior sections of the brain (8 bilateral, 8 left hemisphere, 8 right hemisphere). The remaining 40 participants had documented lesions elsewhere or no documented evidence of localized brain injury, but all participants had been formally assessed by medical staff as having sustained a TBI. The state of Victoria, Australia, has a no-fault transport accident insurance policy and none of the participants was known to be undertaking litigation at the time of assessment. While there was no formal attempt to exclude the effects of insufficient effort on participant's performance, this was not thought to reflect a significant impediment given the voluntary nature of participation in this project and the context in which it was conducted.
The 20-item DEX was completed by the treating neuropsychologist (NP-DEX) and the treating occupational therapist (OT-DEX).
All participants completed each subtest from the BADS as part of their involvement in a previous study (Bennett et al., 2005). The following measures were derived from these data: the Rule Shift Card Test (rulsft), the Action Program Test (ACTPRO), the Key Search Test (KEYSRC), the Temporal Judgement Test (TEMPJ), the Zoo Map Test (ZOOMAP) and the Modified Six Elements Test (MSET). The scores for each subtest were reduced, as advised by Wilson et al. (1996), to a single score. A previous study has reported that the norms provided for one BADS subtest, the Temporal Judgement Test, may be inappropriate for an Australian population (Norris & Tate, 2000). Because Australian norms are not available, two separate composite scores for the BADS were calculated. The first (BADS) included the score for the Temporal Judgement Test, calculated using the formula provided by Wilson et al. (1996). The second (MBADS) comprised summed profile scores for each of the remaining five subtests from the BADS.
One week after completing the BADS and the DEX, participants completed a number of other tests commonly used to assess ED. These were selected on the basis of literature arguing that they may be more sensitive to ED than similar instruments. Banich (1997) has previously argued that executive dysfunction may be reflected as difficulties in the initiation, cessation and control of action, in abstract and conceptual thinking, in using previous knowledge to guide behavior in other contexts, in cognitive flexibility and response to novelty, in sequencing, in shifting set and modifying strategies, in using contingencies to guide behavior, and in self-monitoring. Therefore, care was taken to ensure that each of these constructs was likely to be sampled by at least two measures. Selected for inclusion in the study was the Wisconsin Card Sorting Test (WCST), administered according to Heaton (1981). Two measures were derived from this test, the percentage of correct responses (WCS%COR) and the percentage of perseverative errors (WCS%PER). The Porteus Maze Test (Porteus, 1965) was also included, with test age, as defined by the test manual, being used to represent this measure (PORTEUS). The Trail Making Test (TMT) and the Controlled Oral Word Association Test (COWAT), both administered according to Lezak (1995), were also included. Because the FAS version of the COWAT is routinely administered at Bethesda, the PRW version was used in the current study. The dependent variable (COWAT) was the total number of correct words generated. Completion time for the TMT–B was included as a variable (TMT–B) but, to reduce the impact of slowed processing speed on this variable, a second measure (TMT–B/A) was calculated as the ratio between completion time for TMT–B and completion time for TMT–A. Two other tests, claimed to be sensitive to ED, were also administered. These were the Revised Tinker Toy Test (Lezak, 1993) and a version of the Cognitive Estimation Test (Shallice & Evans, 1978), modified by Axelrod and Millis (1994) so as to facilitate quantification of results. The variable derived from the Tinker Toy Test (TTT) was the complexity score (Lezak, 1993). The modified Cognitive Estimate test (MCET) was scored using normative data provided by Axelrod and Millis (1994).
Over a period of 10 months, consecutive admissions to Bethesda rehabilitation hospital who met the criterion were invited to participate in the study. Participants underwent two testing sessions separated by 1 week, each lasting approximately 1 hr. The BADS and DEX (PT-DEX) were administered in the first session, following which a DEX scale was also completed by the treating clinical neuropsychologist (NP-DEX). This person, who was not the experimenter, was asked to complete the rating scale on the basis of their own assessment of the participant, prior to accessing any test data from this study. A DEX scale was also completed, where possible, by an occupational therapist (OT) familiar with the patient. Both groups of professionals had worked with each patient during their time as an inpatient at the hospital, which ranged from 2 weeks to several months. Some of the longer-term patients had been part of the rehabilitation community for several years and were well known to staff members. These participants, therefore, may have previously been administered some of the tests included in this study by the treating neuropsychologist. Others were less well known, but all had been seen by each professional at least three times during their period of admission. It was anticipated that OT-DEX scales would be obtained for each participant but, midway through the study, administrative changes at Bethesda prevented the participation of OT staff in the study. These were obtained, therefore, for only 45 of the 64 participants. All remaining tests were administered in the subsequent session, with all testing being conducted by a single experimenter. All data analysis was conducted using SPSS for Windows. Missing data were excluded on a pair-wise basis.
Correlations between the BADS subtests and total scores and the NP- and PT-DEX scores were reported in an earlier paper (Bennett et al., 2005). To assess the sensitivity of the remaining tests to ED, correlations between measures from the tests and NP- and OT-DEX ratings were examined (Table 1). From Table 1 it can be seen that several measures were moderately associated with the NP-DEX. The strongest associations were with the Porteus Maze Test and the Modified Cognitive Estimates Test. The magnitude of these associations approached that obtained for the three BADS subtests and two BADS composite scores found previously to be significantly associated with the NP-DEX (RULSFT = −.32, ACTPRO = −.36, MSET = −.36, BADS = −.37, MBADS = −.32; Bennett et al., 2005) . More modest correlations were found for the Tinker Toy Test and measures from the WCST. Measures from the COWAT and TMT–B were not significantly associated with NP-DEX ratings. Although these relationships approached significance, the weak association for the time taken to complete TMT–B disappeared when processing speed was partially removed by expressing it as a percentage of time taken to complete TMT–A. In addition, the number of correlations performed means that the results should be interpreted with caution, particularly given the limited number of participants.
Correlations between neuropsychological measures and DEX rating scores provided by neuropsychologists and occupational therapists

While a different pattern of statistical associations was found between the neuropsychological measures and OT-DEX ratings than was obtained for NP-DEX ratings, none of the differences was large. OT-DEX ratings were moderately associated with several neuropsychological measures although, possibly because of the limited number of OT-DEX ratings available, statistical support for the associations was weaker and should be interpreted cautiously. A reasonably strong association was found between OT-DEX ratings and the percentage of correct responses achieved on the WCST. Weaker but significant associations were also found between OT-DEX ratings and scores on the Porteus Maze Test and TMT–B, and for the percentage of perseverative errors made on the WCST. OT-DEX ratings were not significantly associated with scores on the Modified Cognitive Estimates Test, nor were they significantly associated with several other measures found to be significantly associated with NP-DEX ratings. While the differences are unlikely to be statistically significant, it might be of interest in future to investigate whether neuropsychologists and occupational therapists are particularly sensitive to different types of functional deficits.
In order to investigate whether a combination of neuropsychological measures, taken from the BADS individual subtests and elsewhere, may provide the most accurate source of information about the presence of ED, several exploratory analyses were undertaken. The first technique employed was factor analysis, in which all neuropsychological variables included in this study, including those from the BADS reported previously, were factor analyzed by the principal axes method. Four factors were extracted with eigenvalues greater than one, accounting for 49% of the total variance. The factors were obliquely rotated, as there was no good reason to assume that the underlying executive functions were unrelated to one another, producing the pattern matrix reproduced in Table 2. Only loadings exceeding .3 are presented.
Factors of neuropsychological functioning extracted by the principal axes method
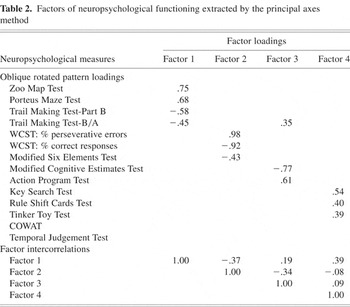
The first factor presented in Table 2 was comprised of four measures, two derived from the Trail Making Test and one each derived from the Zoo Map Test and Porteus Maze Test. Each measure loaded strongly on the factor, with loadings ranging from .45 to −.75. The second factor was comprised of three measures, two derived from the WCST and one derived from the Modified Six Elements Test. The two measures from the WCST loaded strongly on this factor, a more modest loading being observed for the measure from the Modified Six Elements Test. Scores from the Modified Cognitive Estimates Test and Action Program Test loaded strongly on the third factor, while a measure from the Trail Making Test, which loaded more strongly on Factor 1, also contributed. The fourth factor was comprised of measures from the Key Search Test, Rule Shift Test and Tinker Toy Test. All measures loaded only moderately on this factor. Consistent with previous evidence suggesting that the Temporal Judgement Test is not a valid indicator of neuropsychological constructs in an Australian population, the score from this test failed to load on any of the factors derived. This was also found for the measure derived from the COWAT, which failed to load on any factor.
Intercorrelations between the factors are also presented in Table 2. These suggest that four dissociable constructs may underlie scores on the neuropsychological instruments sensitive to ED. Interestingly, the tests found to be most strongly associated with NP-DEX ratings (Rule Shift Card Sort Test, Action Program Test, Modified Six Elements Test, Modified Cognitive Estimates Test and Porteus Maze Test), were distributed across the four factors, at least one measure falling into each group. A similar situation pertains to those measures found to be most strongly associated with OT-DEX ratings (Rule Shift Card Sort Test, Action Program Test, WCST, Modified Six Elements Test, and Porteus Maze Test). To ascertain whether measures from each factor might contribute uniquely to prediction of scores on the NP- or OT-DEX, multiple regression analyses were conducted. For the first analyses all neuropsychological indicators of ED (except the composite BADS scores) were entered together as potential predictors of NP- or OT-DEX scores. This revealed that the combined variables acted as a significant predictor of NP-DEX ratings [R2 = .39; F(14,42) = 1.95, p < .05], although the level of statistical significance was weak (p = .048) and further analysis (Table 3) revealed that no single variable made a significant unique contribution to the prediction of NP-DEX scores. Only the Porteus Maze Test approached significance (p = .053). When all neuropsychological indicators of ED were entered as potential predictors of OT-DEX ratings, the result was not statistically significant [R2 = .46; F(14,28) = 1.73, p > .05]. Given the reasonable value of R2, the lack of statistical significance probably reflects the low number of OT-DEX ratings included in the analysis. As expected on the basis of this result, no single variable made a significant unique contribution to the prediction of OT-DEX scores (Table 3).
Standard multiple regression of neuropsychological measures predicting NP- and OT-DEX ratings

These initial exploratory analyses were clearly limited in power because of the large number of variables included and the limited number of participants. A second type of analysis was conducted, therefore, in which the same neuropsychological measures were entered into the regression equations in a step-wise manner. The first of these analyses (Table 4) revealed that two measures acted as significant unique predictors of NP-DEX ratings (R2 = .22). These variables were the Porteus Maze Test [F(1,55) = 8.42, p < .005] and the Modified Six Elements Test [F(2,54) = 7.57, p < .001]. The second analysis (Table 4) revealed that only one variable, the Action Program Test, acted as a significant unique predictor of scores on the OT-DEX [R2 = .26, F(1,41) = 14.47, p < .001].
Stepwise multiple regression of neuropsychological measures predicting NP- and OT-DEX ratings

In a previous paper (Bennett et al., 2005) we reported finding moderate negative associations between the BADS total score and the NP- and OT-DEX. The degree of association between several subtests and NP- or OT-DEX ratings was equally if not more robust, however, indicating that some of the subtests may be equally effective in isolation, or in combination with other existing tests. The aim in this study was to determine the relative sensitivity of other neuropsychological tests of ED, again using NP- and OT-DEX ratings as comparison measures. A related aim was to ascertain whether a combination of measures, from the BADS and elsewhere, could be identified that would enable detection of ED. A number of measures were significantly associated with NP- and OT-DEX ratings, although the pattern of association differed slightly for the two respondent groups. Only two measures were as strongly associated with NP-DEX scores as were the three effective subtests identified from the BADS; these being the Porteus Maze Test and the Modified Cognitive Estimates Test. The Porteus Maze Test was also moderately associated with scores on the OT-DEX. OT-DEX ratings were not significantly associated with the Modified Cognitive Estimates Test, but were moderately associated with the percentage of correct responses obtained on the WCST.
A number of inconsistencies have been reported following previous attempts to factor analyze measures of ED (Chan, 2001; Kafer & Hunter, 1997; Miyake et al., 2000), rendering available data difficult to interpret coherently. Nevertheless, in order to determine whether a number of dissociable factors may contribute to scores on neuropsychological measures of ED, an exploratory factor analysis of all measures, including those from the BADS, was conducted. Four factors were identified which together accounted for 49% of the variance. It is difficult to speculate about what these factors may represent, given the limited number of participants and large number of variables included in this study. Nonetheless, the factors are reasonably consistent with some of the features of ED identified by Banich (1997), whose conceptualization of ED was used to guide the selection of tests included in this study. Her description of ED includes difficulties in the initiation, cessation, and control of action (Factor 4), in abstract and conceptual thinking and in using previous knowledge to guide behavior in other contexts (Factor 3), in cognitive flexibility and set-shifting in response to novelty (Factor 2), and in sequencing and self-monitoring (Factor 1). Other explanations for these factors are undoubtedly possible, however, and functional descriptions of ED other than that proposed by Banich (1997) abound.
Since the measures shown to be most sensitive to ED were spread across all four factors, multiple regression techniques were used to determine whether any measures made a significant unique contribution to the prediction of NP and OT rating scores. While all measures combined accounted for a significant amount of variance (39%) on the NP-DEX, only two measures, the Porteus Maze Test and the Modified Six Elements Test, made statistically significant unique contributions. All measures combined did not account for a significant amount of variance on the OT-DEX but, given that the amount of variance explained (46%) was consistent with that found for the NP-DEX, this probably reflects reduced statistical power due to the reduced number of OT-DEX scores available. Only the Action Program Test made a statistically significant unique contribution to the prediction of OT-DEX ratings.
On the basis of this study, it can be concluded that the scores derived from existing neuropsychological measures remain only moderately useful for those who wish to assess and document the presence of ED in a heterogeneous clinical population. When all neuropsychological variables were entered into a multiple regression equation, 39% of the variance on the NP-DEX was explained and 46% of the variance on the OT-DEX. This appears reasonable but required the addition of 14 variables, derived from many more tests than are able to be administered during a standard neuropsychological assessment. Many other studies have also concluded that multiple tests may be necessary to adequately assess ED, and that qualitative information is often required to assist interpretation of test results. This has significant implications for both research and clinical practice. If limited time is available to asses ED, then our results indicate that administration of a rating scale, such as the DEX, to professional personnel working with the patient may provide more information than any single test. When formal testing is required, clinicians and researchers alike may simply need to accept that no single test can presently be used to reliably identify ED, and that a battery approach, supplemented with qualitative information and neuroimaging data if possible, is required. Moreover, it would seem unwise on the basis of present data, to combine test scores into a composite measure, as is advised for the BADS, since the overall score may simply obscure useful information provided by the individual subtests rather than adding to the overall sensitivity of the assessment.
In terms of selecting tests for inclusion in an ED test battery, our results indicate that the BADS contains some useful subtests, more sensitive to ED than many of the measures typically used to assess this construct. The Modified Six Elements Test is recommended, along with the Action Program Test. On the basis of our study, additional tests that might be recommended are the Modified Cognitive Estimates Test and the Porteus Maze Test. Other components of the BADS appeared less sensitive to ED, although it should it remembered that, in this study, ED was operationalized on the basis of rating scale scores. It will also be important, when validating new tests or re-examining existing ones, to see which measures are associated with other measures of ED, ranging from ratings scales and existing tests, through to qualitative information and neuroimaging data.
We gratefully acknowledge the participants in this study, who were extremely willing of their time and energy. We also thank the professional raters and family members who contributed to the study.

Correlations between neuropsychological measures and DEX rating scores provided by neuropsychologists and occupational therapists

Factors of neuropsychological functioning extracted by the principal axes method

Standard multiple regression of neuropsychological measures predicting NP- and OT-DEX ratings

Stepwise multiple regression of neuropsychological measures predicting NP- and OT-DEX ratings