Background
According to the US Centers of Disease Control and Prevention (Atlanta, Georgia USA), unintentional injury is the leading cause of death for individuals aged 1-44 years and the fourth leading cause of death overall. 1 Trauma is the leading cause of accidental injury death for individuals aged 5-24 years and the second leading cause of death after unintentional poisoning, a trend that has only recently occurred in the setting of the opioid epidemic. 2 The World Health Organization (Geneva, Switzerland) identifies road injuries as the tenth leading cause of death globally, and the leading cause of injury-related death. 3 Amongst individuals who succumb to trauma, hemorrhage is the major cause of preventable death. It is estimated that hemorrhage accounts for 35.0% of civilian prehospital trauma deaths and 40.0% of deaths in the first 24 hours post-injury.Reference Kauvar, Lefering and Wade 4 Current military data suggest that 91.0% of potentially survivable combat deaths are due to exsanguinating hemorrhage.Reference Eastridge, Mabry and Seguin 5
Until recently, the management of traumatic hemorrhage included large-volume crystalloid fluid administration. There are no compelling data for this approach in the resuscitation of hemorrhagic shock. In fact, there is an increasing body of literature that suggests that this approach may actually be harmful.Reference Haut, Kalish and Cotton 6 , Reference Hussmann, Lefering and Waydhas 7 In 2005, the concept of damage control resuscitation (DCR) as an adjunct to damage control surgery was introduced.Reference Fries and Midwinter 8 - Reference Ball 10 In addition to hemorrhage control, DCR includes targeted hemostatic resuscitation with balanced blood product administration.Reference Stensballe, Ostrowski and Johansson 11 Several recent studies have concluded that earlier DCR improves outcome in both the military and civilian settings.Reference Powell, Hinckley, Gottula, Hart, Lindsell and McMullan 12 , Reference Cotton, Reddy and Hatch 13 As a consequence, blood products have been pushed further forward into the prehospital environment, defined as remote DCR.Reference Fisher, Miles, Cap, Strandenes and Kane 14 - Reference Yann, Habas, Malan, Escarment, David and Peyrefitte 18 A 2016 study demonstrated that 25.3% of Helicopter Emergency Medical Services (HEMS) programs now carry blood.Reference Karl, Pham, Yanosky and Lubin 19
The regional critical care transport service has deployed packed red blood cells (PRBCs) on its HEMS assets since 1988, and fresh thawed plasma since 2009.Reference Stubbs, Zielinski and Berns 20 Currently, blood products are not available on Advanced Life Support (ALS) ground units. The purpose of the current study was to determine whether opportunities for blood product administration by ground ALS ambulances exist within this system.
Methods and Materials
Study Setting
Mayo Clinic Medical Transport (MCMT; Rochester, Minnesota USA) is a comprehensive prehospital care system, including ground (Gold Cross Ambulance Service) and HEMS (Mayo One) assets. Gold Cross Ambulance Service is the sole ALS ground service for the region, responsible for providing both 911 response and inter-facility transportation to a county population of approximately 151,400. The service also provides emergency intercept for regional Basic Life Support (BLS) services. Two hospitals provide emergency services in the ground catchment area; one serves as a quaternary care referral center and Level 1 adult and pediatric trauma center, while the other serves as a community hospital. The latter transfers patients to the former for specialty and sub-specialty evaluation. The study was reviewed and approved by the Mayo Clinic Foundation Institutional Review Board (Rochester, Minnesota USA).
Study Design
This was a retrospective analysis of all MCMT calls for service from January 1, 2011 through December 31, 2015. Subsequent inclusion criteria were:
1. Calls involving scene transport for acute traumatic injury;
2. Priority 1 (emergent) dispatch request;
3. Patient age 18 years or older at time of patient contact; and
4. Predetermined physiological and/or mechanistic criteria corresponding with MCMT guidelines (Figure 1) for potential need for prehospital blood administration.
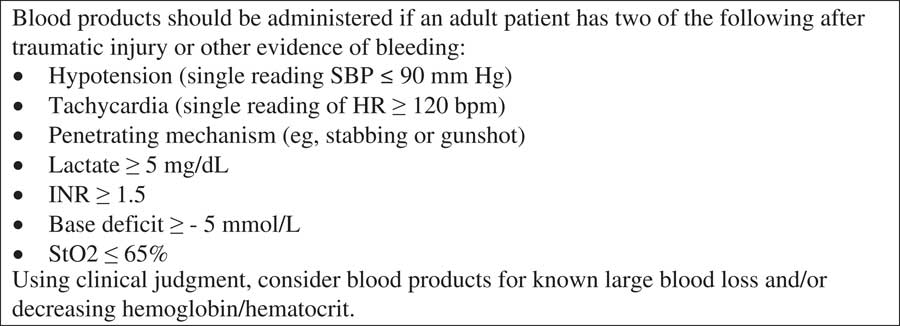
Figure 1 Indications for Blood Product Administration in Trauma Patients. Abbreviations: HR, heart rate; INR, international normalized ratio; SBP, systolic blood pressure; StO2, oxygen saturation.
Physiological criteria included heart rate (HR)≥120 beats per minute and/or systolic blood pressure (SBP)≤90 mmHg, while the mechanistic criterion was penetrating trauma.
Exclusion criteria included:
1. Inter-facility transports; and
2. Age less than 18 years at time of patient contact.
From the identified patient cohort, individual patient care reports were reviewed for all cases, and patients with minor mechanisms of injury (MOIs) not expected to result in significant hemodynamic (HD) derangement were excluded from further analysis.
The MCMT patient names, dates of birth, and service dates were identified and cross-referenced with the Mayo Clinic electronic medical record in order to identify and link any patient with a Mayo Clinic account. For patients transported by ALS ground service, emergency department (ED) trauma records were reviewed to determine whether blood products were administered in the ED, and if administered, the type and quantity. For patients transported by HEMS, the patient care report was reviewed to determine whether blood products were administered en route, as well as type and quantity.
Primary Data Analysis
Data were entered into a Microsoft Excel database (Microsoft Excel for Mac 2011, v 14.5.3; Redmond, Washington USA). Descriptive analyses were generated. Two-sided chi-square and two-sample t tests were used to compare groups, with an alpha level of 0.05 considered statistically significant.
Results
Over the 5-year study period, 7,900 ground ALS transports met inclusion criteria for scene trauma activations (Figure 2). Of these, 843 were categorized as Priority 1 based upon dispatch complaint. An analysis of these patients indicated that 420 met predefined HD parameters, most often tachycardia. Review of the patient care report demonstrated that 53 (0.7%) of these patients had a significant MOI based upon the described mechanism. Fifty-one of these patients had a known outcome. Two were transported to external facilities, and as a consequence, were lost to follow-up. Of these 51 patients, 17 received blood product transfusions in the ED as part of the initial resuscitation. Patients meeting HR and SBP criteria were most likely to receive blood products in the ED (53.3%).

Figure 2 Patient Inclusion Diagram for Patients Receiving Ground Transport, including Breakdown Based Upon Hemodynamic Criteria. Abbreviations: ED, emergency department; HD, hemodynamic; HR, heart rate; MOI, mechanism of injury; SBP, systolic blood pressure.
Clinical characteristics and outcomes of the ground ALS patient cohort are shown in Table 1. A statistically significant difference in total patient contact time (defined as time on-scene and during transport to final destination) was noted, with the HR and SBP group having the longest total patient care time. Penetrating trauma accounted for approximately 25.0% of this severe injury cohort. Of the 13 patients with penetrating trauma, one was lost to follow-up. Although all patients with known outcomes were eventually transfused, either in the intensive care unit or the operating room (OR), only one patient in each group received blood products in the ED. No difference in transfusion rate was noted between penetrating and blunt trauma patients (P=1.0). Thirty-seven percent of patients went from the trauma resuscitation suites to the OR, with the largest proportion occurring in the isolated hypotension group. Although not statistically significant, there was a trend to increasing mortality with worsening HD parameters. The majority of patients received PRBCs as the resuscitative blood product.
Table 1 Clinical Characteristics of Final Ground Patient Cohort Stratified by HD Criteria

Abbreviations: GCS, Glasgow Coma Scale; HD, hemodynamic; HR, heart rate; OHTCA, out-of-hospital traumatic cardiac arrest; OR, operating room; PRBC, packed red blood cells; SBP, systolic blood pressure.
During the 5-year study period, there were 735 HEMS trauma transports, of which, 45.0% were scene flights (Figure 3). In all, 74 (10.1%) patients met HD and mechanistic criteria for blood product administration equivalent to those available to ground ALS services. Of 70 patients with known outcome, 28 (40.0%) received prehospital blood product administration. There was a trend to increasing blood product use as physiologic severity increased, with 60.0% of patients with both HR and SBP parameters receiving transfusion.

Figure 3 Patient Inclusion Diagram for Patients Receiving Helicopter Transport, including Breakdown Based Upon Hemodynamic Criteria. Abbreviations: HD, hemodynamic; HEMS, Helicopter Emergency Medical Services; HR, heart rate; SBP, systolic blood pressure.
Clinical characteristics and outcomes of the HEMS patient cohort are shown in Table 2. No difference in total patient contact time was noted amongst the three HD groups. Penetrating trauma was much less common in the HEMS severe injury cohort, accounting for four percent of patient MOI. Of the three patients with penetrating trauma, two were transfused during HEMS transport. Both of these patients were in the HR+SBP group, while the third patient had a heart rate≥120. The majority of patients received PRBCs for resuscitation.
Table 2 Clinical Characteristics of Final Helicopter Patient Cohort Stratified by HD Criteria

Abbreviations: GCS, Glasgow Coma Scale; HD, hemodynamic; HR, heart rate; OHTCA, out-of-hospital traumatic cardiac arrest; OR, operating room; PRBC, packed red blood cells; SBP, systolic blood pressure.
No statistically significant difference in mean total patient contact time for ALS ground and HEMS transport was noted in the HR+SBP cohort, although the mean ground ALS time was 4.9 minutes shorter than the HEMS time (Table 3). Statistically significant total patient contact time differences were noted for both the HR and the SBP cohorts. Two HEMS patient transports were performed by ground due to weather. The first was a blunt trauma patient who presented with lowest SBP 83 mmHg, had a transport time of 43 minutes, and did not receive blood products. The second blunt trauma patient transport had a maximal HR of 127 bpm, a transport time of 27 minutes, and did receive blood products.
Table 3 Comparison of Total Patient Care Times (minutes), Ground versus Helicopter Transport, Stratified by HD Criteria

Abbreviations: HD, hemodynamic; HR, heart rate; SBP, systolic blood pressure.
Discussion
The management of traumatic shock in the latter-half of the twentieth century involved the administration of intravenous crystalloid solution, with re-assessment and re-administration as needed to obtain normotension. In the 1990s, animal and human studies suggested that such an approach did not improve outcomes and might be harmful.Reference Capone, Safar, Stezoski, Tisherman and Peitzman 21 - Reference Bickell, Wall and Pepe 23 Based upon these studies, the concept of permissive hypotension (hypotensive resuscitation) until definitive surgical management was promulgated. During this same period, acidosis, hypothermia, and coagulopathy were recognized as the lethal triad of acute traumatic injury.Reference Brohi, Singh and Heron 24 - Reference Blackbourne 26
Damage control resuscitation is a systematic approach to the management of acute traumatic shock, designed to mitigate the lethal triad through a combined approach of early hemorrhage control, hypotensive resuscitation, hypothermia prevention, and hemostatic resuscitation with fixed ratio blood product transfusion rather than crystalloid administration.Reference Ball 10 , Reference Holcomb, Jenkins and Rhee 27 , Reference Smith and Pittet 28 Studies have suggested improved outcomes amongst patients receiving DCR strategies.Reference Powell, Hinckley, Gottula, Hart, Lindsell and McMullan 12 , Reference Cotton, Reddy and Hatch 13 As a consequence, efforts have been made to push the concept of hemostatic resuscitation further into the prehospital environment.Reference Fisher, Miles, Cap, Strandenes and Kane 14 - Reference Strandenes, De Pasquale and Cap 16
In the current study, prehospital blood product administration was rare. Of the 7,900 ground ALS transports identified in the study, 53 (0.7%) met criteria for blood product administration. During the same time period, there were 735 HEMS transports, of which 74 (10.1%) met criteria for blood product administration.
Of the 51 ground ALS transports with known outcome, only one-third received blood in the ED. Although there was a trend towards blood product administration based upon physiological severity (HR+SBP>SBP alone>HR alone), this was not statistically different. A similar trend was noted for mortality. Twenty-eight (40.0%) of the 70 HEMS cases with known outcomes received blood products. In the HEMS cohort, statistically significant increased mortality was noted amongst patients with isolated hypotension, although patients presenting with both tachycardia and hypotension were most likely to receive blood.
In order to administer blood products, the patient must first receive vascular access. This, in conjunction with other patient interventions, has an opportunity cost in terms of available time. The mean total patient contact time (on-scene and transport) was consistently longer in the HEMS cohort than in the ground ALS cohort, ranging from 4.9 to 13.0 minutes. In general, HEMS personnel represent the highest skill levels amongst prehospital care providers. In addition, the HEMS medical crew solely perform patient care, with a dedicated pilot(s) to operate the aircraft, as opposed to ground ALS teams in which one of two crew members will likely operate the ambulance. Despite additional time, patient care resources, and availability of blood products, only 40.0% of HEMS patients received transfusions in the prehospital environment.
The delivery of blood products is associated with significant logistical and regulatory constraints, in order to ensure patient safety and product stability. Ideally, products under transport should be stored in refrigerators with a temperature range of +4 (± 2)°C.Reference Stubbs, Zielinski and Berns 20 , Reference Basu and Kulkarni 29 Transport coolers may be used for brief periods of time, but they require vigilance for return of product within a narrow window period. One possible development that may simplify use of prehospital blood product administration is the future availability of freeze-dried plasma.Reference Shuja, Shults and Duggan 30 - Reference Lee, Van and Spoerke 32 Recent civilian and military studies suggest that higher ratios of fresh frozen plasma to PRBCs in DCR improve clinical outcomes.Reference Zehtabchi and Nishijima 33 - Reference Holcomb, Tilley and Baranjuk 37 However, these studies did not determine the specific order in which component blood products should be administered.
Limitations
This study is subject to a number of limitations. As with any retrospective analysis, it is prone to biases, including selection bias and misclassification bias. Initial patient stratification was predicated on Priority 1 dispatch. Patients under-triaged as a lower dispatch priority might have received blood products in the ED, but would not have been identified in this study, thereby decreasing the actual potential utility of prehospital blood product administration.
Nearly five percent of the patients in the final study cohort were lost to follow-up due to transport to an external facility, with two-thirds occurring in the hypotensive groups most likely to require transfusions. Only a single Emergency Medical Services (EMS) system was evaluated. The geography and MOIs noted in this study may not be generalizable to other systems. Each EMS system is unique and should be viewed as such. Other US ground ALS agencies have recently initiated prehospital blood transfusion protocols transfusions. 38 , 39
The current study specifically evaluated trauma patient transport from the scene. Specific criteria have been developed for prehospital blood transfusion by HEMS providers (Figure 1). As written, the guidelines require that two or more criteria be met in order to administer blood products. Much of these data are unavailable to ground ALS units performing scene transports. The current study simplified the guidelines to the presence of a single criterion – either SBP≤90 mmHg or HR≥120 bpm. This simplification has the potential to over-estimate the need for blood product administration. Alternatively, the lack of ancillary data may result in under-estimation of need for blood product administration. Including inter-facility transports would have permitted use of the broader guidelines. However, it is unlikely that ALS ground transport would be used for inter-facility transport of trauma patients requiring blood product administration.
The patient care reports had sparse documentation in terms of medical decision making. Use of blood products was noted, but rationale for use, and more importantly for omission, was not recorded. This information would be critical in determining the real-world feasibility of blood product administration by ground units, given that clinical judgment is an independent criterion for blood product administration.
Conclusions
In this study population, HD parameters alone did not predict subsequent ED blood product administration for trauma patients transported directly from the scene by ground ambulance. Total patient care times were longer in patients transported by HEMS as compared to ground ALS. Despite these time differences and the availability of blood products, only one-third of HEMS patients meeting HD criteria for blood product administration received prehospital transfusion. Less than one percent of scene trauma ground ALS patients would be anticipated to require blood product administration. Given the complex logistical and regulatory requirements involved in blood product storage and administration, there appears to be limited utility within the described ground system.








