Introduction
Since the inception of modern Emergency Medical Services (EMS), advanced airway management, including supraglottic airway devices, endotracheal intubation (ETI), needle cricothyrotomy, and surgical cricothyrotomy, have been a cornerstone of practice. While one of the key tenants of prehospital care remains ensuring adequate ventilation and oxygenation, the definition of what constitutes a secure airway has been highly debated in EMS literature.Reference Fevang, Perkins, Lockey, Jeppesen and Lossius 1 In the control of a hospital setting, ETI has been accepted as the gold standard for a secure airway and is established as soon as possible for the most ill or injured patients. In theory, this would make ETI a natural candidate for application in the field by highly trained EMS providers.Reference Jacobs and Grabinsky 2
The polarized discussion in EMS literature about the usefulness and safety of ETI may be more a function of system-level variables rather than patient-level variables that are often scrutinized to make correlations between ETI usage and patient outcomes.Reference Lockey, Crewdson and Lossius 3 One system factor may be the number of exposures that individual EMS personnel have with ETI attempts.Reference Pepe, Roppolo and Fowler 4 Repetitive exposure has been shown to positively correlate with ETI success.Reference Bernhard, Mohr, Weigand, Martin and Walther 5 Considering the low proportion of patients seen by EMS that require ETI, the rate of ETI exposures a single paramedic may have during a year is likely too low to maintain proficiency with the skill. This issue is amplified in the pediatric population, which makes up an even smaller proportion of patients seen by EMS providers.Reference Mitchell, White, King and Wang 6 Despite numerous studies, ETI has yet to be established as a superior secure airway, and may be detrimental when compared to basic airway skills such as bag-valve-mask (BVM), especially in the pediatric patient.Reference Mitchell, White, King and Wang 6 – Reference Ostermayer and Gausche-Hill 11
The primary objective of this study was to describe a pediatric cohort of patients requiring airway management upon arrival to two pediatric emergency departments (PEDs). The secondary objective included assessing for severity-adjusted associations between EMS airway management technique and patient outcomes. The study cohort consisted of scene trauma and medical transports arriving by EMS to two PEDs that are located in a large metropolitan area serviced by numerous and diverse air and ground EMS agencies.
Methods
Study Design and Setting
A retrospective chart review was performed of a continuous sample of pediatric patients transported directly from the scene by EMS who required airway support upon, or shortly after, arrival to two PEDs. The primary enrolling center was Children’s Medical Center Dallas, a pediatric Level I trauma center centrally located in the Dallas, Texas (USA) metroplex that serves over 120,000 patients annually in the emergency department. The secondary enrolling center was Children’s Medical Center Plano (Plano, Texas USA), a specialized pediatric emergency center and hospital located in a suburban area that serves over 46,000 patients annually in the emergency department. Both centers are part of Children’s Health (Dallas, Texas USA) with research regulatory oversight provided by University of Texas Southwestern Medical Center Dallas (Dallas, Texas USA) Institutional Review Board.
Study Population
Inclusion criteria included patients less than 18 years old, regardless of etiology, who arrived to either of the PEDs between the dates of May 2015 and July 2016. Patients must have been transported directly to the enrolling PED from the scene by air or ground EMS. Additionally, patients must have also required airway support by EMS or initiated prior to the completion of the physician’s primary assessment upon arrival at the PED. Exclusion criteria included patients missing an EMS patient care report (PCR) in their hospital medical record, or patients who were chronically ventilator dependent. The study was reviewed by the Institutional Review Board that has regulatory oversight of research at both PEDs, and was approved with a waiver of informed consent due to the retrospective nature of the research.
Data Collection and Analysis
Data elements were formally defined and agreed upon by the study authors during study development and prior to the beginning of the retrospective chart review. The electronic medical record (EMR) was electronically queried from flowsheet documentation to identify patients who required airway support upon arrival to the PED. Both PEDs used the same EMR, Epic Systems (Verona, Wisconsin USA), which is linked together allowing for simultaneous querying from both enrolling sites. Electronic flowsheets within the EMR that capture airway support devices as documented by the PED nursing staff were used to identify any patients having received or requiring continuous positive airway pressure (CPAP), BVM, or ETI prior to or upon arrival to the PED. A daily log of PED arrivals by EMS was also reviewed by one author to ensure no patients were missed from the electronic query. Once the list of cases was identified, another author, who was trained in the location of information in the EMR, reviewed the medical record to verify eligibility and extracted the defined data elements. Upon completion of the data extraction, a 10% random sample was assessed to review the accuracy of data extraction, in which no patients had errors during this quality control assessment. Data elements that were not found in the medical record were marked as not-applicable if they were not appropriate for the patient, or missing if they were expected but not found in the documentation. Only cases completely missing an EMS PCR were omitted during the data collection phase.
As part of the standard of care and in compliance with state law, EMS providers furnish receiving hospitals with a copy of their completed PCR. The PCR then becomes part of the patient’s hospital record and is stored as a portable document format, also known as a PDF, within each patient’s EMR. The PCR was manually reviewed to extract EMS provider information such as mode of transport, patient complaint, initial assessment, vital signs, treatments, and response to treatments. The patient’s hospital record was reviewed to extract the emergency department care record, physician assessments, nursing assessments, treatments, radiology results, lab results, and hospital disposition.
Airway management provided by EMS was categorized as basic or advanced based on documentation in the PCR. Basic EMS airway management sub-categories included passive management (airway monitoring, positioning, or supplemental oxygen), BVM ventilation, and CPAP. Presence of nasopharyngeal airway (NPA) or oropharyngeal airway (OPA) adjuncts was also recorded. Advanced EMS airway management sub-categories included supraglottic airways (laryngeal mask airway/LMA or King Airway [King Systems; Indianapolis, Indiana USA]) and ETI. During descriptive and outcome analysis, patients with failed prehospital advanced airway attempts who were ultimately managed with basic interventions by EMS were classified as receiving the advanced airway intervention, unless otherwise noted. An attempted advanced airway was considered as any documentation by EMS of insertion of a laryngoscope blade, endotracheal tube (ETT), or supraglottic device into the oropharynx.
The PED documentation of initial vital signs and the initial assessment were both used to determine if a patient was adequately oxygenated upon arrival to the PED. Patients were categorized as inadequately oxygenated if they had an initial PED oxygen saturation of less than 80%, or showed documented signs of poor oxygenation such as cyanosis, or inadequately supported respiratory effort as assessed and documented by physician, nursing, or respiratory staff upon presentation to the emergency department.
Outcome measures consisted of successful placement of an advanced airway in the prehospital setting when attempted by EMS, adequate oxygenation upon PED arrival, and mortality. Successful placement of an advanced airway was confirmed with either physician assessment or radiology confirmation. An advanced airway was considered misplaced if it required positional manipulation in the PED. Supraglottic airways that were confirmed as successfully placed, but replaced with ETI because of physician preference, were considered as successfully placed advanced airways.
Data were collected into a computerized abstraction form using a Microsoft Excel (Microsoft Inc.; Redmond, Washington USA) spreadsheet that was formatted in accordance with the defined data definitions. Analysis and data visualizations were performed with an Anaconda Distribution of Python (Anaconda Inc.; Austin, Texas USA) version 3.512 with the addition of the “Statsmodels” library.Reference Seabold and Perktold 13 Descriptive statistics are presented with counts and percentages, average and standard deviations (SD), or median and inter-quartile ranges (IQR), as appropriate. Chi-square, or Fisher’s Exact when appropriate, were used to assess for significant rate differences between comparative groups. A Mann-Whitney U test was employed to test differences between groups for ordinal variables. Due to mortality rate in sub-groups exceeding 30%, risk-ratio (RR) of mortality was calculated with a general linear model regression with binomial outcome and log-link.Reference Cummings 14 The regression model was used to control for patient severity in comparisons of mortality between groups. A two-tailed P value threshold of less than .05 was used for significance throughout statistical analysis.
Results
A total of 131 patients arrived via EMS to the two participating PEDs during the study timeframe and required initial or continued airway support upon arrival. Twenty-seven (21%) patients did not have an EMS PCR within their medical record and thus were excluded from the study. Twenty different EMS agencies transported the remaining 104 patients, 80 (77%) by ground and 24 (23%) by air. On average, a unique EMS unit transported an eligible patient to one of the two emergency departments less than twice, with a maximum of five patient encounters for a single EMS unit during the allotted study time period. The patients’ average age was 5.9 (SD=5.1) years with a median initial EMS Glasgow Coma Scale (GCS) of nine (IQR 3-14). Overall, EMS providers utilized basic airway management more often than advanced airway management (70% vs 30%; P <.001), and basic management was the method of choice in patients with a documented initial complaint of seizure (92%) or respiratory issues (94%). Demographics of the study cohort including age, EMS airway management, transporting agency, and chief complaint can be seen in Table 1.
Table 1 Patient Demographics
Abbreviations: BVM, bag-valve-mask; CPAP, continuous positive airway pressure; EMS, Emergency Medical Services; ETI, endotracheal intubation; GCS, Glasgow Coma Scale; LOC, level of consciousness.
Seventy-three patients (70%) received basic airway management. Forty-nine (67%) of these consisted of passive airway interventions such as oxygen via mask or direct patient observation, despite the fact they required CPAP or ETI interventions upon arrival to the PED. Only one of the passively managed patients had documented usage of an NPA by EMS. The remainder of the basic airway management group consisted of 22 patients supported by BVM in the field, in which 12 received ETI upon arrival to the PED while the other 10 received only BVM support during their initial presentation to the PED. Eight (36%) of the 22 patients managed with a BVM by EMS had documented usage of an NPA or OPA. The final two basic airway management patients received CPAP by EMS and were continued on CPAP after arrival to the PED.
Organized by EMS airway management method and grouped by basic and advanced methods, Figure 1 shows the overall count of patients for each method on the left side bar graph. On the right side of Figure 1, the definitive PED airway management method that was used is shown as a percent of the corresponding EMS airway management method sub-groups.
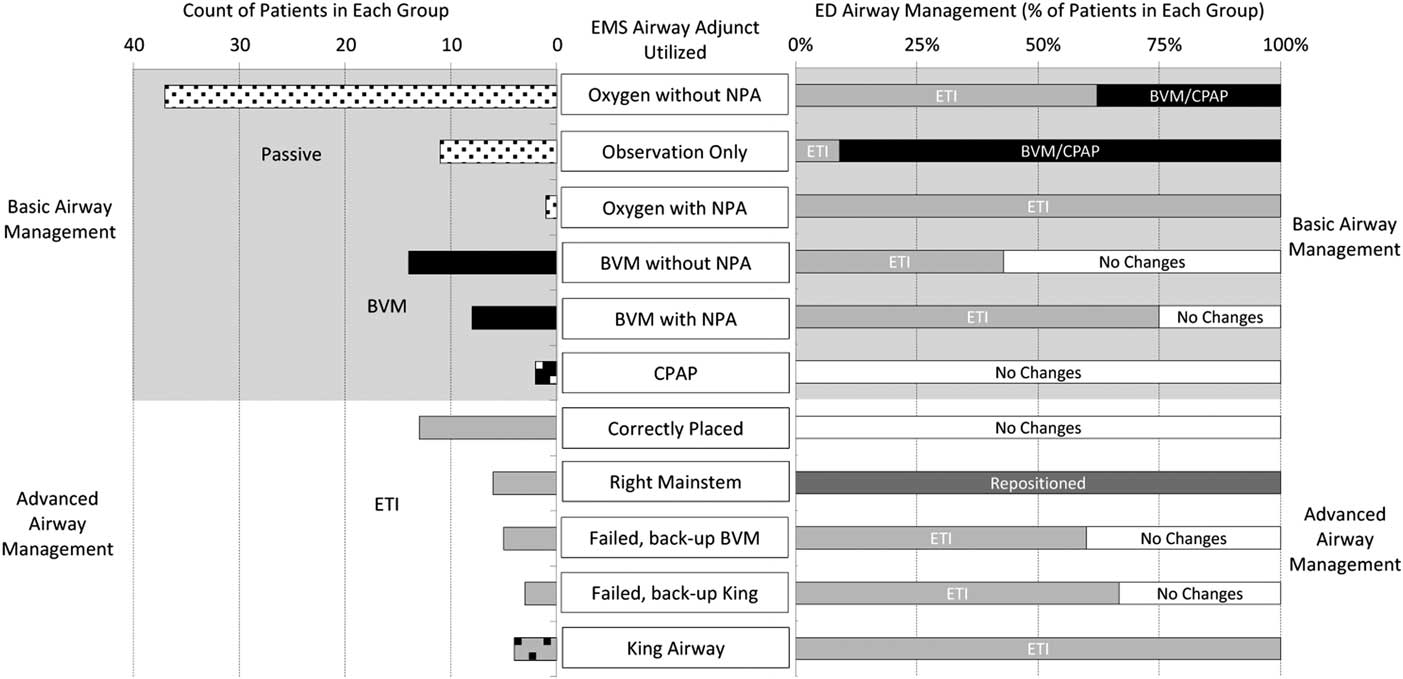
Figure 1 Prehospital Airway Management and Resulting ED Management. Note: Patients grouped by prehospital airway management that was received. Basic management consisted of passive (oxygen or observation) and BVM or CPAP utilization. Advanced management included ETI and supraglottic airways. Definitive airway management as performed by the receiving emergency department is seen on the right side as a percentage of the corresponding count in each group. Definitive care consisted of continuing prehospital care with no significant changes, repositioning of advanced airway, BVM/CPAP, or endotracheal intubation. Abbreviations: BVM, bag-valve-mask; CPAP, continuous positive airway pressure; EMS, Emergency Medical Services; ETI, endotracheal intubation; ED, emergency department; NPA, nasopharyngeal airway; OPA, oropharyngeal airway.
Advanced airways were attempted for the remaining 31 patients (30%). Advanced airway management attempts consisted of supraglottic airways in four patients (13%) and ETI in 27 patients (87%). When supraglottic airways were utilized as the primary EMS advanced airway, no documented issues were noted in the PCR, all patients arrived in the PED with adequate oxygenation, and all had a correctly placed airway. The 27 patients who underwent ETI resulted in 13 (48%) correct placements requiring no changes upon PED arrival, six (22%) that were repositioned from the right mainstem upon PED arrival, and eight (30%) patients had futile ETI attempts requiring use of a rescue airway in the EMS setting. No patients presented to the PED with an esophageal ETI placement. Rescue airways for the eight failed ETI attempts consisted of BVM with no NPA or OPA for five patients and supraglottic airway placement in three patients. Two of the patients who were managed with BVM after futile ETI continued to receive BVM until able to maintain their own airway after arrival at the PED. The remaining three BVM, and three supraglottic airway placements after failed ETI, received ETI in the PED. All supraglottic airways that were inserted by EMS either as first line or rescue airways were documented as King Airway Devices.
Shown in Figure 2, upon reviewing the PCR, adequate documentation to determine justification for ETI attempts were missing in nearly one-half of the patients in which EMS attempted an advanced airway. When documented, fluid in the airway was the most frequently documented reason for ETI attempts. Assistive devices such as video laryngoscopy were utilized in two of the patients, with 10 patients having documented use of a Bougie device (Anaesthetics India Private Limited; Mumbai, India). Twenty-five (93%) of the ETI attempts recorded the number of placement attempts with an average of 1.6 (0.8) attempts. The maximum number of attempts was four, with 11 patients (44%) having multiple attempts documented in the PCR. Patients who experienced an ETI failure averaged two (SD=1.1) attempts with a maximum of four before declaring the prehospital ETI attempt as failure. The selection of ETT size was often within one-half size of recommendations, as shown in Table 2, but was often placed too deep for the selected size as documented by EMS. Of the 25 patients with available documentation, 11 (44%) were documented as being placed in the trachea on the first attempt and two of these patients required repositioning upon arrival to the PED.

Figure 2 EMS Documented Justification for Endotracheal Intubation Attempts. Note: Justification for intubation attempts as documented by EMS in the 27 patients in which endotracheal intubation was attempted. Abbreviations: BLS, Basic Life Support; CHI, closed head injury; EMS, Emergency Medical Services.
Table 2 ETT Size and Insertion Depth Versus Recommendations c

Abbreviations: EMS, Emergency Medical Services; ETT, endotracheal tube; PCR, patient care report.
a ETT size recommendation: ETT Size=(age in years/4)+4.
b Insertion Depth Recommendation: Depth=ETT Size Used x 3.
c Insertion depth was recorded as documented by the EMS provider. Recommended depth was calculated based on the documentation of ETT size in the PCR.
Excluding eight patients where an initial GCS was not documented in the PCR, patients with an initial prehospital GCS less than or equal to eight were more than likely to undergo an advanced airway attempt than those with a GCS over eight (55% vs 10%; P<.001). Outcomes and prehospital airway management stratified by initial GCS scores as documented by EMS are presented in Table 3. The sub-grouping of trauma and medical patients is also presented in each GCS strata. Trauma and medical patients presented to EMS with similar initial GCS scores (7 [IQR 3-9] vs 10 [IQR 3-15]; P=.091). Although not reaching significance, trauma patients tended to more often be managed with advanced airway attempts by EMS (41% vs 23%; P=.054). Overall, the cohort experienced a mortality rate of 28%. There was no significant difference in mortality rate between trauma and medical patients (33% vs 26%; P=.462).
Table 3 Advanced Airway Utilization and Mortality by EMS Initial GCS
Note: Patients grouped by initial EMS GCS assessment. Percent of trauma or medical sub-group in each GCS stratification are presented as percentage of trauma (n=36) or medical (n=68) cohort.
Abbreviations: EMS, Emergency Medical Services; GCS, Glasgow Coma Score.
After controlling for initial EMS GCS with regression, the patients who underwent prehospital advanced airways attempts showed no significant association with mortality (RR 1.48 [95% CI, 0.86-2.56]; P=.156). Similarly, in the sub-group of trauma patients, there was no GCS adjusted significant association with mortality and EMS advanced airway (RR 0.61 [95% CI, 0.35-1.06]; P=.082). In medical patients, there was a significant GCS adjusted association with increased risk of mortality for those that received EMS advanced airway management (RR 2.98 [95% CI, 1.18-7.56]; P=.021).
Overall, a total of 19 patients (18%) were determined to have inadequate oxygenation upon arrival to the PED. These patients were most often treated with passive airway management by EMS (n=16; 84%). Passively managed patients who presented to the PED with inadequate oxygenation made up 33% of the entire passively managed population. The remaining three patients who arrived at a PED showing signs of inadequate oxygenation were managed with a BVM by EMS, with one of them being a failed ETI attempt that was managed with a BVM as a rescue airway. These three patients constituted only 11% of the population that arrived at the PED receiving BVM as their definitive EMS airway management.
Discussion
Patients who require interventions for airway management have very little tolerance for error. This tolerance for error is further narrowed in the pediatric population. Skillful assessment of the pediatric patient and careful selection of airway management considering all possible iatrogenic effects are necessary for EMS personnel.
Overall, patients receiving basic airway support in this study were shown to have similar outcomes versus advanced airways. Superior outcomes were seen for basic airways in the medical sub-group. Patients were adequately oxygenated upon presentation to the PED 90% of the time when managed with a BVM despite under-utilization of basic airway adjuncts designed to increase airway patency and promote proper ventilation. Proper basic airway management, even in a patient who receives ETI is paramount.Reference Levitan 15 A randomized trial by Gausche, et al showed overall, after re-education on ETI and proper and effective BVM, there was no difference in outcomes between BVM and ETI, but BVM provided superior outcomes in the sub-group of respiratory arrest and child maltreatment.Reference Gausche, Lewis and Stratton 10
The majority of patients who required airway support upon arrival to two different PEDs were managed with only passive airway management in the EMS setting. These patients were more likely to be found with inadequate oxygenation upon arrival to the PED, which required immediate escalation of the airway management by PED providers to prevent further demise, when compared to patients who received more aggressive airway management by EMS (P<.001). This observation may be an effect of the low exposure that individual EMS personnel have with pediatric patients requiring airway support or pediatric emergencies in general. In this cohort, the exposure to pediatric patients requiring emergency airway support was less than two patients in a 15-month period for a single EMS unit, likely meaning that the exposure to pediatric patients with airway emergencies is far too low to adequately maintain proficiency in identifying and managing pediatric airway emergencies.
In this study, the lack of exposure to pediatric ETI is seen in the fact that less than one-half of the patients who underwent ETI attempted by EMS had a properly placed ETT upon arrival to the emergency department, and a first pass proper ETI placement rate less than 40% (which is less than previously published success ranges of 69% to 98% in pediatric and adult literature).Reference Jacobs and Grabinsky 2 Also contrary to currently published literature stating unrecognized esophageal intubation rates upon arrival to the PED as high as 17%,Reference Katz and Falk 8 none of the ETI procedures performed by EMS in this study were classified as unrecognized esophageal intubations upon PED arrival.
While EMS ETI is often cited a necessity for long or air-transported patients versus long-term basic airway support,Reference Tollefsen, Brown, Cox and Walls 16 the data revealed that all patients receiving supraglottic airways either as a primary management modality, or secondary to failed ETI, were transported by air or ground without issues in patients as young as 2.4 years old. In addition, in simulated pediatric arrest, supraglottic airways have been shown to be preferred by EMS personnel when compared to ETI.Reference Mitchell, White, King and Wang 6 While the number of attempts was small, all supraglottic airways were successfully placed on the first attempt by EMS and showed no signs of inadequate oxygenation upon PED arrival.
Any type of patient management in the prehospital setting will be subject to the uncertainty that comes with responding to very fluid situations that patients are found in. Despite this uncertainty, procedures with very serious complications that were once reserved for in-hospital patients are taken into the prehospital setting. While these procedures are carefully controlled in the hospital, when they are performed in the prehospital setting, they are subject to the uncertainty that faces the prehospital provider every day. This uncertainty introduces a variation in care from the controlled hospital environment which introduces the possibility for devastating complications.Reference Gausche, Lewis and Stratton 10 While there are understandable differences between a paramedic intubating a pediatric patient at the scene and a pediatric patient being intubated by a pediatric emergency physician in the PED, the patient deserves to hold both providers to the same standard for safety and quality of care.Reference Lockey, Crewdson and Lossius 3 As advanced airways will most likely always play a part in prehospital care, future studies should focus on the physiological differences that are seen in a patient who undergoes advanced airway management in the field versus the emergency department. Efforts should identify the current gap and begin to find ways to minimize this gap in care.
Limitations
As a retrospective review of patient data, this study is subject to several limitations. Despite the current statues that require EMS providers to furnish receiving hospitals with a PCR, there are several logistical barriers to ensuring each patient who is transported by EMS has a PCR correctly inserted into their official medical record. With a majority of study data being sourced from EMS PCRs, patients who were missing a PCR had to be excluded. As a result, 20% of the patients who were otherwise eligible to be included in the study were excluded because of missing EMS PCRs. As often is the case with retrospective chart reviews, not all patients had a complete dataset. Eight patients were missing an EMS GCS, and four patients were missing documentation of the initial ETI depth. These patients were excluded from their respective sub-analysis.
As only one author performed chart abstraction, there was no way to assess inter-rater reliability in this study. Data elements including possible responses and data definitions were defined prior to chart review. Building these definitions into the electronic chart abstraction form, and performing a randomized quality check of the data, furthered the effort to make the data collection as unbiased and objective as possible. While including patients that arrived at two facilities from the scene allowed for maximum capture of patients from two distinct geographies, there is still a population of pediatric patients that were likely taken to other hospitals from the scene and are not represented in this analysis.
Conclusion
Currently, EMS exposure to pediatric airway emergencies remains low, and advanced airway management is still widely used by EMS in severely injured or ill pediatric patients; however, the data show that BVM management by EMS was shown to be effective in maintaining adequate oxygenation for 90% of pediatric patients while advanced management offered no definitive benefits. The majority of patients who arrived inadequately oxygenated to the PED were only managed with blow by oxygen or monitoring by EMS. Even in the metropolitan setting, opportunities exist for furthering research and continuing education on providing adequate prehospital knowledge in the identification and treatment of pediatric patients requiring airway support.







