Introduction
Rigid and excessive avoidance of unpleasant situations, feelings and thoughts can cause negative long-term outcomes (Rochefort et al., Reference Rochefort, Baldwin and Chmielewski2018), and serves a vital role in development and maintenance of psychopathology (Levin et al., Reference Levin, Krafft, Pierce and Potts2018). Avoidance is a risk factor in depressive disorders, anxiety disorders, eating disorders and personality disorders, and it has been suggested that avoidance may be a transdiagnostic factor across psychiatric disorders (Barlow and Farchione, Reference Barlow and Farchione2017; Boelen and Eisma, Reference Boelen and Eisma2015; Wheaton and Pinto, Reference Wheaton, Pinto, Fontenelle and Yücel2019). Thus, accurate assessment of avoidance is critical for both research and clinical practice.
Avoidance has been defined as a coping or problem-solving strategy, experiential component, or as a cognitive behavioural concept. Moos and Schaefer (Reference Moos, Schaefer, Goldberger and Breznitz1993) developed a framework for coping strategies, in which they distinguished cognitive avoidance and behavioural avoidance strategies. Avoidance has also been incorporated into the framework of experiential avoidance, defined as escaping from exposure with particular personal experiences and taking strategies to alter the form or frequency of the events and the contexts that occasion them (Harris, Reference Harris2019).
Ottenbreit and Dobson (Reference Ottenbreit and Dobson2004), defined avoidance as ‘refraining or escaping from, an action, person or thing’ (p. 297). They suggest that avoidance consists of serval dimensions, including cognitive versus behavioural, active versus passive, and social versus non-social, and that the measurement of avoidance should encompass these aspects. Drawing upon theories and research on depression, they developed an integrated, multi-dimensional scale (the Cognitive Behavioural Avoidance Scale: CBAS) to measure avoidance. While this scale was developed in response to need for a trait measure of avoidance in depressive disorders, it can also be used in other forms of psychopathology (Brockmeyer et al., Reference Brockmeyer, Kulessa, Hautzinger, Bents and Backenstrass2015; Ottenbreit et al., Reference Ottenbreit, Dobson and Quigley2014a,b).
The CBAS is a 31-item questionnaire which assesses Behavioural Social (BSA), Cognitive Social (CS), Behavioural Nonsocial (BN) and Cognitive Nonsocial (CN) dimensions of avoidance. Ottenbreit and Dobson (Reference Ottenbreit and Dobson2004) reported that exploratory factor analyses (EFA) of CBAS revealed a four-factor solution, which was consistent with the hypothesized structure of the scale. These factors showed good internal consistency, temporal stability, and convergent and divergent validity (Ottenbreit and Dobson, Reference Ottenbreit and Dobson2004). Since then, the reliability and validity of the CBAS has been examined in several other cultures and populations. Röthlin et al. (Reference Röthlin, Grosse Holtforth, Bergomi, Berking, Ottenbreit and Caspar2010) and Vandromme et al. (Reference Vandromme, Raes, Defranc and Hermans2007) found a similar four-factor structure for the German and the Dutch versions of the CBAS, respectively. The four-factor solution has good internal consistency and test–re-test reliability. A study of a Spanish version of the CBAS showed that the four-factor model best fitted the data (Hernández-Guzmán et al., Reference Hernández-Guzmán, Dobson, Caso-Niebla, González-Montesinos, Epp, Arratíbel-Siles and Wierzbicka-Szymczak2009). Çakir (Reference Çakir2016) also reported that an EFA of data from Turkish students revealed a four-factor solution. All of the factors demonstrated satisfactory internal consistency and temporal stability. Finally, a study of the CBAS in a sample of depressed women (Ottenbreit et al., Reference Ottenbreit, Dobson and Quigley2014a,b) confirmed the reliability and validity of the CBAS.
Although it appears that the four-factor model incorporated into the CBAS is replicable cross-culturally, there is no published evidence about the psychometric properties of the CBAS in Eastern cultures. Thus, the primary aim of the study was to evaluate the psychometric properties of a Persian version of the CBAS. The factor structure was examined with both exploratory (EFA) and confirmatory factor analysis (CFA). The convergent and divergent validity, test–re-test reliability, discriminative validity, internal consistency, and temporal stability of the CBAS were also examined.
Study 1: purpose and design
Study 1 investigated factor structure (via EFA), internal consistency, test–re-test reliability, and divergent and convergent validity of the CBAS. Based on the literature we expected that EFA would reveal a four-factor solution. We hypothesized that the CBAS would demonstrate strong positive correlations with depression and anxiety symptoms and weak or negative association with healthy thought control strategies.
Method
Participants
Participants were 767 students of humanities, engineering, education and agricultural sciences of Imam Khomeini International University, in Qazvin, Iran. They were recruited in the academic year 2016–2017. They did not receive any compensation or gratification for their participation. Sixty-five students missed more than 10% of the items and their data were excluded from analyses. Thus, data from 702 participants (233 males, 469 females) were analysed. The mean age of the males was 22.35 years (SD = 3.88, range = 18 to 51), and corresponding figures for females were 20.79 (SD = 2.15, range = 17 to 41).
Measures
Beck Depression Inventory, second edition (BDI-II)
The BDI-II measures the severity of depressive symptoms (Beck et al., Reference Beck, Steer and Brown1996). It has demonstrated good psychometric properties (McElroy et al., Reference McElroy, Casey, Adamson, Filippopoulos and Shevlin2018; von Glischinski et al., Reference von Glischinski, von Brachel and Hirschfeld2019). The reliability and validity of the scale in an Iranian sample has been demonstrated (Toosi et al., Reference Toosi, Rahimi and Sajjadi2017). In the current study, the internal consistency of the BDI-II was .89.
Cognitive Behavior Avoidance Scale (CBAS)
The CBAS (Ottenbreit and Dobson, Reference Ottenbreit and Dobson2004) is a multi-dimensional self-report measure of avoidance with 31 items. It has four factors including behavioural social avoidance, behavioural non-social avoidance, cognitive social avoidance and cognitive non-social avoidance. Respondents indicate how true the mentioned strategies for coping with stressful situations are for them using a 5-point scale (1 = not at all true for me to 5 = extremely true for me). The items are summarized to provide an overall score that ranges from 31 to 155. Higher scores indicate more avoidance.
Anxious Thoughts Inventory (AnTI)
The AnTI (Wells, Reference Wells1994) is a self-report questionnaire that assesses social worry, health worry and meta-worry. The reliability and validity of the AnTI has been established (Fata et al., Reference Fata, Moutabi, Moloodi and Ziai2010) in Persian samples. Its internal consistency in the current study was .94.
Thought Control Questionnaire (TCQ)
The TCQ (Wells and Davies, Reference Wells and Davies1994) is a 30-item scale that measures using strategies to control intrusive thoughts. The questionnaire contains five subscales including Distraction, Social control, Worry, Punishment, and Reappraisal. The Social control and Reappraisal subscales were employed in the current study, as these subscales are associated with emotional stability and healthy approach to unwanted thoughts. The Persian version of the TCQ has demonstrated good validity and reliability (Fata et al., Reference Fata, Moutabi, Moloodi and Ziai2010). The internal consistency of the Social control and Reappraisal subscales were .72, and .64, respectively, in the current sample.
Procedure
The CBAS was translated into Persian and independently back-translated into English. After some minor revisions, the second author confirmed that the English back-translation of the scale reasonably matched the original version. As a second step, 15 clinical psychologists examined the fluency and cultural adaptations in wording of the scale and suggested a few minor revisions. Finally, the research assistants went to classes and explained the purpose and procedure of the study. Students who signed a written informed consent were asked to complete the questionnaires. After 4 weeks, 504 of these participants completed the CBAS a second time. This procedure was approved by the Ethics Review Board of Imam Khomeini International University, Qazvin, Iran.
Data analyses
EFA was utilized to evaluate the factor structure of the CBAS using SPSS-24 (IBM, 2016). Internal consistency was investigated using Corrected Item-Total Correlations (CITC), alpha if items removed, and Cronbach’s alpha coefficient. Test–re-test reliability, as well as convergent and divergent validity, were examined using Pearson correlation coefficients.
Results
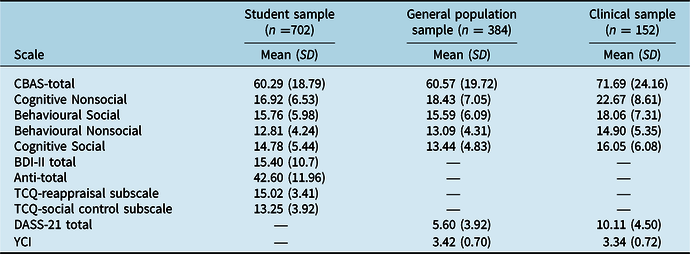
The means and standard deviations for the CBAS, BDI-II, AnTI and TCQ can be seen in Table 1.
Table 1. Means and standard deviations, of the CBAS, BDI-II, AnTI and TCQ-reappraisal subscale, TCQ-social control subscale in student sample, and means, standard deviations and ranges of the CBAS, DASS-21 and YCQ in the general population and clinical samples

CBAS, Cognitive Behavioral Avoidance Scale; BDI-II, Beck Depression Inventory-II; AnTI, Anxious Thoughts Inventory; TCQ, Thought Control Questionnaire; DASS-21, Depression Anxiety Stress Symptom-21; YCI, Young Compensation Inventory; SD, standard deviation.
Internal consistency
All of the CBAS items with one exception showed acceptable item-total correlations (Table 2). Item 3 (‘I like to achieve, but have to accept limits’) showed a weak relationship with the total CBAS (CITC = .21). An excellent internal consistency was found for the CBAS total score (α = .91). Internal consistency of the subscales was as follows: Cognitive Nonsocial = .85, Behavioural Social = .80, Behavioural Nonsocial = .77, Cognitive Social = .76.
Table 2. Factor loading, communalities, item-total correlations, and factor internal consistency scores for principal factor extraction after varimax rotation of the CBAS items

Exploratory factor analysis
The Kaiser-Meyer-Olkin (KMO) coefficient was .93, and the Bartlett coefficient was 7270.95 (p < 0.001). The results, based on the criteria of eigenvalues greater than 1 and screeplot, suggested a four-factor solution. The four factors accounted for 51% of the total variance (Table 2). Varimax rotation revealed four factors with similar item loadings to the original version, but with a few differences. Item 18 (‘Try not think about how to improve performance’) and item 19 (‘Try not think about future/what do with life’) simultaneously loaded on the Cognitive Nonsocial and the Cognitive Social factors. Based on the higher loading factors of these items on Cognitive Nonsocial factor, we placed these two items in the Cognitive Nonsocial factors, which is also in line with the original version of the CBAS. Also, item 13 (‘Avoid trying activities with a potential for failure’) double-loaded on Behavioural Nonsocial and Cognitive Social factors. Again, based on the higher factor loading of the item on Behavioural Nonsocial factor, and the factor structure of original version, we placed it on the Behavioural Nonsocial factor. In addition, item 26 (‘Confusion in relationships, not try figure out’), and item 27 (‘Not think how solve family problems – useless’) loaded on Cognitive Nonsocial factor, whereas these items loaded on Cognitive Social factor in the original version. Item 3 and item 12 (‘Rather than getting out, I sit home watch TV’) did not load on any factor and were deleted from further analysis.
Test–re-test reliability
The 4-week test–re-test reliability of the CBAS was examined, using Pearson correlation coefficients. These results were as follows: CBAS total score (r = .76, p < .001); Cognitive Nonsocial (r = .72, p < .001); Behavioural Social (r = .69, p < .001); Behavioural Nonsocial (r = .73, p < .001); and Cognitive Social (r = .67, p < .001)
Convergent and divergent validity
The total score and all subscales of CBAS showed significant positive associations with both BDI-II (r s = .43 to .57, p < .001), and AnTI (r s = .49 to .61, p < .001), as predicted. In contrast, the CBAS total score and its subscales had low and mostly non-significant relationships with the reappraisal (r s = –.001 to –.09, p > .05) and social control (r s = –.007 to –.02, p > .05) subscales of TCQ. The two correlations that were negatively significant were –.07 (p < 0.01) and –.09 (p < 0.01), and thus accounted for a minimal amount of shared variance (Table 3).
Table 3. Association of the CBAS with BDI-II, AnTI, TCQ, Depression-Anxiety Stress Scale and Young Compensation Inventory

* p<0.01.
** p<0.001.
CBAS, Cognitive Behavioral Avoidance Scale; BDI-II, Beck Depression Inventory-II; AnTI, Anxious thoughts Inventory; TCQ, Thought Control Questionnaire; DASS-21, Depression Anxiety Stress Symptom-21; YCI, Young Compensation Inventory.
Study 2: purpose and design
Study 2 examined the factor structure of the CBAS via CFA, as well as its internal consistency, divergent and convergent validity, and discriminative validity, in a general population and clinical samples. Based on the literature and the results from Study 1, a four-factor model was expected to fit the data. It was hypothesized that the CBAS would demonstrate positive correlations with depression, anxiety and stress symptoms, but no association with compensatory behaviour strategy. Finally, discriminative validity of the CBAS was evaluated by examining whether the scale could successfully differentiate between the clinical and general population samples.
Participants
This study was part of a larger project related to mechanisms of perfectionism. The participants and procedure of the project are described elsewhere (Moloodi et al., Reference Moloodi, Pourshahbaz, Mohammadkhani, Fata and Ghaderi2017). The participants were recruited from the general population and hospital clinics. The general population sample included 403 participants (199 males, 204 females) in Tehran, Iran. They were selected via proportional quota sampling based on the last census data of the Statistical Center of Iran (2011). The mean age of the males was 33.23 years (SD = 9.18) and females 32.71 years (SD = 9.78). Nineteen participants missed more than 10% of the items, and so their data were eliminated from the study, leaving data from 384 participants.
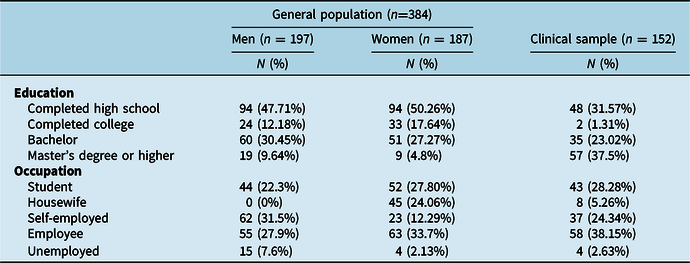
The clinical sample consisted of patients who met the DSM-IV-TR criteria for major depressive disorder (MDD; n = 40, 26 females), obsessive compulsive disorder (OCD; n = 39, 24 females), social anxiety disorder (SAD; n = 35, 26 females) or eating disorder (ED; n = 38 females). The mean age of the four clinical groups was: MDD = 29.87 (SD = 5.94); OCD = 31.25 (SD = 5.52); SAD = 28.37 (SD = 6.37) and EDs = 30.38 (SD = 5.55) (for further demographic characteristics, see Table 4).
Table 4. Demographic information for the sample from the general population and the clinical sample

Method
The general population data were obtained by five social workers, who selected participants according to a quota sampling matrix from visitors in health centres, parks and/or cultural houses. Potential participants were approached, received information about the study, and if they provided written consent, they were asked to complete a battery of questionnaires.
For the clinical sample, psychiatrists and clinical psychologists were invited to refer their patients to the first author (R.M.) for an evaluation using the Structured Clinical Interview for DSM-IV (SCID). Individuals who met the inclusion criteria and agreed to participate in the study were instructed about the questionnaires and requested to complete them in one week. The research procedure was approved by Ethics Review Board of University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Instruments
Depression Anxiety Stress Scales-21 (DASS-21)
The DASS is a 21-item self-report instrument. It has three subscales that measure symptoms of depression (e.g. ‘I felt down-hearted and blue’), anxiety (e.g. ‘I felt I was close to panic’), and stress (e.g. ‘I found myself getting agitated’). Validity and reliability of the DASS-21 has been stablished in Western (Scholten et al., Reference Scholten, Velten, Bieda, Zhang and Margraf2017) and Iranian (Asghari Moghaddam et al., Reference Asghari Moghaddam, Saed, Dibajnia and Zangeneh2008) populations. In current study, the internal consistency of the DASS-21 was .92.
Cognitive Behavior Avoidance Scale (CBAS)
The CBAS is described in Study 1 above.
Young Compensation Inventory (YCI)
The YCI (Young et al., Reference Young, Klosko and Weishaar2003) is a 48-item measure that assesses several forms of schema compensation strategies. Schema compensation is a construct that is significantly different from avoidance, and so this scale was not expected to correlate significantly with CBAS scores. Each YCI item is rated on a 6-point Likert scale from 1 (‘completely untrue of me’) to 6 (‘describes me perfectly’). The YCI has satisfactory validity and reliability (LuKaraosmanoglu et al., Reference LuKaraosmanoglu, Soygut and Kabul2013; Sundag et al., Reference Sundag, Zens, Ascone, Thome and Lincoln2018). The internal consistency of YCI in the current study was .88.
Statistical analyses
Data analysis was performed using SPSS-24 (IBM, 2016, and Amos 23 (Arbuckle, Reference Arbuckle2014). First, the necessary assumptions for running parametric analyses (e.g. normal distribution) were checked using descriptive statistics. In order to test the proposed four-factor model of CBAS, CFA with maximum likelihood estimation and fixing a factor loading to 1 method was performed using Amos 23. The results of the CFA were examined by a variety of goodness-of-fit indices, including χ2, the goodness-of-fit index (GFI), adjusted goodness-of-fit index (AGFI), incremental fit index (IFI), comparative fit index (CFI), and the root mean square error of approximation (RMSEA). Internal reliability was examined using Cronbach’s alpha. The convergent and divergent validity of the CBAS were assessed by Pearson correlation coefficients, while its discriminative validity was investigated using univariate analysis of variance between the community and clinical samples.
Results
The means and standard deviations for the CBAS, BDI-II, AnTI and TCQ can be seen in Table 1.
Confirmatory factor analysis
CFA was used to examine the proposed four-factor model of CBAS. Furthermore, based on the dimensional nature of avoidance (Ataie et al., Reference Ataie, Fata and Ahmadi Abhari2014), the data of the general population and clinical samples were pooled for a total n of 536. The goodness-of-fit indices showed that the four-factor model showed a good fit with the data (χ2 (2) = 2.91, p = .0001, GFI = .93, AGFI = .90, IFI = .90, CFI = .90, RMSEA = .05, 90% CI [.05, .06]) (see Fig. 1).

Figure 1. Confirmatory factor analysis of CBAS in general population and clinical samples. The standardized regression weight is reported.
Internal consistency
All of the items except item 3 indicated satisfactory item-total correlations. Item 3 (‘I like to achieve, but have to accept limits’) showed a weak relationship with the total score (CITC = .13). All items except item 3 made a significant contribution to the internal consistency of the CBAS, using item-removed-analysis. The internal consistency of the CBAS total was .93. The internal consistency of the subscales was as follows: Cognitive Nonsocial, α = .85, Behavioural Social, α = .84, Behavioural Nonsocial, α = .74, Cognitive Social, α = .78.
Convergent and divergent validity
As shown in Table 3, the CBAS and its subscales yielded significant positive associations with DASS-21 (r s = .40 to .58, p < .001) scores, and in both the general population and clinical samples. In contrast, the CBAS and its subscales did not correlate with Young Compensation Inventory scores (r s = .02 to .09, p > .05).
Discriminative validity
In order to evaluate the discriminative validity of the CBAS, the scores of general population (N = 384) and a pooled clinical sample (N = 152) were compared through ANOVA. This analysis indicated that the pooled clinical group had significantly higher scores on the CBAS total and its four subscales than the general population (Table 5). Subsequent ANOVAs between the specific clinical groups failed to reveal significant differences for either the CBAS total scores or any of the four subscales suggesting that the CBAS has value in multiple diagnostic groups (Table 5).
Table 5. CBAS total and its subscales scores of general population and clinical samples

* F is between the general population and the total clinical sample. The degrees of freedom for the F-test was between the general population and the total clinical sample (1534).
** F is between the MMD, OCD, SAD and EDs groups. The degrees of freedom for the F-test was between the clinical subsamples (3148). CBAS, Cognitive Behavior Avoidance Scale; MDD, major depressive disorder; OCD, obsessive compulsive disorder; EDs, eating disorders; SAD, social anxiety disorder.
Discussion
The current studies examined the reliability and validity of the Persian version of the CBAS in Iranian culture. Factor analyses revealed a four-factor solution for the CBAS in a large Iranian student sample. The content of the factors was similar to the original version of the CBAS and therefore these factors were validated. Our results are generally consistent with previous literature (Çakir, Reference Çakir2016; Ottenbreit and Dobson, Reference Ottenbreit and Dobson2004; Ottenbreit et al., Reference Ottenbreit, Dobson and Quigley2014a,b; Vandromme et al., Reference Vandromme, Raes, Defranc and Hermans2007), although some differences were observed. In other words, item 26 (‘Confusion in relationships, not try figure out’), and item 27 (‘Not think how solve family problems – useless’) loaded on Cognitive Nonsocial factor, rather on Cognitive Social factor. The content of these discrepant items might imply that in Iran the items reflected an intrapersonal process of avoiding social problems. It might be a noteworthy hypothesis to investigate cultural differences in future research.
The current results also demonstrated that the four-factor model of the CBAS fitted the data from the clinical and general population samples. These results were in line with previous studies (Hernández-Guzmán et al., Reference Hernández-Guzmán, Dobson, Caso-Niebla, González-Montesinos, Epp, Arratíbel-Siles and Wierzbicka-Szymczak2009; Röthlin et al., Reference Röthlin, Grosse Holtforth, Bergomi, Berking, Ottenbreit and Caspar2010), which showed that the four-factor model provided the best fit with data. Finally, in line with previous research (Çakir, Reference Çakir2016;Ottenbreit and Dobson, Reference Ottenbreit and Dobson2004; Hernández-Guzmán et al., Reference Hernández-Guzmán, Dobson, Caso-Niebla, González-Montesinos, Epp, Arratíbel-Siles and Wierzbicka-Szymczak2009; Ottenbreit et al., Reference Ottenbreit, Dobson and Quigley2014a,b; Röthlin et al., Reference Röthlin, Grosse Holtforth, Bergomi, Berking, Ottenbreit and Caspar2010; Vandromme et al., Reference Vandromme, Raes, Defranc and Hermans2007), the CBAS and its subscales showed good internal consistency in both studies as well as temporal stability. While the temporal stability of CBAS scores over a 4-week period provides some evidence for the stability and trait conceptualization of avoidance, a longer time frame is needed to demonstrate trait nature of avoidance (Ottenbreit and Dobson, Reference Ottenbreit and Dobson2004).
The convergent validity of the CBAS was verified through the positive significant correlations of the CBAS and its subscales with depression, anxiety, stress symptoms and anxious thoughts. These results are consistent with research that demonstrated the relationship between the CBAS and indices of depression and anxiety (Ottenbreit et al., Reference Ottenbreit, Dobson and Quigley2014a,b; Röthlin et al., Reference Röthlin, Grosse Holtforth, Bergomi, Berking, Ottenbreit and Caspar2010), and in line with theories that postulate avoidance as a central feature of anxiety (Barlow et al., Reference Barlow, Allen and Choate2016; Hofmann and Hay, Reference Hofmann and Hay2018) and depressive disorders (Quigley et al., Reference Quigley, Wen and Dobson2017).
The CBAS did not correlate with healthy thought control strategies and compensatory behaviour strategy. Ottenbreit and Dobson (Reference Ottenbreit and Dobson2004) reported negative relationships between CBAS scores and behavioural and cognitive coping approaches. In addition, the CBAS did not correlate with compensatory behaviour strategy. Our findings indirectly support schema theory (Young et al., Reference Young, Klosko and Weishaar2003), which suggests that avoidance and overcompensation are distinct coping styles.
The CBAS and its subscales were able to distinguish a diverse clinical sample from a general population. These results confirmed the discriminative power of the CBAS and indirectly support the dimensional nature of avoidance. In addition, ancillary ANOVA analysis to compare patients with MDD, OCD, EDs and SAD showed that the four clinical groups did not differ significantly on the CBAS and its subscale scores, which implies that avoidance has a transdiagnostic role in these psychopathologies.
This study had several strengths, but also some limitations. An important strength was the size of the samples recruited from a student population, from the general population, and from a clinical context. Another strength was the use of number of validated scales to explore convergent and divergent validity of the CBAS. This said, the mere use of self-report instruments is a limitation of the study. Second, except for the test–re-test analyses in Study 1, the results reported here are correlational and cannot be used to imply any causation. Longitudinal research is needed to examine the extent to which self-reported avoidance patterns predict future psychological distress.
In essence, our findings contribute to further research to explore the predictive validity of avoidance in depression and other psychiatric conditions, and to examine the extent to which changes in avoidance in clinical populations might predict recovery, or play a role in relapse prevention. The current focus on behavioural activation treatments in the area of depression (Dobson and Dobson, Reference Dobson and Dobson2018) suggests that addressing avoidance in the therapeutic context is a key aspect of depression treatment (Dobson and Dobson, Reference Dobson and Dobson2018), and the validation of the Persian CBAS now permits further studies of this important construct.
Acknowledgements
The authors are grateful to the research assistants who collected the data, and all the study participants.
Financial support
Study 2 was supported by the University of Social Welfare and Rehabilitation Sciences, grant number 94/801/T/ 26318. The university did not play a role in design, data collection, data analysis or preparation of the manuscript.
Conflicts of interest
The authors have no actual or potential conflicts of interest.
Ethical statement
Informed consent was obtained from all individual participants included in the study. The authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the APA. The research procedure was approved by Ethics Review Board of University of Social Welfare and Rehabilitation Sciences.







Comments
No Comments have been published for this article.