Introduction
Vertigo is the most disabling symptom for patients with Ménière's disease. Chemical labyrinthectomy using gentamicin results in vestibulotoxicity, thereby controlling the vertigo attacks. Aminoglycosides cause ototoxic damage to the dark cells within the stria vascularis, thereby reducing endolymph production.Reference Pender1 Unfortunately, the auditory system is also at risk from aminoglycosides delivered to the inner ear. The risk is less so with gentamicin. This drug can have profound effects on the dark cells before any functional damage is seen in the cochlea or in the vestibular end-organs.Reference Pender1
Transtympanic drug therapy has become increasingly popular in the treatment of Ménière's disease. Various methods of drug delivery have been used.Reference Obholzer and Wareing2 They include direct intra-tympanic injection into the middle ear, injection onto Gelfoam® placed in the round window niche, continuous perfusion using a round window microcatheterReference Suryanarayanan and Cook3 and drug delivery using the Silverstein MicroWick™.Reference Silverstein4
In this paper, we present the long term outcome of patients undergoing gentamicin inner-ear perfusion using the Silverstein MicroWick, in our centre.
Materials and methods
This study was performed retrospectively and assessed the outcome of patients treated with gentamicin perfusion of the labyrinth, using the Silverstein MicroWick, at our centre. The diagnosis of Ménière's disease was made based on the American Association of Otolaryngology-Head and Neck Surgery (1995) criteria for definite Ménière's disease, that is: (1) two or more definitive, spontaneous episodes of vertigo lasting 20 minutes or longer; (2) audiometrically documented sensorineural hearing loss on at least one occasion; (3) tinnitus or aural pressure in the treated ear; and (4) exclusion of other causes.5
All patients underwent a magnetic resonance imaging scan to exclude cerebellopontine angle pathology. All patients initially received medical therapy, including a low salt and low caffeine diet and betahistine, for at least six months. Only those patients who did not obtain significant relief of their symptoms with this medical therapy were treated by chemical perfusion. Three patients had undergone grommet insertion prior to Gentamicin perfusion, without benefit.
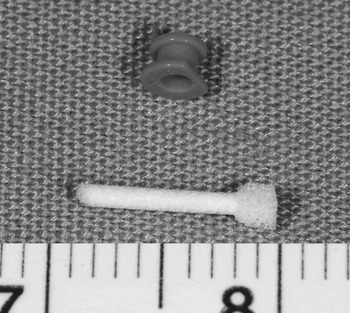
The Silverstein MicroWick (Figure 1) consists of an absorbent sponge and a grommet. The procedure was performed under general anaesthesia as a day case. A posterior myringotomy was performed (Figure 2). Use of a laser reduces the risk of bleeding, although this is not essential. The myringotomy was sited over the expected position of the round window niche.Reference Silverstein, Durand, Jackson, Conlon and Rosenberg6 Through the myringotomy, the round window niche was identified (Figure 3) and freed of any mucosal folds or adhesive bands. The grommet was placed, through which the microwick was inserted and positioned to be in contact with the round window niche (Figure 4). The stiffness of the microwick facilitated this step. The microwick was then primed with gentamicin solution; the microwick swelled, anchoring it snugly in place. The microwick absorbed the drug and transported it across the tympanic membrane and middle ear to the round window niche. A gentamicin concentration of 10 mg/ml was used, made up by a pharmacist each time.

Fig. 1 Silverstein MicroWick and grommet.

Fig. 2 Operating microscope view of posterior myringotomy, performed with laser.

Fig. 3 Operating microscope view of round window niche, as seen through the myringotomy.

Fig. 4 Operating microscope view of Silverstein MicroWick with grommet in place.
Post-operatively, patients self-treated using the same solution as ear drops (three drops thrice daily for two weeks). After the treatment, both wick and grommet were removed in the clinic and the myringotomy was allowed to heal. Patients did not undergo sequential audiography during their treatment.
For this study, patients who had undergone the above procedure were asked to complete a questionnaire enquiring about their Ménière's symptomatology, namely, the number of episodes of vertigo, tinnitus and fullness. They were also asked to rate their disability based on a six point functional level scale,5 and to fill in the Glasgow benefit inventory.Reference Robinson, Gatehouse and Browning7 Their case notes were reviewed to obtain details of past symptoms, investigation results and treatments.
The data obtained were analysed as per the American Association of Otolaryngology-Head and Neck Surgery (1995) reporting guidelines.5 The frequency of vertigo (FV) was measured using the following equation: FV = (x/y) × 100 (rounded to the nearest whole number), where x was the number of definitive vertigo spells per month for the last six months of follow up, and y was the average number of vertigo spells per month for the six months before therapy. Pure tone average (PTA) results were obtained by averaging thresholds measured at 0.5, 1, 2 and 4 kHz (3 kHz is not routinely measured in the UK). A PTA change of at least 10 dB was considered significant.
The Glasgow benefit inventory is particularly useful in retrospective studies. This self-assessment questionnaire was designed to measure changes in quality of life as a result of a health care intervention. The scale consists of 18 items, grouped into general, physical and social support subscales. The answers are based on a five-point Likert scale, ranging from a large deterioration to a large improvement. The various subscale scores and the total Glasgow benefit inventory score can be calculated using specified formulae. The scores can vary from −100 (i.e. a large deterioration) to +100 (i.e. a large improvement), with zero signifying no change in quality of life.
Results
The study included 15 patients, who had each completed at least 24 months of follow up. There were nine women and six men, with ages ranging from 41 to 79 years (mean 58 years). Their duration of follow up had varied from 24 to 48 months. Their Ménière's disease was staged as per the American Association of Otolaryngology-Head and Neck Surgery (1995) reporting guidelines, based on the pre-operative PTA. The majority had stage three disease, and three patients had a ‘dead ear’ pre-operatively (i.e. stage four).
Vertigo control
All patients obtained complete resolution of their vertigo symptom initially (Class A). Three patients subsequently changed to class B control at follow up after 10, 26 and 30 months respectively. At the time of this study therefore, complete control (class A) was seen in 80% and class B in 20% of patients.
Functional level
The preoperative functional level varied between level 3 to 6. Post operatively they improved to level 1 to 3 (Figure 5).

Fig. 5 Patients' reported levels of function (a) before and (b) after transtympanic gentamicin microwick perfusion.
Glasgow benefit inventory
The Glasgow benefit inventory results (Figure 6) demonstrated an improved quality of life in patients with class A vertigo control, with a mean total score of +34. This indicated substantial benefit from the intervention. However, three patients with class B vertigo scored poorly, with a mean of −18. It should be noted that these three patients initially had class A control for periods varying from 10 to 30 months after treatment, and that during this time they may have had good quality of life.

Fig. 6 Glasgow benefit inventory (GBI) scores in patients achieving class A and class B vertigo control following transtympanic gentamicin microwick perfusion.
Change in hearing
Four patients were found to have a dead ear at the time of the study. Of these, three had pre-operative dead ears. One patient with a pre-operative PTA of 57 dB developed a dead ear post-operatively. Three further patients demonstrated a decrease in hearing, with a mean reduction of 17 dB. The incidence of hearing loss due to the procedure was therefore 26 per cent (four out of 15 patients). Two patients showed improvement in hearing, with a mean increase of 16.5 dB. In the remaining six patients, hearing remained unchanged.
Change in tinnitus
Four patients reported an improvement in their tinnitus. Patients' tinnitus was reported as unchanged in nine cases and worse in two cases.
One patient developed severe pain in the operated ear post-operatively, requiring strong analgesia. In another patient, the round window niche could not be located through the initial myringotomy and a second incision had to be made at a higher level in order to successfully complete the operation. Despite these incidents, both these patients healed well. One patient required a tympanotomy because of overhang of the posterior canal wall. There was no incidence of tympanic membrane perforation or infection.
Discussion
Gentamicin-induced vestibulotoxicity has been successfully utilised in the treatment of Ménière's disease, as reported by several studies. In a recent meta-analysis, intratympanic gentamicin therapy was found to result in 75 per cent class A vertigo control and 93 per cent class B control, without significant hearing loss.Reference Cohen-Kerem, Kisilevsky, Einarson, Kozer, Koren and Rutka8 Gentamicin can be injected into the middle ear, but the procedure needs to be repeated several times. This can result in reduced patient compliance. In addition, the amount of drug actually delivered onto the round window niche is doubtful with this technique; it is possible that much of the dose drains into the eustachian tube rather than reaching the round window.
Studies using a round window microcatheter have reported vertigo control varying from 72 to 100 per cent, with a hearing loss rate of up to 82 per cent. However, this procedure requires a tympanotomy.Reference Suryanarayanan and Cook3
The only available published study using the Silverstein MicroWick as a delivery vehicle was published by the Silverstein group itself.Reference Jackson and Silverstein9 In a review of 92 patients, these authors found 85 per cent vertigo control, along with good relief from aural pressure and tinnitus. The incidence of hearing loss in this study was 37 per cent. This study differed from ours in the treatment regimen used. In contrast to our study, Jackson and Silverstein used the titration method, and vestibular ablation was the end-point of treatment. The same group subsequently published their results for long term follow up, with a vertigo control rate of 77 per cent.Reference Hill, Digges and Silverstein10
The Silverstein MicroWick procedure has several advantages. As the affected ear is treated directly, systemic toxicity of the drug is avoided. The procedure is less invasive and easy to perform. It can be done under local anaesthesia, making it a clinic procedure. Even when performed under general anaesthesia, patients can be discharged the same day. Patients are able to self-treat over the next few weeks. The procedure is well tolerated by patients.
• Gentamicin-induced vestibulotoxicity has been successfully utilised in the treatment of Ménière's disease, as reported by several studies
• Transtympanic gentamicin therapy using the Silverstein MicroWick results in good vertigo control
• Provided patients are fully informed of the risk of hearing deterioration, this therapy can be an alternative to intracranial treatments such as vestibular neurectomy
On the negative side, the incidence of hearing loss is higher with any form of transtympanic gentamicin therapy (13–25 dB), when compared with procedures such as vestibular neurectomy (1.8–2 dB).Reference Hillman, Chen and Arriaga11, Reference Colletti, Carner and Colletti12 The latter also produces better vertigo control (95–96 per cent) when compared with intratympanic gentamicin therapy (75–80 per cent).Reference Hillman, Chen and Arriaga11, Reference Colletti, Carner and Colletti12
Despite its adverse effect on hearing, intratympanic gentamicin therapy continues to be popular, not only because of the many advantages mentioned above, but also due to the quick post-operative recovery. Vestibular neurectomy typically produces acute, unilateral labyrinthine failure, resulting in temporary imbalance. In comparison, intratympanic gentamicin therapy in general, and that using the Silverstein wick in particular (as per our study), generally produces relatively less imbalance and distress in the post-operative recovery period, when complete ablation of the vestibular response is not chosen as the end-point of therapy.
We did not perform post-operative caloric tests, because vestibular ablation was not the end-point of treatment. Neither is such testing mandatory, as indicated by the American Association of Otolaryngology-Head and Neck Surgery guidelines on reporting Ménière's disease treatment results. However, in our study, the fact that hearing remained unchanged in six patients and improved in two patients suggests that our therapy did not result in complete vestibular ablation. It is possible that the residual vestibular function in the treated ear could have contributed to smoother post-operative recovery. Complete vestibular ablation does not seem to be necessary to obtain good vertigo control using gentamicin ear perfusion. Previous studies have reported good vertigo control, without much hearing loss or any significant reduction in vestibular function.Reference Suryanarayanan and Cook3, Reference Hoffer, Kopke, Weisskopf, Gottshall, Allen and Wester13 It may be that gentamicin causes a biochemical alteration rather than an ablation when used for a short period of time.
Conclusion
Transtympanic gentamicin therapy using the Silverstein MicroWick results in good vertigo control in Ménière's disease patients. The procedure is less invasive and better tolerated. Provided that patients are made fully aware of the risk of hearing deterioration, this therapy can be an alternative to intracranial treatments such as vestibular neurectomy, which may be refused by the patient or contraindicated due to coexisting medical illness. Transtympanic gentamicin microwick perfusion would also be an ideal alternative in centres where neuro-otological expertise is unavailable.