Introduction
Epistaxis is the most common emergency in the field of ENT services, with around 25 000 hospital presentations per year in the National Health Service (NHS).1 Epistaxis management consumes significant NHS resources, as evident in the Health and Social Care Information Centre figures for England and Wales from 2014 to 2015, which demonstrated 7935 consultant-managed ‘surgical arrest of bleeding from the internal nose’ episodes and 9113 ‘packing of cavity of nose’ actions, with an average in-patient stay of 3 days per epistaxis episode.Reference Ellinas, Jervis, Kenyon and Flood2
Persistent epistaxis that does not resolve following first-line measures such as nasal cautery or packing may require surgical intervention. Endoscopic sphenopalatine artery ligation has gained popularity as the surgical intervention of choice for persistent epistaxisReference Abdelkader, Leong and White3 since its first description by Malcomson in 1963.Reference Malcomson4 Published evidence has demonstrated its benefits in terms of efficacyReference Nouraei, Maani, Hajioff, Saleh and Mackay5,Reference Kitamura, Takenaka, Takeda, Oya, Ashida and Shimizu6 and cost-savings.Reference Dedhia, Desai, Smith, Lee, Schaitkin and Snyderman7,Reference McDermott, O'Cathain, Carey, O'Sullivan and Sheahan8
Despite this, there has been no conclusive evidence in the literature regarding the potential complications and long-term outcomes associated with sphenopalatine artery ligation.Reference Ellinas, Jervis, Kenyon and Flood2 Re-bleeding that requires further revision surgery is a possible complication. This was demonstrated in a meta-analysis by Kitamura et al.,Reference Kitamura, Takenaka, Takeda, Oya, Ashida and Shimizu6 comprising 33 studies with 896 sphenopalatine artery ligation cases, which showed a pooled total re-bleeding rate of 13.4 per cent (95 per cent confidence interval (CI), 10.0 per cent–17.8 per cent). However, a case series by George et al. demonstrated that 89.4 per cent of patients who underwent sphenopalatine artery ligation had not experienced re-bleeding by the five-year review.Reference George, Smatanova, Joshi, Jervis and Oluwole9 Vessel ligation carries a theoretical risk of ischaemic necrosis and subsequent septal perforation, although this is only sparsely reported in the literature.Reference Elsheikh and El-Anwar10
This study aimed to evaluate the peri-operative outcomes of all patients who underwent sphenopalatine artery ligation at two secondary care centres over a 10-year period, with a focus on re-bleeding rates and septal perforation.
Materials and methods
A retrospective review was performed for all patients who underwent sphenopalatine artery ligation for treatment of epistaxis between January 2011 and January 2021 at Frimley Park Hospital and Wexham Park Hospital. A search was performed by the Department of Health Informatics in both centres using the operating procedure code E05.2 (ligation of artery of the internal nose). Those patients who underwent sphenopalatine artery ligation for reasons other than epistaxis, with incorrectly coded procedures or with incomplete medical notes were excluded.
The following data were extracted from patient records: baseline characteristics, and pre-, peri- and post-operative data. The pre-operative data include interventions prior to surgery, such as cautery or packing. The peri-operative data include concurrent procedures such as septoplasty and nasal cautery. The post-operative data include re-bleeding rates, septal perforation and follow-up time.
Microsoft Excel® spreadsheet software was used to perform data organisation and descriptive statistical analysis.
Results
Baseline characteristics
During the 10-year study period, 131 patients were identified in a search conducted by the Department of Health Informatics using the operating procedure code E05.2 (ligation of artery of the internal nose). Twenty-nine patients were excluded as they did not undergo sphenopalatine artery ligation for treatment of persistent epistaxis. Eleven patients were excluded because of incomplete medical records.
Ninety-one patients were included in the final analysis. Results from the search process are presented in Figure 1.
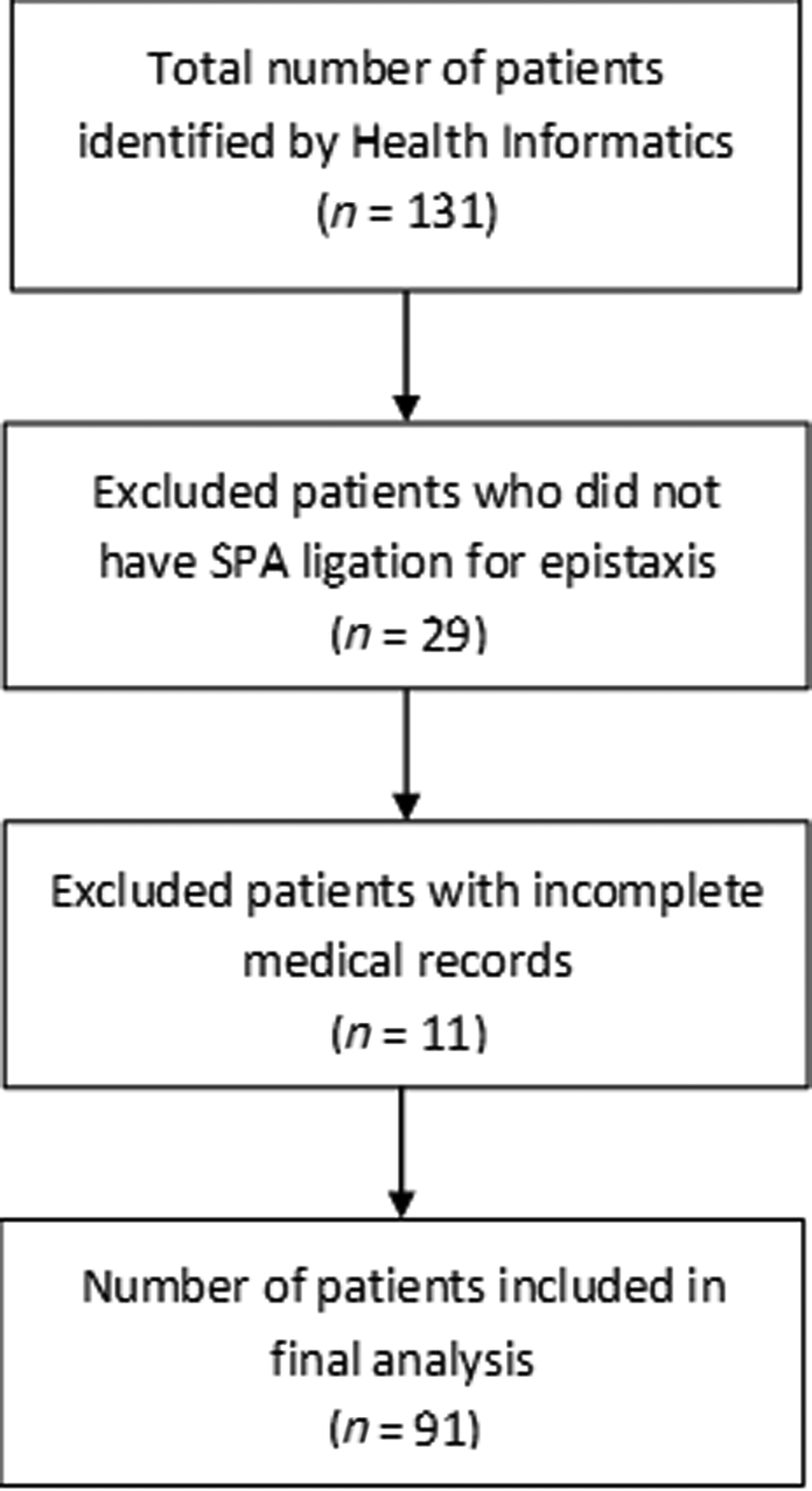
Fig. 1. Department of Health Informatics search for sphenopalatine artery (SPA) ligation patients.
The median age of the study population was 63 years (range, 13–90 years). There were 60 men and 31 women. The median number of previous hospital attendances for epistaxis was 2 (range, 0–10 attendances). Hypertension was the most common co-morbidity in the study population (61.5 per cent). Further information on baseline characteristics are presented in Table 1.
Pre-operative data
Most of the study population underwent sphenopalatine artery ligation as an emergency operation for the control of persistent epistaxis (78.0 per cent). The median time to surgery from admission was 1 day (range, 0–28 days). Pre-operative non-dissolvable nasal packing was used a median of 1 time (range, 0–8 times). Table 2 provides additional information on pre-operative data.
Peri-operative data
Twelve patients (13.2 per cent) underwent concurrent septoplasty surgery to facilitate access. Thirty-five patients (38.5 per cent) had concomitant bipolar cautery to the nasal septum for additional haemostasis (Table 3).
Post-operative data
Table 4 illustrates the post-operative outcomes for the study population. The median time to discharge from surgery was 1 day (range, 0–56 days). Sphenopalatine artery ligation surgery was successful in controlling bleeding for the majority of the study population (79.1 per cent), with 19 patients (20.9 per cent) reporting re-bleeding in the post-operative period. Fourteen of these patients (15.4 per cent) were managed conservatively. Five patients (5.5 per cent) required further revision surgery to control the bleeding. Four patients (4.4 per cent) were found to have septal perforation at the post-operative review. The median follow-up time was 54 days (range, 0–2657 days).
Table 5 compares peri-operative factors between the four patients diagnosed with septal perforation and the total sphenopalatine artery ligation cohort. We noted a higher percentage of certain risk factors in these four patients compared to the total cohort, such as hypertension (100 per cent), antiplatelet or anticoagulant therapy (50 per cent), previous silver nitrate cautery (100 per cent), previous sphenopalatine artery ligation (50 per cent), higher median number of uses of non-dissolvable nasal packing (n = 3), concurrent bipolar cautery to the nasal septum (100 per cent), and concurrent septoplasty (75 per cent).
Table 5. Details of septal perforation cases

*n = 4; †n = 91. KTP = potassium titanyl phosphate; SPA = sphenopalatine artery
Table 6 explores the operative records and risk factors in those five patients who required revision surgery. All had one or more risk factors, including pre-existing hypertension, antiplatelet therapy and previous sphenopalatine artery ligation surgery. Four out of five patients (80 per cent) required control of further arterial bleeding sources besides the main sphenopalatine artery branch.
Table 6. Details of revision surgery for re-bleeding
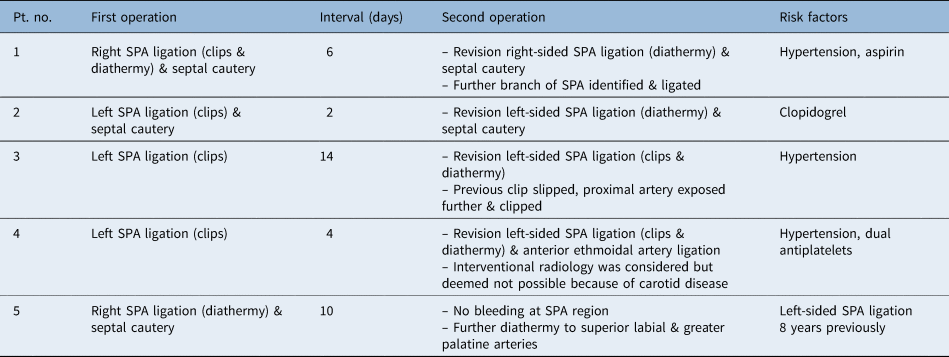
Pt. no. = patient number; SPA = sphenopalatine artery
Discussion
In recent years, sphenopalatine artery ligation has continued to gain popularity as a definitive surgical treatment for persistent epistaxis, in line with the increasing popularity of endoscopic sinus surgical procedures.Reference Abdelkader, Leong and White3 This trend is also reflected in our 10-year series, where there has been an overall increase in the number of sphenopalatine artery ligation surgical procedures performed each year from 2011 to 2021, as shown by Figure 2. Possible reasons behind this observed trend include better awareness and training of ENT surgeons to escalate persistent epistaxis patients to surgery,Reference Walen, Rudmik, Lipkewitch, Dixon and Mechor11 as well as increases in medical co-morbidities and anticoagulation therapy within the patient population.

Fig. 2. Number of sphenopalatine artery (SPA) ligations performed by year.
However, despite the well-established role of sphenopalatine artery ligation for treating persistent epistaxis, there is still a lack of consensus and no national guidelines regarding: patient selection, timing for escalation to ligation surgery and recommended surgical techniques for vessel ligation. This has resulted in considerable variation in national practice.Reference Ellinas, Jervis, Kenyon and Flood2,Reference Daudia, Jaiswal and Jones12 Previous studies in the literature have recommended certain criteria and algorithms for sphenopalatine artery ligation, such as the Wexham Park Criteria or the Dundee Protocol.Reference Lakhani, Syed, Qureishi and Bleach13,Reference Spielmann, Barnes and White14 Further research in this area is needed to identify consensus surgical criteria for widespread national adoption, in order to better inform patient selection and timing for surgery, and to predict the likelihood of successful haemostasis and complications.
In this 10-year data series, sphenopalatine artery ligation successfully controlled bleeding and prevented epistaxis recurrence in 72 out of 91 patients (79.1 per cent) who underwent surgery. Of the 19 patients (20.9 per cent) who reported post-operative re-bleeding, only 5 (5.5 per cent) required further revision surgery. These figures are similar to findings from previous studies, suggesting that sphenopalatine artery ligation is an effective treatment modality for persistent epistaxis.Reference Abdelkader, Leong and White3,Reference Nouraei, Maani, Hajioff, Saleh and Mackay5,Reference Kitamura, Takenaka, Takeda, Oya, Ashida and Shimizu6,Reference McDermott, O'Cathain, Carey, O'Sullivan and Sheahan8,Reference Howe, Wazir and Skinner15–Reference Basnet, Ghimire, Shrestha and Aryal17
Factors that were independently associated with most of the five patients who required revision surgery (Table 6) included hypertension, antiplatelet therapy, previous sphenopalatine artery ligation, using clips only instead of diathermy during the first surgery, and alternative bleeding sources besides the sphenopalatine artery. Despite the lack of evidence for direct causality, these risk factors are consistent with those identified in previous studies,Reference Howe, Wazir and Skinner15 and may be interpreted as predictors of procedural failure. We postulate that the use of surgical clips only may be detrimental and they can be accidentally displaced when the surgeon continues dissection by searching for further vessels posteriorly.Reference McDermott, O'Cathain, Carey, O'Sullivan and Sheahan8 This is supported by Kitamura and colleagues’ meta-analysis,Reference Kitamura, Takenaka, Takeda, Oya, Ashida and Shimizu6 which demonstrated a significantly higher re-bleeding rate in patients who underwent sphenopalatine artery ligation with clips only (15.1 per cent; 95 per cent CI, 9.8–22.5) compared to with diathermy only (7.2 per cent; 95 per cent CI, 4.6–11). In one of our study centres, the use of clips was discouraged amongst junior surgeons because of the higher risk of re-bleeding.
Sphenopalatine artery ligation carries a risk of ischaemic necrosis and subsequent septal perforation,Reference Ellinas, Jervis, Kenyon and Flood2 although this is only rarely reported in the literature,Reference Elsheikh and El-Anwar10 which may be due to the rich vascular supply present in the nasal mucosa.Reference Ellinas, Jervis, Kenyon and Flood2 The risk is deemed to be higher if there is further compromise to collateral blood supply of the nasal lining, such as bilateral sphenopalatine artery ligations.Reference Elsheikh and El-Anwar10 We do not advocate bilateral sphenopalatine artery ligations concurrently, unless there is severe, intractable bleeding in an emergency scenario. We would instead recommend surgery on the more symptomatic side (where identifiable), with a return to the operating theatre (semi-electively, after a suitable interval), to perform an endoscopic ligation on the contralateral side, if the bleeding does not settle. This may allow, in theory, collateral vessels to form, and minimises the risks of crusting, dryness and ischaemia that lead to necrosis followed by subsequent septal perforation.
Risk factors that were found to be more common in our septal perforation cohort compared to the total cohort (Table 5) may also compromise collateral blood supply of the nasal lining. There is evidence that smoking and septoplasty are associated with a higher risk of septal perforation.Reference Cetiner, Cavusoglu and Duzer18 Higher pressures of nasal packing may also induce ischaemic necrosis,Reference Elwany, Kamel and Mekhamer19,Reference Moorthy, Anand, Prior and Scott20 although this factor was not measured in this study. Other potential identifiable risk factors might include hypertension, previous procedures and concurrent septal cautery; however, there are no direct significant associations between these factors and ischaemic necrosis of nasal mucosa in current literature.Reference Nouraei, Maani, Hajioff, Saleh and Mackay5
In a total cohort of 91 patients, there were peri-operative complications of re-bleeding (20.9 per cent), requirements for further revision surgery (5.5 per cent) and occurrences of septal perforation (4.4 per cent). Despite the presence of confounding risk factors such as hypertension, anticoagulation therapy, non-dissolvable nasal packing use, concurrent septal cautery or septoplasty, we felt that these potential complications should be included in the consenting process for sphenopalatine artery ligation surgery and thoroughly explained to patients. Future research should focus on delineating the exact roles of these risk factors in precipitating re-bleeding and septal perforation as compared to the surgical practice of sphenopalatine artery ligation itself.
• Endoscopic sphenopalatine artery ligation has gained popularity as a surgical intervention for persistent epistaxis; it has efficacy and cost-saving benefits
• Evidence on potential complications and long-term outcomes associated with sphenopalatine artery ligation is limited
• Vessel ligation carries a theoretical risk of ischaemic necrosis and subsequent septal perforation, but this is sparsely reported in literature
• Sphenopalatine artery ligation was effective in controlling persistent epistaxis for most patients (79.1 per cent)
• In this study, 5.5 per cent of patients had re-bleeding needing revision surgery, and 4.4 per cent had septal perforation
• These complications may be precipitated by confounding risk factors (pre-operative non-dissolvable nasal packing, concurrent septal cautery, septoplasty and co-morbidities)
We identified several limitations to our study. The study is retrospective by design, which increases the risk of biases. The search process performed by Health Informatics (Figure 1) may be limited by inaccurate coding of operating procedures, which may mean a lower number of patients should have been included, with a subsequent reduction in the power of the study. The rarity of the complication of septal perforation means that there is likely to be an increased risk of type II errors with our findings. Our median follow-up duration of 54 days may be an insufficient period to adequately evaluate post-operative complications.
Conclusion
Our study found that sphenopalatine artery ligation was effective in controlling persistent epistaxis for most of our patient cohort, with small numbers of re-bleeding episodes requiring revision surgery and septal perforations. Further research on the peri-operative complications of sphenopalatine artery ligation is needed. Pre-operative non-dissolvable nasal packing, concurrent septal cautery, septoplasty, and co-morbidities such as hypertension represent potential confounding factors which could not be further assessed in this small, retrospective study.
Competing interests
None declared














