Introduction
The Eustachian tube plays an important role in the pressure equalisation, drainage and overall health of the middle ear. Anatomically, it connects the mesotympanum and nasopharynx, and consists of a lateral bony and medial cartilaginous segment. In contrast to the bony segment, the cartilaginous segment is dynamic, opening and closing. Whilst at rest, the Eustachian tube orifice, which is made by the cartilaginous portion, remains closed. The Eustachian tube classically opens during swallowing and yawning because of tensor veli palatini and levator veli palatini actions. Eustachian tube dysfunction can result from failure of the tube to open or close appropriately. This article describes the patulous Eustachian tube, which is characterised by chronic patency and failure to close.
Patulous Eustachian tube affects 0.3–6 per cent of the population. This clinical diagnosis is based on history and examination with nasoendoscopy.Reference DiBartolomeo and Henry1 Patients typically present with symptoms of autophony, aural fullness and increased perception of physiological sounds, such as the heart beat and breathing.Reference O'Connor and Shea2 Examination demonstrates movement of the tympanic membrane with respiration, and dilation of the Eustachian tube orifice.Reference Yoshida, Kobayashi, Takasaki, Takahashi, Ishimaru and Morikawan3 There are a number of theories behind the causality of patulous Eustachian tube, including tissue loss (weight loss, pregnancy, use of oestrogen therapy), and atrophy or scarring of the nasopharynx secondary to adenoidectomy, radiotherapy, poliomyelitis and trauma.Reference O'Connor and Shea2, Reference Plate, Johnsen, Nodskov Pedersen and Thomsen4, Reference Pulec5
Treatment can be divided into medical or surgical modalities, although the effectiveness is limited. We present our first case of patulous Eustachian tube treated with transnasal endoscopic obliteration of the Eustachian tube with endovascular coils. To the best of our knowledge, this novel technique has not been described in literature previously.
Materials and methods
To date, we have successfully treated one patient with the following procedure. The patient consented to undergo Eustachian tube obliteration using a 3 mm VortX Diamond coil (Boston Scientific, Marlborough, Massachusetts, USA); the risks of bleeding, infection, pain, conductive hearing loss due to glue ear, treatment failure and coil migration were relayed. The procedure was undertaken alongside a neuroradiologist.
The procedure can be performed under local or general anaesthetic, depending on the degree of nasal septal deviation affecting instrumentation of the Eustachian tube orifice. The patient is suitably positioned and decongested as for functional endoscopic sinus surgery. Under direct endoscopic visualisation using a 4 mm, 0-degree rigid endoscope, the Eustachian tube orifice is identified. Once the Eustachian tube is confirmed patent, a 70-degree Relieva sinus guide suction tube from a balloon sinuplasty set (Acclarent, Irvine, California, USA) is passed into the post-nasal space and guided into the Eustachian tube orifice. A 3.0 × 3.3 mm VortX Diamond coil (fibred platinum coil) is subsequently passed through a standard embolisation catheter and inserted to a depth of 1.5 cm, to the opening of the Eustachian tube.
A cone beam computed tomography (CT) scan was undertaken post-operatively to confirm adequate positioning. The patient was then followed up at one and six months to assess outcome and symptom resolution.
Case report
A 27-year-old female presented with intrusive symptoms of bilateral autophony secondary to patulous Eustachian tubes. She consented to undergo left Eustachian tube obliteration with an endovascular coil (Figure 1). The procedure was successfully undertaken, with a six-week post-operative cone beam CT scan confirming adequate positioning (Figure 2).
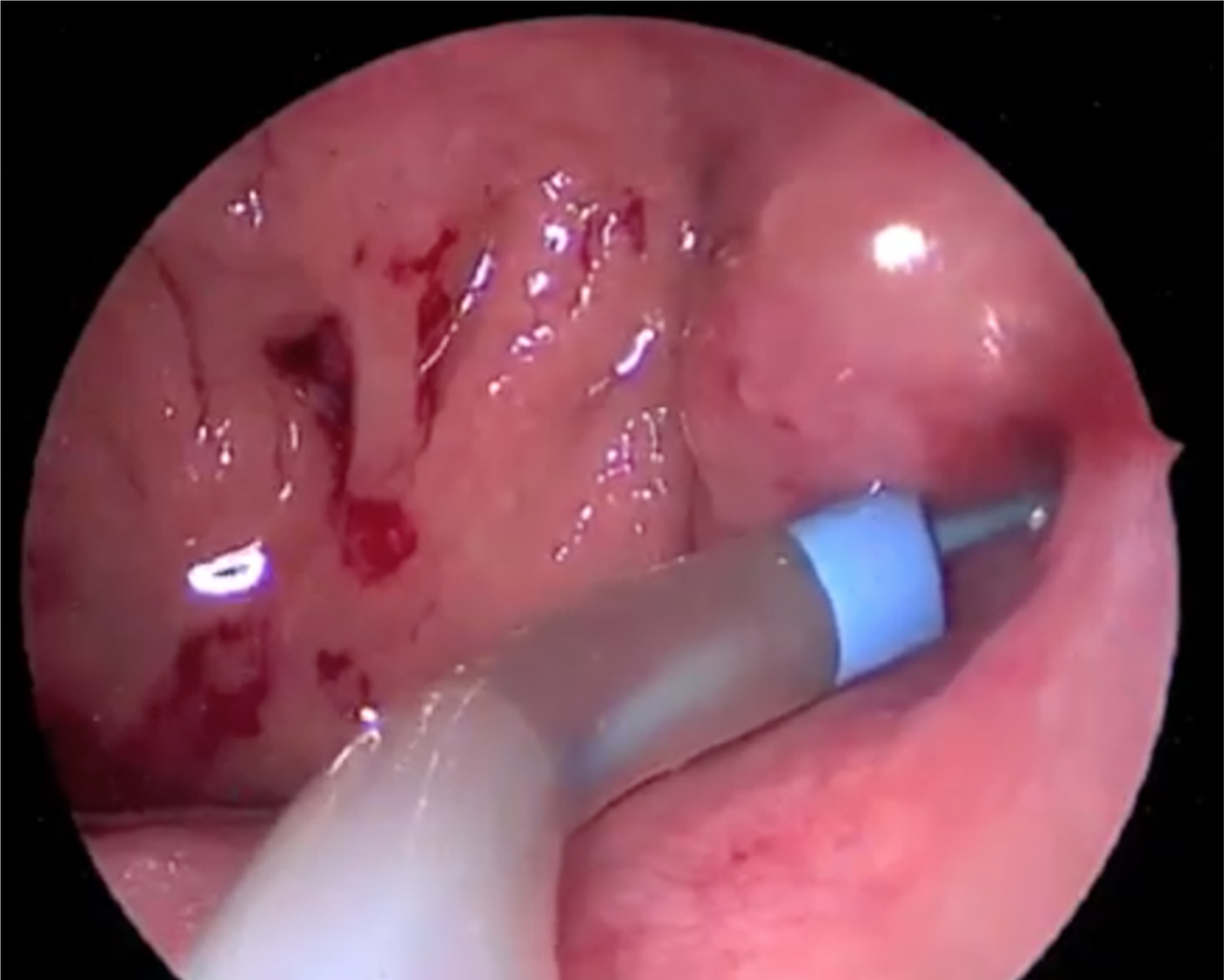
Fig. 1 Endoscopic view of the Boston Scientific VortX Diamond coil being inserted in the left Eustachian tube.
Fig. 2 Axial computed tomography image showing the Boston Scientific VortX Diamond coil in the left Eustachian tube.
Her symptoms subsided significantly, and a second procedure on the contralateral ear was requested. Although a second post-operative follow up confirmed adequate positioning bilaterally, with resolution of autophony, the patient developed right-sided tinnitus and mild conductive hearing loss secondary to middle-ear effusion. The effusion was drained through a myringotomy, with no further symptomology documented on a recent follow up.
Discussion
Patulous Eustachian tube dysfunction is a debilitating yet relatively uncommon condition. A wide range of both medical and surgical techniques have been described to treat the condition, with no consistency in effectiveness amongst them. The diagnosis of patulous Eustachian tube is clinical, and based on a cluster of symptoms and direct visualisation. The severity and frequency of symptoms can be variable, and will direct clinicians as to the management plan.
Most patients' symptoms can be effectively managed with conservative measures. Currently, the most commonly used topical therapy is intranasal saline, which has demonstrated resolution of symptoms in 45.2–65.7 per cent of patients.Reference Ikeda, Oshima, Oshima, Miyazaki, Kikuchi and Kawase6, Reference Oshima, Kikuchi, Kawase and Kobayashi7 Historically, other topical therapies adopted include hydrochloric acid, boric acid and benzyl alcohol, with marginal benefit.Reference Luu, Remillard, Fandino, Saxby and Westerberg8 Although a large proportion of patients' symptoms settle following topical saline use, patients with severe symptoms or symptoms refractory to conservative measures may be considered for surgery.
Surgical management can be divided into categories depending on the mode of function. These include mass loading of the tympanic membrane, Eustachian tube plugging, Eustachian tube injections, cautery or ligation of the Eustachian tube orifice, or a combination of the aforementioned. Mass loading of the tympanic membrane aims to weigh the membrane down to reduce excessive mobility, which is reported to be the cause of symptoms. This is most commonly achieved by ventilation tubes, with partial or full resolution of symptoms in 53–100 per cent of patients.Reference Ikeda, Oshima, Oshima, Miyazaki, Kikuchi and Kawase6, Reference Thaler and Yanagisawa9, Reference Chen and Luxford10 Other mass loading techniques include blue tacking or paper patching, with partial or complete resolution of symptoms in 78.6 per cent and 76.2 per cent of patients for each method respectively.Reference Bartlett, Pennings, Ho, Kirkpatrick, Van Wijhe and Bance11, Reference Boedts12 Given the relative rarity of the condition, the numbers in the aforementioned series are limited at 14 and 16 respectively.Reference Bartlett, Pennings, Ho, Kirkpatrick, Van Wijhe and Bance11, Reference Boedts12
Regarding Eustachian tube plugging, techniques have involved fat grafting, silicone plugs, tissue glue, bone wax, angiocatheters or a combination, alongside cautery. The majority of these methods were transtympanic; success rates were marginal, with limited patients within the case series. The most well-established plugging technique utilises the Kobayashi silicone plug. A recent study of 252 ears treated with the Kobayashi plug showed successful treatment in 83.0 per cent of patients, with complications of tympanic membrane perforation and middle-ear effusions falling to 17.5 per cent and 10.2 per cent respectively with the new plugs.Reference Kikuchi, Ikeda, Oshima, Takata, Kawasw and Oshima13 Cautery alone to the Eustachian tube yielded symptom resolution across two studies in 66.6–83.3 per cent of patients.Reference Robinson and Hazell14, Reference Yanez, Pirron and Mora15
• Patients with patulous Eustachian tube commonly present with symptoms of aural fullness and autophony
• There are a variety of different surgical options, each with limited evidence behind their use
• A new endonasal technique is proposed, which involves plugging the Eustachian tube
• This is a day-case procedure, in which an endovascular coil is deployed into the distal Eustachian tube
• Risks include bleeding, infection, displacement, pain and glue ear
Our technique has so far proved to be highly effective and minimally invasive. There is no optimal treatment consensus for patulous Eustachian tube given the low level of evidence in the literature. Topical saline instillation and ventilation tube placement appear to be the most effective and commonly utilised modalities amongst practitioners, with a good safety profile. We aim to use this technique with more patients, in order to fully establish its effectiveness in the treatment of patulous Eustachian tube.
Competing interests
None declared




