Introduction
Chronic rhinosinusitis is a common disorder that may be associated with a significant impact on quality of life (QoL) for affected individuals and adds a well-known burden on the healthcare system.Reference Soy, Pinar, Imre, Calli, Calli and Oncel1 The maxillary sinus is frequently affected by inflammatory processes because of its dependent position which, presumably, makes gravity a natural hindrance against proper mucociliary clearance. This makes maxillary sinuses a common target for endoscopic sinus surgery performed to treat chronic rhinosinusitis.Reference Richtsmeier2,Reference Morrissey, Wormald and Psaltis3
According to the nature and extent of the pathology within the maxillary sinus, the surgical approach is planned to optimise visibility and control of the affected part of the sinus and thereby enhance surgical success.
With improvement of surgical techniques, together with the advancement of angled telescopes and instruments, functional middle meatal antrostomy became the preferred endoscopic transnasal ‘window’ not only to secure ventilation through widening of the natural ostium but also to access and manage pathologies within the maxillary sinus.Reference Morrissey, Wormald and Psaltis3,Reference Woodworth, Parker and Schlosser4
The second window to access the maxillary sinus endoscopically is the inferior meatal antrostomy. This was considered the main approach to the maxillary sinus in the pre-endoscope era; however, it is much less in use nowadays and has been almost completely replaced by middle meatal antrostomy.Reference Eloy, Marchiano and Vazquez5
A well-pneumatised maxillary sinus can have peripheral extensions into the surrounding bony framework. Further pneumatisation anteriorly, anterolaterally, inferiorly or inferomedially is associated with anatomical recesses, namely prelacrimal, zygomatic, alveolar or palatal recesses, respectively. Pathologies in these ‘around the corner’ areas may be difficult to effectively visualise and handle endoscopically through a large middle meatal antrostomy or even through endoscopic medial maxillectomy.
The prelacrimal recess approach was first described by Zhou et al.Reference Zhou, Han, Cui, Huang, Wei and Liu6 as a minimally invasive approach to certain maxillary sinus lesions with complete preservation of the lacrimal duct and the inferior turbinate. In this report, we describe our experience in utilising the prelacrimal recess approach as a ‘third window’ for accessing the maxillary sinus through a transnasal endoscopic approach.
The aim of our study was to assess the outcomes of combined middle meatal antrostomy and a prelacrimal recess approach in the management of maxillary sinus pathologies in ‘difficult to reach areas’ within the sinus. The prelacrimal recess approach was used as an alternative to the Caldwell–Luc approach or canine fossa puncture,Reference el-Guindy and Mansour7 with their significant post-operative morbidity.Reference Lock, Siow, Karandikar, Goh and Siow8,Reference DeFreitas and Lucente9
Materials and methods
This was a prospective cohort study that was conducted in a tertiary referral hospital, at the Department of Otolaryngology – Head and Neck Surgery, Tanta University Hospital, Egypt, between April 2017 and March 2019.
Patients enrolled in the study had pathologies in difficult to reach areas within the maxillary sinus (e.g. isolated fungal balls, antrochoanal polyps or displaced dental structures) provided that the width of the prelacrimal recess was more than 3 mm as shown in Figure 1. The prelacrimal recess width was obtained by measuring the distance between the anterior wall of the maxillary sinus and the anterior border of the nasolacrimal duct, at the level of the anterior end of the attachment of the inferior turbinate into the frontal process of the maxilla. Simmen et al.Reference Simmen, Veerasigamani, Briner, Jones and Schuknecht10 proposed that a prelacrimal recess width more than 7 mm allows the prelacrimal recess approach to be performed easily, a width between 3–7 mm requires displacement of the nasolacrimal duct and a width of 0–3 mm makes this approach less feasible.

Fig. 1. Axial plane computed tomography scan of the nasolacrimal duct (white arrow) and the lacrimal recess of the maxillary sinus (black arrow).
Patients were excluded if they had a prelacrimal recess width less than 3 mm, benign and malignant tumours of the maxillary sinus or maxillary sinus pathology that was accessible by middle meatal antrostomy.
Computed tomography (CT) scans of the nose and the paranasal sinuses were done with 1 mm cuts. Coronal, axial and sagittal views were reconstructed to assess the extent of the pathology and pneumatisation of the maxillary sinus, the course of the nasolacrimal duct in the lateral nasal wall, and the presence and width of the prelacrimal recess.
Ethical consideration
The study was approved by the Tanta University institutional review board and informed consent was obtained from all patients. Patient data were collected from electronic case records and questionnaires and reviewed only by members of the responsible research team.
Operative technique
All patients were operated on under general anaesthesia. The procedure was started by using traditional middle meatal antrostomy. In cases where the pathology within the maxillary sinus was not completely accessible through the middle meatal antrostomy, a prelacrimal recess approach was undertaken (Figure 2a–f).
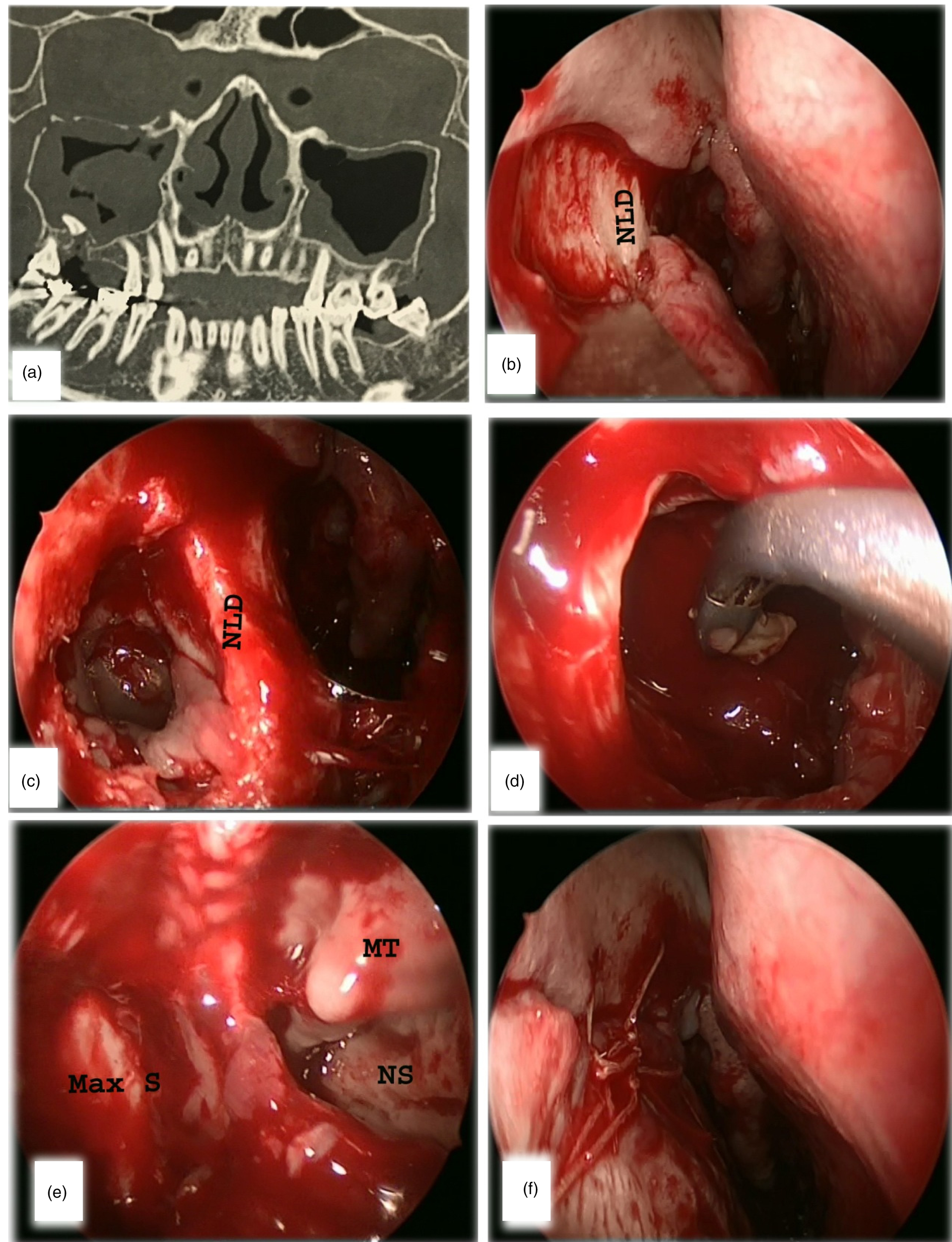
Fig. 2. (a) Cone beam computed tomography scan (coronal view) showing migrated part of the tooth with inflammatory reaction around it. (b) Incision of the lateral nasal wall begins at the anterior end of the middle meatal antrostomy just above the inferior turbinate. (c) An access window created in the lateral nasal wall anterior to the nasolacrimal duct (NLD). (d) Extraction of a part of tooth through the prelacrimal recess. (e) Endoscopic view from within the maxillary sinus (Max S) demonstrating middle turbinate (MT) and nasal septum (NS) through the middle meatal antrostomy. (f) Closure of mucoperiosteal flap at the end of the operation.
We injected 1 per cent lidocaine with 1:100 000 epinephrine in the submucosal plane of the lateral nasal wall, superior and anterior to the anterior attachment of the inferior turbinate. A horizontal mucosal incision was made on the lateral nasal wall from the anterior edge of the antrostomy, a few millimetres above the anterior insertion of the inferior turbinate, to the edge of the pyriform aperture. Dissection and mobilisation of the mucoperiosteal flaps was done slowly using a freer instrument to keep them intact and achieve exposure of the bony lateral nasal wall. An access window through the lateral nasal wall, anterior to the nasolacrimal duct, was opened using a drill or an osteotome. Widening of the window was done as much as needed to allow proper access into the maxillary sinus using Kerrison forceps or a drill with careful preservation of the nasolacrimal duct. This window usually allowed exploration of the whole maxillary sinus including the anterior wall and alveolar and palatine recesses of the maxillary sinus with proper eradication of the pathology. In cases of a narrow prelacrimal recess, we tended to remove the lacrimal bone and the nasolacrimal duct was bluntly freed out of its bony canal and medialised. The ascending process of the maxilla forming the bony canal of the lacrimal duct can be removed without causing epiphora as the function of the valve of Hasner is not dependent on bony support.Reference Lock, Siow, Karandikar, Goh and Siow8
Depending on the size of the prelacrimal recess and the window made, the window allowed access of both the endoscope and an instrument to manipulate the pathology as demonstrated in Figure 2d, or it allowed access of the endoscope alone while a curved instrument was passed through the middle meatal antrostomy to clear the pathology (two ports technique) as shown in Figure 3.
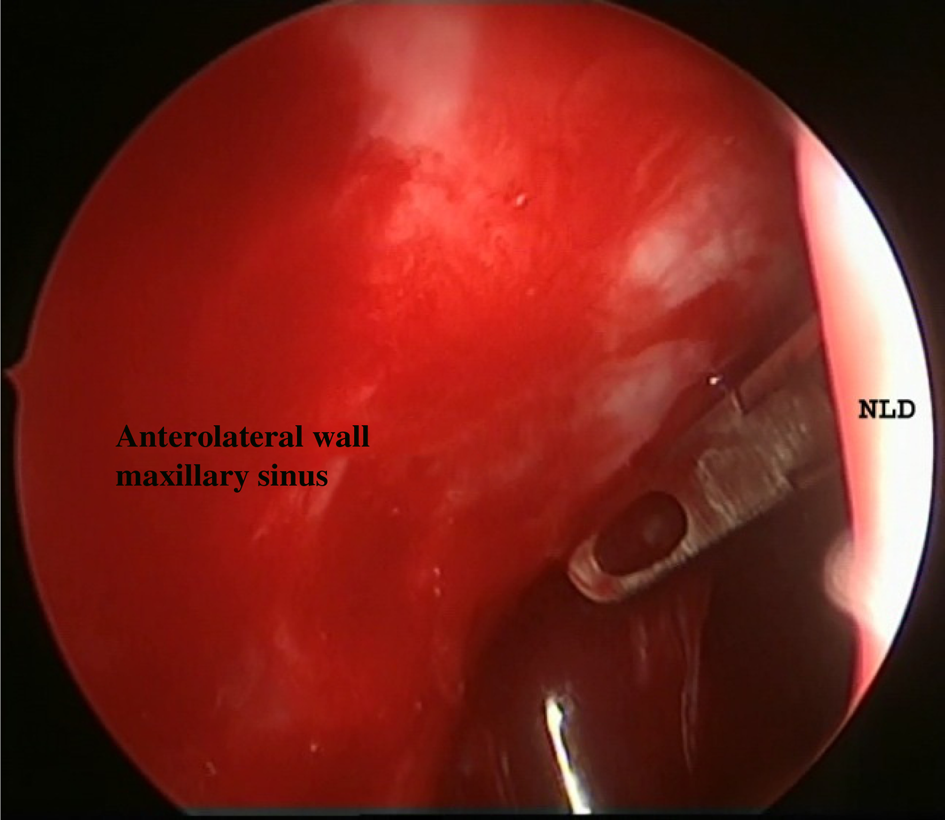
Fig. 3. Endoscopic view demonstrating working through two ports, with the endoscope passed through the prelacrimal recess and Heuwieser antrum grasping forceps passed through the middle meatal antrostomy. NLD = nasolacrimal duct
At the conclusion of the procedure the mucosal flaps were re-draped and approximated by one or two absorbable sutures, without nasal packing.
All patients received antibiotics for at least two weeks post-operatively, after which antibiotic use was individualised. All patients were encouraged to start saline douching of the nose on the first post-operative day. Post-operative endoscopic surveillance and debridement were performed in the out-patient clinic one week post-operatively and then according to endoscopic findings, in order to remove mucus, blood and crust, and to lyse synechiae.
All patients were prospectively evaluated using the validated Arabic version of the Sino-Nasal Outcome Test-22 (SNOT-22)Reference Elwany, Ibrahim, Ismail, Hussein, Youssef and Elwany11 pre-operatively and at least six months post-operatively. The SNOT-22 can be divided into four subscales: rhinological symptoms, ear and facial symptoms, sleep function and psychological manifestations subscales. Two questions (about a cough and waking up tired) are not classified into any of these subscales. The total SNOT-22 score ranges between 0 and 110, with higher total and subscale scores implying a higher impact of the disease.Reference Hopkins, Gillett, Slack, Lund and Browne12
Statistical analysis
Statistical analyses were performed using SPSS® (version 20) statistical software. Qualitative data were described using number and percentage. A Kolmogorov–Smirnov test was used to verify the normality of data distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5 per cent level. The Wilcoxon signed rank test was used for abnormally distributed quantitative variables, to compare the pre- and post-operative values.
Results
A total of 25 patients with unilateral maxillary sinus pathology underwent endoscopic middle meatal antrostomy combined with the prelacrimal recess approach over the 24-month study period. Of these, there were 10 male patients and 15 female patients. The age range was 17 to 65 years (mean 37.0 ± 12.03 years). The patients were followed up for 6 to 14 months (mean 10.9 months).
Thirteen patients (52 per cent) had antrochoanal polyps, 10 patients (40 per cent) had an isolated maxillary fungal ball and two patients (8 per cent) had a part of maxillary premolar tooth displaced into the maxillary sinus. Of the 25 patients, 6 (24 per cent) had undergone previous unsatisfactory surgery (4 patients with antrochoanal polyp and 2 patients with a maxillary fungal ball) and 19 patients (76 per cent) were primary surgical patients.
We did not need to remove the lacrimal bone in 13 out of 25 cases (52 per cent). We had to remove the lacrimal bone and medially displace the nasolacrimal duct in 12 out of 25 cases (48 per cent) to allow maximal exposure of the maxillary sinus pathology.
All patients experienced significant improvement in the quality of life after the surgery with a lowering of the total mean SNOT-22 score from 57.80 ± 18.84 pre-operatively to 17.36 ± 6.99 post-operatively. Patients also showed improvement in the mean score of rhinological manifestations, ear and facial symptoms, sleep function, psychological manifestations, cough, and waking up tired subscale scores of SNOT-22 as shown in Table 1.
Table 1. Sino-Nasal Outcome Test (SNOT-22) scores
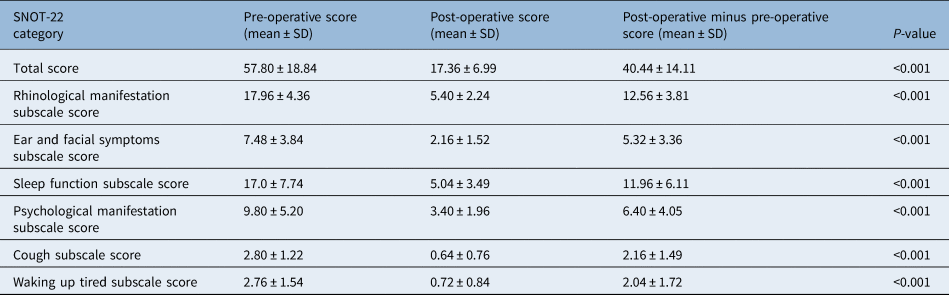
The antrostomies remained patent in all cases with pre-operative diagnosis of isolated maxillary fungal ball. The disease recurred in one patient with antrochoanal polyp despite a patent antrostomy, and this case was successfully managed with an office endoscopic procedure through a patent antrostomy.
In two cases, synechiae were noticed between the nasal septum and the lateral nasal wall, but both patients were asymptomatic, and no injury of the nasolacrimal duct was reported.
Discussion
Despite advances in equipment and instrumentation for endoscopic sinus surgery, there are still regions within the maxillary sinus that remain difficult to access in order to manage benign and malignant diseases affecting the sinus.Reference Morrissey, Wormald and Psaltis3 Middle meatal mega-antrostomy provides good access to the posterior and superior aspects of the maxillary sinus but not to the anterior wall or the floor of the maxillary sinus, especially if it is well pneumatised.Reference Robey, O'Brien and Leopold13
The prelacrimal recess approach is a promising technique that allows good exploration and surgical access to the anterior wall and floor of the maxillary sinus with lower morbidity and recurrence rates compared to the open approaches.Reference Yu, Guan, Zhang, Zhang, Jiang and Lian14,Reference Lee, Ahmad, Kim, Ryu, Kim and Dhong15 Zhou et al.Reference Zhou, Han, Cui, Huang, Wei and Liu6,Reference Zhou, Han, Cui, Huang and Wang16 first described the prelacrimal recess approach (in Chinese and English literature in 2007 and 2013, respectively) proposing removal of the bony medial maxillary wall including the bony lacrimal canal while at the same time preserving the lacrimal apparatus and the inferior turbinate. In 2015, Morrissey et al.Reference Morrissey, Wormald and Psaltis3 emphasised the importance of uncinectomy and middle meatal antrostomy with removal of bone from the margin of the pyriform aperture to improve the surveillance of the maxillary sinus via the use of angled endoscopes.
The prelacrimal recess is considered as a surgical corridor to lesions within the maxillary sinus as well as lesions of the nearby regions. A study by Li et al.Reference Li, London, Prevedello and Carrau17 included dissection of five cadaveric heads and demonstrated the role of the prelacrimal recess as direct access from the posterolateral maxillary sinus to the lateral recess of the sphenoid sinus, utilising the infra-orbital nerve as a landmark to preserve the vidian nerve and pterygopalatine ganglion. In another cadaveric study by Li et al.,Reference Li, London, Silva, Prevedello and Carrau18 the prelacrimal recess was used to access the inferior intraconal space through the orbital floor.
In a study of 100 patients, Simmen et al.Reference Simmen, Veerasigamani, Briner, Jones and Schuknecht10 previously reported that the prelacrimal recess approach was feasible in only 68.5 per cent of their patients. This percentage appeared to be higher (93 per cent) in Chinese subjects in a study published by Lock et al.Reference Lock, Siow, Karandikar, Goh and Siow8 (including 100 sinus CT scans with 200 sides), who reported that the feasibility of the prelacrimal recess approach in Chinese subjects was 93 per cent.
Lin et al.Reference Lin and Chen19 evaluated the treatment outcomes of the prelacrimal recess approach utilising the visual analogue and SNOT-22 scales in the management of different maxillary sinus pathologies: 9 lesions were sinonasal papilloma, 7 were other types of neoplasms (5 benign and 2 malignant), 2 were trauma-related and 4 were inflammatory diseases, with a total of 22 lesions (21 patients). They found that the prelacrimal recess approach could be used safely and efficaciously to manage various maxillary sinus lesions and could replace the other invasive procedures.
In our study, we highlight the importance of middle meatal antrostomy combined with the prelacrimal recess approach (two ports technique) for the management of cases where pathology exists in remote areas within the maxillary sinus, including antrochoanal polyp, isolated maxillary fungal ball and displaced dental structures into the maxillary sinus that are difficult to visualise and reach (such as the alveolar recess, pre-lacrimal recess and anterior or medial wall of the maxillary sinus). In such cases, middle meatal antrostomy might be insufficient to guarantee complete eradication of the pathology.
Contrary to Zhou et al.Reference Zhou, Han, Cui, Huang, Wei and Liu6,Reference Zhou, Han, Cui, Huang and Wang16 and Morrissey et al.Reference Morrissey, Wormald and Psaltis3, who proposed that removal of a part of the pyriform aperture allows better exploration of the maxillary sinus, we intended to preserve this part to avoid potential cosmetic drawbacks including collapse of the external nasal valve. In addition, we re-approximated the mucosal flap at the end of the procedure to position with one or two absorbable sutures to decrease the incidence of synechia and crusts post-operatively.
In a study by Comoglu et al.Reference Comoglu, Celik, Enver, Sen, Polat and Deger20 that included 12 patients with recurrent antrochoanal polyps, the prelacrimal recess approach was feasible in 83 per cent of patients (10 of 12), and they reported no recurrence during the follow up period of 14.2 months. Three patients developed synechiae between the lateral nasal wall and the nasal septum, and nasolacrimal duct injury occurred in two patients with no epiphora.
Another study by Lee et al.Reference Lee, Ahmad, Kim, Ryu, Kim and Dhong15 compared the prelacrimal recess approach with the Caldwell–Luc approach to remove benign maxillary sinus tumours. In the prelacrimal recess approach group, eight of the benign maxillary sinus tumours were inverted papillomas, one was an ameloblastoma and one was an ossifying fibroma. In the Caldwell–Luc approach group, all the 30 lesions were inverted papillomas. No recurrences were reported during follow up in either group (mean follow-up period was 10.8 months in the prelacrimal recess approach group and 13.0 months in Caldwell–Luc approach group). Regarding post-operative complications, 11 patients in the Caldwell–Luc approach group (37 per cent) and 3 patients in the prelacrimal recess approach group (30 per cent) had numbness around the cheek and upper lip area after surgery. The duration of facial numbness after the prelacrimal recess approach was shorter than for the Caldwell–Luc approach.
Based on our results, we believe that endoscopic middle meatal antrostomy combined with the prelacrimal recess approach is a good option for management of maxillary sinus pathology that may be out of reach through a conventional middle meatal antrostomy, provided that the prelacrimal recess is wide enough (more than 3 mm) and the open approaches are reserved for patients with a narrow prelacrimal recess (less than 3 mm). Our technique allowed efficient eradication of the described sinus pathologies while avoiding potential complications of the open approaches (e.g. the Caldwell–Luc approach) including facial swelling, facial paraesthesia, dental injuries and neo-osteogenesis of the maxillary sinus.
To our knowledge, we are the first to recommend closure of the prelacrimal window after removal of the pathology within the maxillary sinus to improve post-operative healing and avoid post-operative crusting and adhesions. We are the first to describe the prelacrimal recess as the ‘third window’ of the maxillary sinus, akin to that already used for the inner ear.
• There are certain areas that are out of reach endoscopically within the maxillary sinus (e.g. the anterior, anterolateral and inferior walls) in well pneumatised maxillary sinuses
• Open approaches, such as the Caldwell–Luc operation have many disadvantages, including facial swelling, facial paraesthesia, dental injuries and neo-osteogenesis of the maxillary sinus
• The prelacrimal recess approach is feasible in patients with a prelacrimal recess width greater than 3 mm
• The prelacrimal recess approach combined with a middle meatal antrostomy allows instrumentation through two channels to remove hard to reach pathology within the maxillary sinus
The limitations of our study include a relatively small sample size, a follow-up period that is shorter than needed to properly assess the long-term sequelae of the technique and any delayed recurrence. The absence of a control group was another limitation of our study because all our patients had a prelacrimal recess that favoured the endoscopic prelacrimal recess approach over the open approaches.
Conclusion
The prelacrimal recess approach combined with middle meatal antrostomy represents a good option for the management of difficult to reach maxillary sinus lesions. The prelacrimal recess approach improves visualisation and removal of certain maxillary sinus lesions with preservation of the middle turbinate and nasolacrimal duct and minimal morbidity in comparison to open approaches.
Competing interests
None declared






