Introduction
Acute coronary syndrome (ACS) is one of the leading causes of death in the world with more than three million deaths per year. Reference Mechanic, Gavin and Grossman1 In France, there are approximately 80,000 cases of ACS per year, including 12,000 deaths. 2 In the presence of chest pain leading to the suspicion of ACS, it is the interpretation of the electrocardiogram (ECG) that allows the diagnosis of patients with ST-elevation myocardial infarction (STEMI) or non-ST-elevation myocardial infarction (NSTEMI). Reference Ibanez, James and Agewall3 In France, suspected ACS is managed by medical teams of the Emergency Medical Services (EMS). While the management of STEMI is well-codified in the prehospital setting in France, the management of NSTEMI poses problems, mainly in terms of referral to an appropriate care pathway. Indeed, the medical team taking care of the patient has several means (including troponin measurement at point-of-care), but the risk stratification strategy allowing referral to an appropriate care pathway remains poorly evaluated.
The European Society of Cardiology (ESC; Brussels, Belgium) 2020 guidelines for NSTEMI propose an algorithm for management in the emergency department (ED) based on risk stratification. 4 The ESC 2020 algorithm is based, in addition to clinical data, ECG, and Global Registry of Acute Coronary Events (GRACE) score, Reference Collet, Thiele and Barbato5 on a troponin assay at H0 and then H1 or H2 depending on whether it is ultra or hypersensitive. An additional assay occurs at H3 if the previous assays are inconclusive with a clinic in favor of ACS. Patients are classified according to this algorithm into very high risk, high risk, and low risk. Reference Arslan, Damman and Zwart6 For the first two categories, management in a percutaneous coronary intervention (PCI) center is proposed with coronary angiography within one hour or 24 hours. For low-risk patients, management can be ambulatory after evaluation in the ED with an ischemia test or CT Colonography, followed or not by coronary angiography.
In France, some hospitals have an ED without a PCI center or a cardiac intensive care unit. Conversely, some facilities have a PCI center and a cardiac intensive care unit without an ED. It is therefore important to refer ACS patients to the right hospital with the right department. The goal is to avoid that a patient with NSTEMI, who turns out to be high risk or very high risk, is transported to a nearby ED without a downstream cardiac intensive care unit. This patient would need to be transferred secondarily to another hospital, delaying adequate management. Conversely, it is not always possible to drop all patients, including low-risk patients, directly into a cardiac intensive care unit.
As the ESC 2020 algorithm is not adapted to the decision making of patient orientation by the EMS medical team in the prehospital setting, the aim of this study was to search for clinical elements and examinations that can help orient patients. The main objective of the study was to search for a concordance between a negative troponin result in prehospital available to some French EMS medical teams and a diagnosis of NSTEMI classified as low risk. The secondary objectives were to: (1) analyze an influence of the time of onset of pain on the relationship between delocalized troponin and risk level; and (2) search for clinical and electrocardiographic criteria of out-of-hospital management predictive of a low-risk classification of the patient.
Material and Method
Study Design
This retrospective, monocentric, observational study took place at the EMS of Beaujon University Hospital, AP-HP (Paris region, France) from January 02, 2021 through June 31, 2021.
Population
Data were collected from the EMS software Interposition (@Jumping Group; Issy-Les-Moulinaux, France). The records of patients taken in charge for a primary intervention by EMS of Beaujon University Hospital, AP-HP (Paris region, France) from January 1, 2020 through December 31, 2020, in whom a point-of-care troponin assay was performed, were analyzed. Patients with a high-sensitivity cardiac troponin-I assay for suspected NSTEMI were included. Patients for whom troponin was performed for another indication (ie, STEMI or severity of SARS-CoV-2 pneumonia) were not included. Patients with missing data in the medical records that did not allow calculation of risk stratification were excluded.
Point-of-Care High-Sensitivity Cardiac Troponin-I Assay in the Prehospital Setting
A high-sensitivity cardiac troponin-I assay was performed prehospital before transport using Abbott cTnI cartridges (Abbott Laboratories; Chicago, Illinois USA) on the I-STAT-1 system with a measurement range of 3.2 to 50,000ng/L and a detection limit of 1.1 to 1.9ng/L. Sampling was performed by venipuncture on a dry tube. Troponin was considered positive above 4ng/L.4 Results were available within eight to twelve minutes.
Data Collection
At the EMS, all the ECGs were made in two copies: one copy intended for the service receiving the patient and one copy for the EMS file. The archived ECGs were recovered and interpreted by two experts. In case of disagreement between the two experts, a third expert analyzed the ECG to obtain a consensus in the interpretation. A copy of the troponin result was also available in the file. Socio-demographic data, history, time between onset of pain and start of care, and clinical data were collected from the EMS medical records. Troponin and creatinine determinations were collected from the ED records.
Classification of NSTEMI Patients Included in the Study
The GRACE score is used to calculate the probability of in-hospital and six-month mortality from the acute phase. Reference Collet, Thiele and Barbato5 It includes hemodynamic and clinical variables such as age, systolic blood pressure, heart rate, Killip classification, occurrence of cardiac arrest, ST-segment change, and biological variables with troponin increase and creatinine level. The patients were then classified into two groups according to the ESC 2020 guidelines: low-risk patients corresponding to patients who should be referred to the nearest ED and high-risk or very high-risk patients who should be referred to a PCI center or cardiac intensive care unit.
Statistics
Data were collected in Excel 2016 (Microsoft Corporation; Redmond, Washington USA). Statistical analyses were performed with SAS version 9.4 (SAS Institute; Cary, North Carolina USA). Continuous variables were described by mean and standard deviation (SD) or median and 1st and 3rd quartiles [Q1; Q3], depending on the distribution. The normality of the distribution was tested by a graphical method based on a frequency histogram and the Shapiro-Wilk test. Categorical variables were expressed as number (n) and percentage (%). Univariate comparative analysis between the two groups (ie, low risk and high risk or very high risk) was performed using a student t-test or an unpaired nonparametric Wilcoxon test in the case of continuous variables. Analysis of categorical variables used a Chi 2 test (or a Fisher test in case of expected number <five). Statistical interaction was sought to determine whether there was heterogeneity in the relationship between point-of-care troponin and risk level according to time to pain onset using logistic regression. The search for an association between point-of-care troponin and risk level was then conducted for each level of pain onset time: <three hours, three-to-six hours, and >six hours. A search for factors predictive of risk level and the role of troponin in this prediction were performed using multivariate logistic regression. The threshold of significance for alpha risk was five percent (P <.05).
Ethics
Data collection and storage by the Interpostion (@Jumping Group; Issy-Les-Moulinaux, France) EMS database was approved by the French National Commission for Data Protection and Liberties (Paris, France). All data were completely anonymous. In accordance with French law and in view of the retrospective nature of the study that evaluated professional practice, no patient consent was required. The Emergency Ethics Committee for Biomedical Research of Assistance Publique-Hôpitaux de Paris Nord approved this study (Paris, France; DAG-2020-P3-R2).
Results
Population
Over the study period, 309 patients received point-of-care troponin during management by the EMS team. Out of these 309 patients, 76 were excluded and 233 patients were included in the analysis (Figure 1). The mean age was 63 years [52;74]. There were 141 (61%) men and 92 (39%) women. The analysis of cardiovascular risk factors is given in Table 1. The time lapse (in hours) between the onset of pain and prehospital medical care by the EMS team was 10 hours [4;24]. Pain assessment showed a Numerical Rating Scale (out of ten) of four [0;6]. Hemodynamic data showed a heart rate (bpm) of 85 [70;85], systolic blood pressure of 150mmHg [130;170], and diastolic blood pressure of 90mmHg [40;145]. Out of the patients studied, only 22% had a baseline ECG and six percent had a change from their baseline ECG. A modified ECG was found in 61% of patients. The description of the ECG and the type of abnormality found are given in Table 2. Among the 233 patients, 153 (65.7%) were at low risk and 76 (32.6%) were at high or very high risk. The risk was undetermined for four (1.7%) patients.

Figure 1. Flow Chart.
Abbreviations: EMS, Emergency Medical Services; NSTEMI, non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction.
Table 1. Cardiovascular Risk Factors

Abbreviations: ACS, acute coronary syndrome; HDL, high density lipoprotein; HR, heart rate; LDL, low density lipoprotein.
Table 2. Characteristics of ECG

Abbreviations: ECG, electrocardiogram; EMS, Emergency Medical Services.
Univariate Comparative Analysis between the Two Risk Level Classes
Point-of-care high-sensitivity cardiac troponin-I assay was available for 227 patients. For three of the patients classified as low risk on the basis of the results of troponin measured in the hospital, there was no point-of-care troponin result. Point-of-care high-sensitivity cardiac troponin-I assay was negative in 143/150 (95.3%) low-risk patients versus 50/76 (65.8%) of patients classified as high or very high risk (P <.0001). The other differences found between patients classified as low risk and those classified as high or very high risk concerned age: 61 years (SD = 15) versus 66 years (SD = 16), respectively (P = .04); a history of atrial fibrillation: 136 (89%) versus 60 (79%), respectively (P = .04); and a history of coronary artery bypass surgery 149 (97%) versus 68 (89%), respectively (P = .02). Regarding the history and clinical examination data, typical pain was found in 11 (7%) patients classified as low risk versus 13 (17%) patients classified as high or very high risk (P = .02). The ECGs were normal in 83 (54%) and four (5%) patients classified as low risk and high or very high risk, respectively (P <.0001). The ECG abnormalities that were significantly different between the two groups were ST-segment depression and negative T wave. ST-segment depression was found in three (2%) versus 19 (25%) patients classified as low risk and classified as high or very high risk, respectively (P <.0001). The negative T wave was found in six (4%) versus 47 (62%) patients classified as low risk and classified as high or very high risk, respectively (P <.0001). The variables analyzed in univariate analysis are presented in Table 3.
Table 3. Univariate Comparative Analysis of Low-Risk versus High- and Very High-Risk Patients

Abbreviations: ACS, acute coronary syndrome; ECG, electrocardiogram; EMS, Emergency Medical Services; HDL, high density lipoprotein; LDL, low density lipoprotein; NRS, numerical rating scale.
Subgroup Analysis Looking for an Influence of Time to Pain on the Relationship between Delocalized Troponin and Risk Level
The interaction between point-of-care troponin and time to pain onset was not significant (P = .86). Point-of-care troponin was significantly more often positive in high- or very high-risk patients than in low-risk patients, regardless of time to pain onset; the adjusted OR for time to pain onset is 9.36 (95% CI, 3.97-22.08). Table 4 shows the point-of-care troponin results according to time to pain onset.
Table 4. Influence of Time to Pain Onset on Relationship between Prehospital Point-of-Care Troponin and Risk Level

Multivariate Analysis for Factors Predicting Risk Level and Place of Point-of-Care Troponin
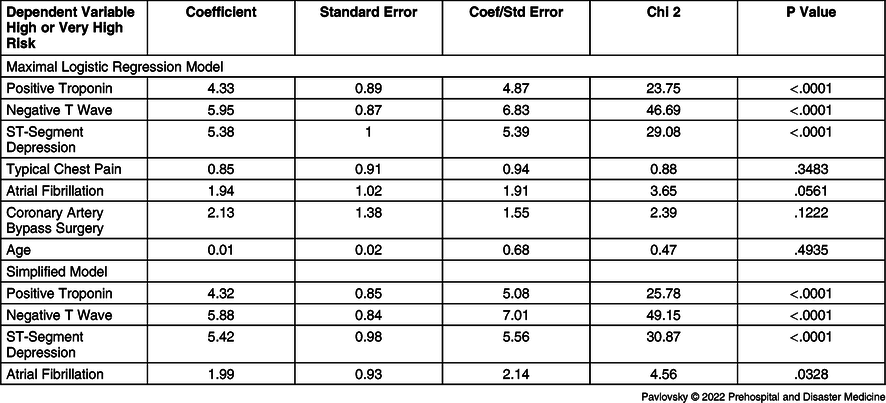
Factors associated with risk level in univariate analysis were considered in a maximal logistic regression model (R2=68%; Table 5). After simplification of the model (Table 5), the predictors of a high or very high level of risk were: positive point-of-care troponin (P <.0001), ST-segment depression (P <.0001), negative T wave (P <.0001), and a history of cardiac arrhythmia by atrial fibrillation (P = .03). The multiple explanation coefficient of this simplified model was R2=66% and decreased to 52% after removal of delocalized troponin. The simplified model predicted risk level with an accuracy (rate of well-classified) of 92%. Most high-risk and very high-risk patients (85%) were well-predicted in this risk class by the model. Low-risk patients were even more accurately predicted by the model (95%).
Table 5. Multivariate Analysis of Predictors of Risk Level
Discussion
During prehospital medical management of NSTEMI by the EMS, point-of-care determination of positive high-sensitive troponin-I is predictive of risk level. In clinical practice, cardiac troponin concentrations are interpreted in conjunction with the ECG and clinical assessment. Reference Chapman, Lee and McAllister7 In the present study, age, a history of atrial fibrillation or coronary artery bypass surgery, and the typical appearance of pain and repolarization abnormalities on the ECG were also predictive of risk level. After simplification of the model, positive troponin, electrocardiographic abnormalities such as ST-segment depression and negative T wave, and a history of atrial fibrillation arrhythmia were found to be independent predictors of high or very high risk. Subgroup analysis by time of onset showed that positive troponin was statistically associated with high/very high risk in each subgroup. In a recent metanalysis of 19 prospective study cohorts, negative predictive value (NPV) and sensitivity were excellent for a risk stratification threshold of less than 5ng/L in the subgroup of patients without myocardial ischemia on ECG. Reference Chapman, Lee and McAllister7 Authors’ conclusions gave NPV of 99.7% (95% CI, 99.4%-99.8%) and sensitivity of 99.0% (95% CI, 97.3%-99.6%), identifying 45.9% of patients as low risk, with 4.4 (95% CI, 3.0-6.0) false negatives per 1,000 patients and a positive predictive value (PPV) of 24.5% (95% CI, 20.3%-29.2%).
In a prospective, single-center study conducted in Denmark from 2012 through 2015, in which all EMS ambulances were equipped with point-of-care troponin, Reference Rasmussen, Stengaard and Sørensen8 the population was comparable. The study population was predominantly male 64% (versus 63% in the present study), with an average age of 70 years (versus 63 years), and with at least one cardiovascular risk factor, including 25% of patients with ischemic heart disease (versus 33%). Patients with troponin above 50ng/L in suspected ACS had 20% increased one-year mortality. In this study, on-board troponin had sensitivity of 44% and specificity of 93%. In the present study, the analysis of history, repolarization abnormalities, and the use of point-of-care troponin allowed proper classification of 85% of NSTEMI patients considered at high or very high risk. This means that perhaps 15% could have been referred to a local ED. More importantly, this combined clinical, electrical, and biological analysis in the prehospital setting correctly classified 95% of NSTEMI patients as low risk. This result means that referral to the local ED can be made without risk of loss of time and chance for the patient, even if the hospital does not have a PCI center and a cardiac intensive care unit.
Other factors that appeared predictive of a high level of risk were age, history of coronary artery bypass surgery, atrial fibrillation, typical pain, and electrocardiographic changes. It is clear that these are important factors in assessing risk. They are also included in the algorithm of the ESC 2020 recommendations associated with the GRACE score. Reference Collet, Thiele and Barbato5,Reference Eagle, Lim and Dabbous9 In the literature, two studies were found that stratify the level of risk according to a HEART (History, ECG, Age, Risk Factors, Troponin) score that combines these clinical and electrocardiographic criteria with prehospital troponin determination. In a prospective multicenter cohort study from January 2016 through July 2017 in Holland, including 700 patients, nurses were asked to test a HEART score with prehospital troponin. The primary endpoint was the occurrence of major cardiac events (death, myocardial infarction, NSTEMI/STEMI, unstable angina, or revascularization) at 45 days. Major events occurred in five patients (2.9%) in the low-risk group (HEART score <three) and in 111 (21.0%) patients with intermediate or high risk (P <.001). Reference Van Dongen, Tolsma and Fokkert10 Another retrospective study conducted at two centers in the USA from 2013 through 2014 investigated a modified prehospital HEART score predictive of major cardiac events (death, myocardial infarction, or revascularization) in patients with suspected NSTEMI. This modified HEART score showed sensitivity of 94% and NPV of 98%. Reference Stopyra, Harper and Higgins11 The simplified model of multivariate analysis highlighted that atrial fibrillation is a predictor of risk level stratification. Atrial fibrillation, as a public health burden, is well-known to be risk factor for ACS, Reference Soliman, Safford and Muntner12 stroke, heart failure, and to be associated with a higher morbidity and mortality. Reference Benjamin, Chen and Bild13
Finally, in the present study, subgroup analysis by time to pain onset showed that positive troponin in the prehospital setting was statistically associated with high/very high risk regardless of time to pain onset. In the meta-analysis by Chapman, et al, Reference Chapman, Lee and McAllister7 population was stratified by time since symptom onset on two groups: ≤two hours or >two hours. Unfortunately, PPV was not specified. Results suggests the NPV of myocardial infarction or cardiac death within 30 days was lower in those who presented within two hours of symptom onset (99.0% [95% CI, 97.7%-99.5%]; [n = 2303] versus 99.6% [95% CI, 99.4%-99.8%]; [n = 11 101]; P = .003). The size of the population in the present study could explain why such a small difference could not be significant. Furthermore, the objective of the current study was to investigate the predictive factors of being well-classified as high- or very high-risk NSTEMI in order to refer these patients not to the nearest hospital, but to a hospital with a PCI center and cardiology intensive care unit. It is therefore important that troponin testing be positive in high-risk/very high-risk patients, regardless of the time lapse between onset of pain and management of these patients.
The study conducted is original and useful, given the limited literature on the value of troponin in prehospital risk stratification. The lack of data in the prehospital setting is probably related to the need for management by a medical or paramedical team authorized to take blood samples in the prehospital setting, which is not the case in all countries. In addition, these teams must be able to perform point-of-care biological analyses. The major issue concerning the management of NSTEMI in the prehospital setting is optimization of the care pathway. Directing the patient to the appropriate hospital and department according to risk is essential so that the patient can benefit from the appropriate technical platform and from receiving treatment at the right time. Troponin measurement therefore appears to be a powerful tool in risk stratification and the resulting management. Nevertheless, the interest of a prospective multicenter study is obviously to increase the external validity of troponin measurement in prehospital care. In fact, the study was conducted in a Parisian EMS in France, where patients are managed in an area where there are several hospitals and clinics with or without PCI center and cardiac intensive care unit. The interest is certainly less important in medium-sized cities that have only one hospital with an adapted technical platform since all patients are directed to this hospital. On the other hand, the interest could be more important for isolated sites where there are only small hospitals with insufficient technical facilities and where a higher-level hospital with sufficient technical facilities is distant. For these patients, a good classification from the prehospital management could be essential. In addition, construction of a score applicable in prehospital combining troponin with clinical and electrocardiographic criteria could be useful for standardization of the management of patients suspected of NSTEMI.
Limitations
This study is not without limitations. It was a retrospective study with inherent types of bias such as selection bias and information bias. The records were not standardized and sometimes lacked data. For example, the typical pain variable was not standardized in advance and was left to the subjectivity of the EMS physician. The recruitment bias appears to be unavoidable because the patients recruited all contacted a certified call center for chest pain and were managed by the EMS. Triggering of a medical ambulance from the EMS was based on cardiovascular risk factors (age and cardiovascular history in particular), as well as clinical criteria such as the presence of typical pain and its time of onset. The likelihood of patients being enrolled in the study is related to several of the factors studied. Lastly, the monocentric nature of this study with a small sample did not allow to be free of geographic and ethnic selection biases.
Conclusion
The management algorithm for patients with NSTEMI is based on risk stratification according to clinical, electrocardiographic, and biological data performed in the hospital. There exists no recommendation for risk stratification in prehospital management. The use of point-of-care troponin, associated with clinical and ECG criteria, seems to allow classification of patients suspected of having NSTEMI as early as prehospital management and to optimize referral to an adapted care pathway. The use of troponin in point-of-care by EMS medical teams appears to be a valuable aid in directing the patient in prehospital care to a hospital with a PCI center and cardiology intensive care unit if the assay is positive, and to a local ED, even if the hospital does not have the technical platform, when the troponin assay is negative.
Conflicts of interest/funding
None of the authors have any financial conflicts of interest in connection with the work to disclose. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors would like to thank Jeffrey Arsham, an American scientific translator, for having reviewed the English language text.









