Introduction
Tympanoplasty is one of the most common surgical procedures performed in the otorhinolaryngology field.Reference Liu, Yu, Shiao and Wang1 It is performed to repair perforation due to otitis media, traumatic rupture or post-operative complications, and to restore the function of the middle ear.Reference Naderpour, Jabbari Moghadam, Ghanbarpour and Shahidi2,Reference Anzola and Nogueira3 Despite the advances in antibiotic treatment, middle-ear infections and the subsequent tympanic membrane perforations remain a common otological problem. This makes it imperative that otolaryngology residents are adequately exposed to, and gain experience in, tympanoplasty.
Although simulation-based training helps trainees develop surgical skills in a controlled and safe environment,Reference Owa, Gbejuade and Giddings4,Reference Piromchai, Ioannou, Wijewickrema, Kasemsiri, Lodge and Kennedy5 there is no substitute for hands-on training on the specific techniques and intra-operative decision making. In our training programme, residents spend five training years in the residency programme. During their first three years, they receive audio-visual instructions while working as assistants in tympanoplasty procedures. Fourth- and fifth-year residents (junior trainees), and otology fellows (senior trainees), usually perform the procedure on their own.
Although tympanoplasty is a common procedure, complications can occur in the early post-operative course. These include bleeding, wound infection, facial nerve palsy, tinnitus, dizziness, ear discharge, ear pain and taste disturbance. In addition, complications can occur in the late post-operative course, including surgery failure and perforation recurrence.Reference Emir, Ceylan, Kizilkaya, Gocmen, Uzunkulaoglu and Samim6
Although the effects of resident participation on hospital charges, patient care and surgical outcome have been investigated across various surgical disciplines,Reference Wexner, Rosales-Velderrain, Wexner and Rosenthal7–Reference Cobb, Eguia, Janjua and Kuo14 including otolaryngology,Reference Pollei, Barrs, Hinni, Bansberg and Walter15–Reference Baker, Ong, O'Connell, Sokohl, Clinkscales and Meyer17 the impact on the outcome of tympanoplasty still remains to be studied. Most recent studiesReference Wexner, Rosales-Velderrain, Wexner and Rosenthal7–Reference DiDato, Farber, Rybin, Kalish, Eslami and Moreira10,Reference Cobb, Eguia, Janjua and Kuo14,Reference Pollei, Barrs, Hinni, Bansberg and Walter15 have reported an association between resident involvement and longer operative time. However, some studies have reported contradictory findings. Uecker et al.Reference Uecker, Luftman, Ali and Brown13 found comparable operative time in surgery performed with or without resident involvement. Moreover, Cvetanovich et al.Reference Cvetanovich, Schairer, Haughom, Nicholson and Romeo11 found that resident participation had a favourable effect on operative time. Similar conflicting results exist for length of hospital stay and complications.Reference Cvetanovich, Schairer, Haughom, Nicholson and Romeo11,Reference Uecker, Luftman, Ali and Brown13,Reference Jackson, Wannares, Lancaster, Rattner and Hutter18
The Saudi Commission for Health Specialties mandates that residents and fellows must achieve a minimum number of listed tympanoplasty and tympano-ossiculoplasty procedures before graduation. We aimed to assess the clinical outcomes of tympanoplasty performed by otorhinolaryngology trainees compared to those of tympanoplasty performed by consultants, in terms of operative complications, operation time and audiological outcome (hearing improvement).
Materials and methods
Study design and setting
This retrospective observational cohort study aimed to investigate the outcome of tympanoplasty based on the type of primary surgeon performing the procedure. The target population consisted of all subjects who underwent tympanoplasty or tympano-ossiculoplasty performed by a consultant, senior trainee or junior trainee, from 2012 to 2015, at a tertiary university hospital.
Inclusion and exclusion criteria
The inclusion criterion was all adult subjects who underwent tympanoplasty or tympano-ossiculoplasty. The exclusion criteria were: incomplete patient data, including all patients with no follow-up information; patients who underwent another procedure (e.g. mastoidectomy) in addition to tympanoplasty; and revision surgical procedures.
Sampling technique
All adult patients who were operated between 1 January 2012 and 31 December 2015 were included. A total of 689 patient files were initially screened; 291 subjects were excluded according to the exclusion criteria.
Data collection methods
The data collectors reviewed the subjects’ medical records and completed the online forms with the following target parameters: surgical data, operative time, surgical outcome and audiological outcome. Surgical data included: type of surgery (tympanoplasty or tympano-ossiculoplasty); primary tympanoplasty or revision surgery; operative time; surgical approach (end-aural or retro-auricular); and position of primary surgeon (i.e. consultant, senior trainee (otology fellows) or junior trainee (R4 or R5 residents)). Operative time was calculated as the time elapsed from wound incision to closure. Surgical outcome was evaluated by investigating the complications, which were divided into intra-operative, early post-operative (24 hours or less) or late post-operative (more than 24 hours). Audiological outcome was determined according to hearing improvement, evaluated both subjectively (by referring to clinic follow-up notes, and whether the patient had noticed hearing improvements) and objectively (by pure tone audiometry (PTA)).
Statistical analysis
All data were entered into SPSS® statistical software, version 21. The chi-square test was used to assess for statistically significant differences (p-value of less than 0.05) among the participants. The statistical outlier method was used to detect entry errors.
Ethical considerations
This study was approved by the institutional review board at a university hospital. We ensured participant confidentiality by assigning each participant with a code number for analytical purposes only.
Results
A total of 398 tympanoplasty and tympano-ossiculoplasty surgical procedures were included in the final analysis. Among the surgery patients, 178 (44.7 per cent) were males and 220 (55.3 per cent) were females. The patients’ mean age was 36 years. Regarding the type of surgery, 336 (84.4 per cent) were tympanoplasty procedures, which represented the majority, and 62 (15.6 per cent) were tympano-ossiculoplasty procedures. In regard to the primary surgeon, 283 (71.1 per cent) surgical procedures were performed by junior trainees, 71 (17.8 per cent) by consultants and 44 (11.1 per cent) by senior trainees (Figure 1).
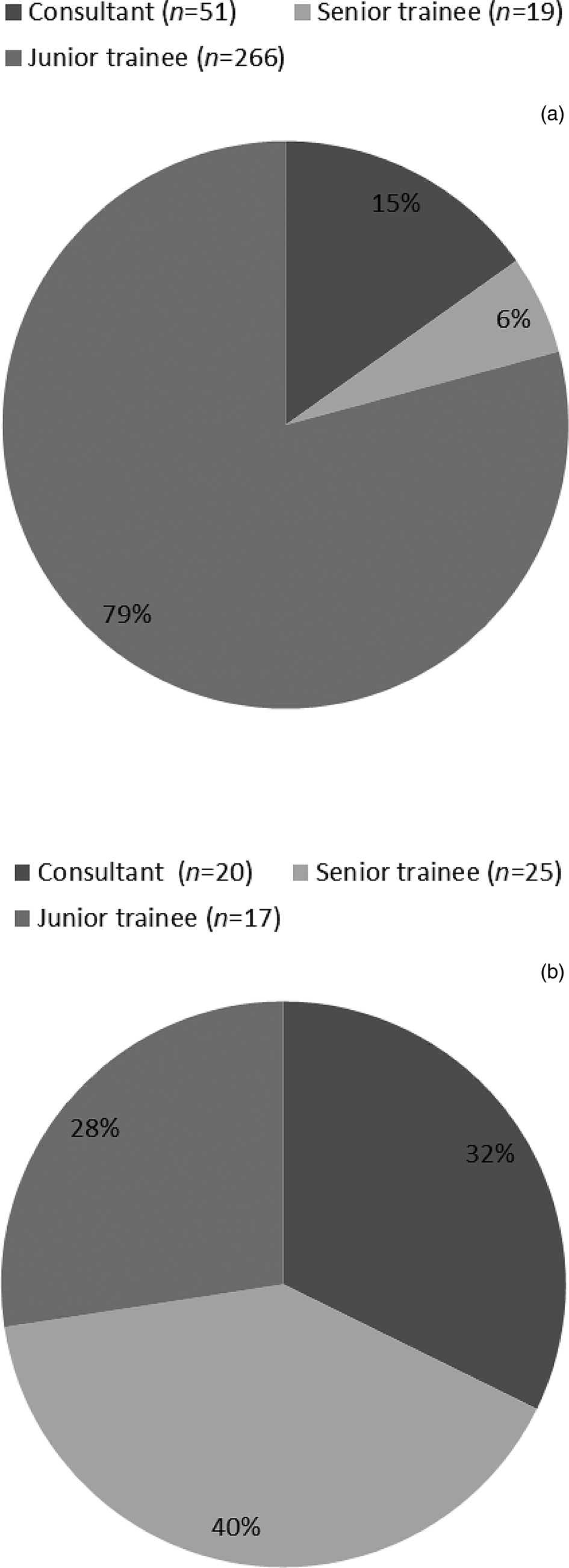
Fig. 1. Distribution of (a) tympanoplasty and (b) tympano-ossiculoplasty procedures performed by consultants, senior trainees (fellows) and junior trainees (residents).
We calculated the operative time to determine the influence of trainee involvement on the duration of surgery. Our results showed a statistically significant difference (p < 0.001) in the operative time among consultants, senior trainees and junior trainees. Consultants were associated with the shortest mean operative time for tympanoplasty and tympano-ossiculoplasty (110 minutes and 147 minutes, respectively). The junior trainee group had the longest mean operative time for tympanoplasty and tympano-ossiculoplasty (144 minutes and 155 minutes, respectively). The mean operative time of the senior trainees for tympanoplasty and tympano-ossiculoplasty was 126.8 minutes and 155 minutes, respectively (Figure 2).

Fig. 2. Comparison of operative times between consultants, senior trainees (fellows) and junior trainees (residents).
There was no statistically significant difference in the duration of hospitalisation (p = 0.06) among the consultants, fellows and residents. Table 1 shows the average duration of hospital stay (in days).
Table 1. Duration of hospitalisation

Data represent days of hospitalisation, unless indicated otherwise. There was no statistically significant difference in hospitalisation duration between junior trainees (residents), senior trainees (fellows) and consultants (p = 0.06).
In order to assess the safety of surgery performed by trainees, we compared the incidence of complications among the three different groups. There were no statistically significant differences among consultants, senior trainees and junior trainees in terms of complications for tympanoplasty and tympano-ossiculoplasty (p = 0.294 and p = 0.568, respectively). The overall operative complication rate for tympanoplasty was 34.2 per cent, while that for tympano-ossiculoplasty was 53.2 per cent. The highest complication rates in tympanoplasty and tympano-ossiculoplasty surgery were found in the trainee group (Tables 2 and 3).
Table 2. Complications of tympanoplasty

There was no statistically significant difference in tympanoplasty-related complications between junior trainees (residents), senior trainees (fellows) and consultants (p = 0.294). Intra-op = intra-operative; post-op = post-operative
Table 3. Complications of tympano-ossiculoplasty

There was no statistically significant difference in tympano-ossiculoplasty related complications between junior trainees (residents), senior trainees (fellows) and consultants (p = 0.568). Intra-op = intra-operative; post-op = post-operative
Lastly, we measured the outcome of surgery in terms of subjective and objective hearing improvement. There was no statistically significant difference in subjective hearing improvement among consultants, fellows and residents (p = 0236). Among the patients included, 210 (52.8 per cent) had subjective hearing improvement, 93 (23.4 per cent) had no change, 90 (22.6 per cent) had no report and only 5 (1.3 per cent) had decreased hearing. Objective hearing improvement, assessed using PTA, showed no statistically significant difference in post-operative air–bone gap improvement among consultants, fellows and residents (p = 0.848) (Table 4).
Table 4. Air–bone gap values

Data represent air–bone gap values (in dB). There was no statistically significant difference in post-operative air–bone gap improvement between junior trainees (residents), senior trainees (fellows) and consultants (p = 0.848). ABG = air–bone gap; pre-op = pre-operative; post-op = post-operative
Discussion
The present study investigated the overall effect of trainee involvement in performing tympanoplasty and tympano-ossiculoplasty on outcomes. Our results indicate that the involvement of senior or junior surgical trainees does not affect the surgical quality and peri-operative outcomes; however, the surgery takes longer.
Over the past few years, there has been great debate regarding the outcomes of surgical procedures involving trainees and the safety of procedures performed by residents. Several single-institution and large multi-institution studies have evaluated the effect of trainee participation on surgical outcomes. Previous studies have reported mixed results regarding the impact of involving trainee surgeons, in a variety of surgical specialties.Reference Wexner, Rosales-Velderrain, Wexner and Rosenthal7–Reference Pollei, Barrs, Hinni, Bansberg and Walter15,Reference Fiorini, Santoro, Deganello, Mannelli, Meccariello and Gallo19–Reference Schrand, Hussain, Dunki-Jacobs and Grannan24 There have been relatively limited studies in otolaryngology,Reference Liu, Yu, Shiao and Wang1,Reference Pollei, Barrs, Hinni, Bansberg and Walter15–Reference Baker, Ong, O'Connell, Sokohl, Clinkscales and Meyer17 especially on the impact of specific procedures. A thorough literature review revealed that the impact of resident participation has only been investigated in open tracheostomy.Reference Fiorini, Santoro, Deganello, Mannelli, Meccariello and Gallo19 Another study explored the learning curve of tympanoplasty type I in different residency levels.Reference Liu, Yu, Shiao and Wang1
Our results further confirm that the presence of a junior or senior trainee is associated with a longer operative time compared to that of consultants. Compared to tympanoplasty, the mean operative time for tympano-ossiculoplasty was higher for all three surgeon groups, which could be attributed to the complexity of the procedure. However, the trend for a decrease in the operative time associated with seniority and experience was maintained. For tympanoplasty, there was no significant difference in the operative time between junior and senior trainees, which might be explained by the fact that the junior trainees were always supervised by either consultants or senior trainees.
Most previous studies assessing the operative times have similarly reported that trainee involvement is associated with longer surgery duration.Reference Wexner, Rosales-Velderrain, Wexner and Rosenthal7,Reference Feeney, Price, Chen, Graham and Chatterjee8,Reference DiDato, Farber, Rybin, Kalish, Eslami and Moreira10 In contrast, Cvetanovich et al.Reference Cvetanovich, Schairer, Haughom, Nicholson and Romeo11 analysed 1382 patients and found that resident involvement in total shoulder arthroplasty had a positive effect on both surgery duration and hospital stay. A study that evaluated residents throughout their training found that residents in their fourth and fifth years spent more time in surgery than when they were in their sixth and seventh years.Reference Liu, Yu, Shiao and Wang1 Similar results were also reported by a study involving general surgery procedures.Reference Feeney, Price, Chen, Graham and Chatterjee8
We found no statistically significant differences in the surgical complications among the primary surgeons who performed the procedures (consultants, senior trainees or junior trainees). This indicates that the procedure can be performed safely by trainees. Previous otolaryngology studies have reported similar results.Reference Liu, Yu, Shiao and Wang1,Reference Naderpour, Jabbari Moghadam, Ghanbarpour and Shahidi2,Reference Emir, Ceylan, Kizilkaya, Gocmen, Uzunkulaoglu and Samim6,Reference Pollei, Barrs, Hinni, Bansberg and Walter15–Reference Baker, Ong, O'Connell, Sokohl, Clinkscales and Meyer17,Reference Fiorini, Santoro, Deganello, Mannelli, Meccariello and Gallo19 In addition, reports for other surgical specialties also found no statistically significant difference between staff and trainees in terms of the intra- or post-operative complication rates.Reference Wexner, Rosales-Velderrain, Wexner and Rosenthal7,Reference Feeney, Price, Chen, Graham and Chatterjee8,Reference DiDato, Farber, Rybin, Kalish, Eslami and Moreira10,Reference Cvetanovich, Schairer, Haughom, Nicholson and Romeo11,Reference Uecker, Luftman, Ali and Brown13 However, other studies have reported that resident participation increases the complication rate,Reference Jackson, Wannares, Lancaster, Rattner and Hutter18,Reference Dasani, Simmons, Wirtalla, Hoffman and Kelz20 and that the complication rate increases in emergency surgical procedures (e.g. appendectomy and explorative laparotomy).Reference Scheer, Martel, Moloo, Sabri, Poulin and Mamazza25
In 2016, Vieira et al.Reference Vieira, Hernandez, Qin, Smith, Kim and Dutra16 published the first study using American College of Surgeons National Surgical Quality Improvement Program data to analyse the impact of resident participation in otolaryngology surgery. They collected data on laryngectomy, neck dissection, tonsillectomy and adenoidectomy, thyroidectomy, tongue and floor of the mouth surgery, and salivary gland surgery performed in both academic and non-academic hospitals. However, their data did not include tympanoplasty or tympano-ossiculoplasty. They reported longer operative times, higher morbidity and higher mortality in cases with resident involvement in unadjusted analyses. They explained that as academic hospitals were likely to deal with both medically and surgically complex cases, resident involvement would be associated with more complex cases. Therefore, after controlling for the higher rates of resident involvement in more complex and longer operations, as well as bias related to an attending's selection of ‘teaching cases’, the analysis showed no difference in morbidity and mortality.
Baker et al.Reference Baker, Ong, O'Connell, Sokohl, Clinkscales and Meyer17 specifically evaluated out-patient surgical procedures in otolaryngology, including tympanoplasty, but not tympano-ossiculoplasty, using the American College of Surgeons National Surgical Quality Improvement Program database. For those procedures, resident participation was associated with longer surgical time, but it did not have any negative impact on complications.
• Tympanoplasty is commonly performed in ENT; it is imperative that ENT residents are adequately exposed and gain experience in this procedure
• The impact of ENT resident involvement on tympanoplasty or tympano-ossiculoplasty outcomes has not been previously reported
• Trainee participation increased operative times, with no negative impact on tympanoplasty or tympano-ossiculoplasty outcomes and complication rates
• A high level of trainee involvement enhances the quality of otolaryngology surgical education
• This involvement can be maintained with no adverse effects on surgical complication rates and outcomes
In the current study, there was no statistically significant difference in the duration of hospitalisation among the three surgeon groups. Similar results were reported by studies evaluating general surgery procedures.Reference Jackson, Wannares, Lancaster, Rattner and Hutter18 However, other studies have reported that the hospital length of stay is shorter when residents are involved.Reference Cvetanovich, Schairer, Haughom, Nicholson and Romeo11 This has been attributed to patients being seen early in the morning and more frequently, as well as the availability of more personnel to discharge patients.Reference Uecker, Luftman, Ali and Brown13 In our hospital, the post-operative care of patients is the same regardless of whether the primary surgeon is a trainee or consultant; this contributed to the similar length of stay in the hospital between the groups.
The major limitation of this study is that it was conducted in a single centre. Therefore, a multicentre study is recommended for stronger evidence.
Conclusion
Although trainee participation in tympanoplasty and tympano-ossiculoplasty surgery results in a clinically appreciable increase in the operative time, it does not affect other peri-operative outcomes, and thus appears to be safe. Therefore, we recommend that residents are allowed to perform these surgical procedures under direct supervision, especially in teaching institutions.
Acknowledgement
We thank Dr Shahad Alawwad, who worked with us when submitting the study proposal to the institutional review board and when collecting data.
Competing interests
None declared








