Introduction
Malignant otitis externa is an acute infective process of the external auditory canal, which spreads via the fissures of Santorini at the osseous-cartilaginous junction to involve the infratemporal fossa. This may progress if untreated, causing osteomyelitis and involving the skull base, with subsequent lower cranial nerve weakness.Reference Mehrotra, Elbadawey and Zammit-Maempel1
Recent UK studiesReference Pankhania, Bashyam, Judd and Jassar2 and Hospital Episode Statistics data appear to show a significant and concerning increase in malignant otitis externa cases (the first case series was described by Chandler in 1968Reference Chandler3). In this prospective case series, we analysed malignant otitis externa patients presenting to a tertiary hospital over a 12-month period. The aim was to identify possible causative factors and prognostic indicators, and through these data develop a local standardised treatment pathway.
Materials and methods
All cases of malignant otitis externa (necrotising otitis externa and skull base osteomyelitis) diagnosed in a tertiary referral ENT department over 12 months were included in this study. A single otologist reviewed and confirmed all diagnoses of malignant otitis externa, and acted as lead role in therapeutic management alongside a multidisciplinary team (MDT) involving microbiologists, radiologists and infectious disease consultants.
The data collected included: age; gender; pre-existing medical co-morbidities (e.g. diabetes mellitus and other causes of immunosuppression); possible precipitating events; presenting signs and symptoms; microbiology culture results; histology findings; trends in erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and glycosylated haemoglobin (haemoglobin A1c or ‘HbA1c’); radiology results; choice and length of antimicrobial treatment, with any subsequent changes; treatment duration; other treatments or surgical procedures; recurrences; re-admissions; and any fatalities.
Results
Within the 12-month study period, a total of 16 patients were diagnosed with malignant otitis externa (11 males and 5 females), with a mean age of 72 years (range, 40–89 years). Male patients were found to have a lower mean age compared to females, 68 years and 80 years respectively.
Four patients (25 per cent) directly reported a preceding event in the days before they developed initial symptoms: ear syringing in three individuals and trauma from excessive ear cleaning in the other.
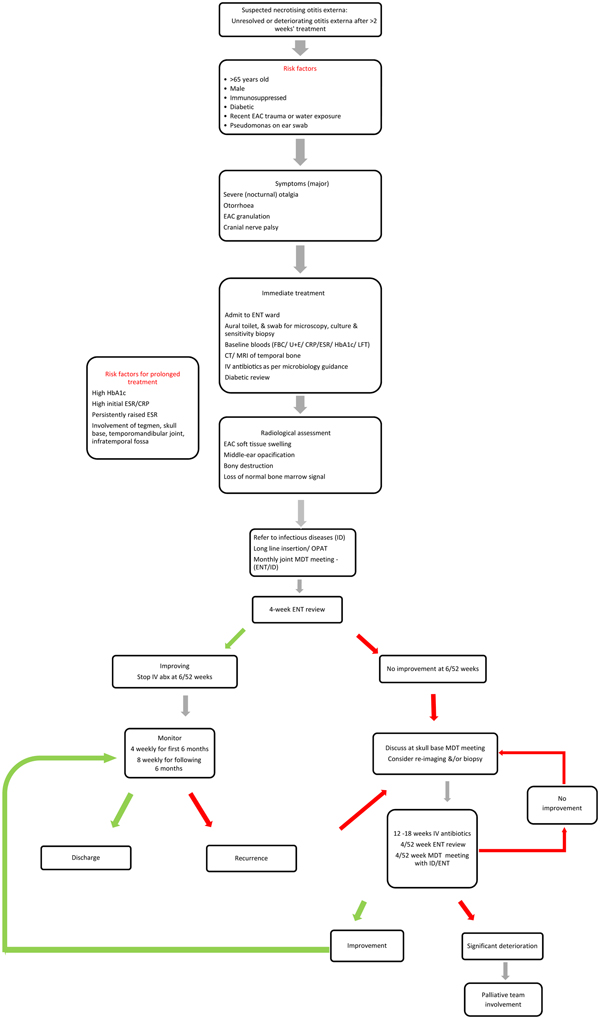
The commonest presenting symptoms were otorrhoea and otalgia, affecting all 16 cases, with otalgia marked as severe, often at night. Figure 1 outlines the other common presenting symptoms and clinical signs within our malignant otitis externa cohort.

Fig. 1. Clinical signs and symptoms on initial presentation observed within our cohort of 16 malignant otitis externa patients. EAC = external auditory canal; CN = cranial nerve
A total of 11 patients (69 per cent) had a pre-existing diagnosis of diabetes mellitus: 9 had type II diabetes mellitus (5 of whom required insulin injections) and 2 had type I insulin-controlled diabetes mellitus. Of the five non-diabetic patients, two were on immunosuppressive medication for rheumatoid arthritis, one had received previous radiotherapy to the head and neck, and one was under the care of the haematology department with a diagnosis of acute myeloid leukaemia. Risk factors for the cohort are outlined in Table 1.
Table 1. Co-morbidities and pre-existing risk factors in malignant otitis externa patients*

* Total n = 16
Inflammatory markers, as well as haemoglobin A1c levels, were tested on admission in those with known diabetes mellitus. The results, including the mean and range for each variable, are outlined in Table 2 and Figure 2. The ESR was raised in 12 patients (78 per cent) and was within a normal range in 3 patients (less than 15 mm/hour); testing was not performed initially in 2 patients. A CRP test was undertaken in 15 patients and was found to be raised in 80 per cent. Haemoglobin A1c levels were recorded in 10 of the 11 diabetic patients, but were not routinely evaluated in non-diabetic patients. Levels of glycosylated haemoglobin reflect the mean glucose concentration in the preceding 8–12 weeks, and thus provide a surrogate marker for longer-term diabetic control. In our diabetic cohort, the mean haemoglobin A1c level on admission was 78.9 mmol/mol, significantly higher than the upper limit of normality at 48 mmol/mol.
Table 2. Inflammatory marker and glycosylated haemoglobin levels on admission in malignant otitis externa patients

* Normal result upper limits within our laboratory. ESR = erythrocyte sedimentation rate; CRP = C-reactive protein

Fig. 2. Initial erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) and haemoglobin A1c (HbA1c) (if applicable) levels on admission, for each individual patient with a clinical diagnosis of malignant otitis externa. The upper limits of normal results for our laboratory are: ESR = 15 mm/hour, CRP = 5 mg/l and haemoglobin A1c = 48 mmol/l.
All patients underwent computed tomography (CT) of the temporal bone on admission. Subsequent magnetic resonance imaging (MRI) was arranged for all but two patients who had contraindications (i.e. a pacemaker in situ). The most commonly reported finding on initial CT was external auditory canal inflammation and soft tissue thickening, present in 100 per cent of scans. This was followed by inflammatory changes and opacification in the middle ear and mastoid air cells. Bony destruction was seen in 4 of the 16 initial CT scans, with MRI imaging confirming bone marrow enhancement in all 4, in keeping with evidence of underlying osteitis or osteomyelitis. No intracranial complications were reported. Table 3 highlights the commonest findings with both imaging modalities.
Table 3. Incidence of radiological findings in malignant otitis externa patients on initial MRI and CT imaging
MRI = magnetic resonance imaging; CT = computed tomography; TMJ = temporomandibular joint
Pseudomonas aeruginosa was the commonest organism cultured on microscopy of external auditory canal swabs, being positive in 12 patients (75 per cent). One patient also grew concomitant candida and another grew enterococcus. The reported antimicrobial sensitivities varied in this pseudomonas cohort, with the commonest being ceftazidime, Tazocin® and gentamicin. Three cases of antimicrobial resistance were recorded: ciprofloxacin in two patients and gentamicin in one. The full results are outlined in Table 4.
Table 4. Microscopy and culture results for malignant otitis externa patients on admission*
* Swabs taken from external auditory canal. N/A = not applicable
The most common first-line antimicrobial used on admission was Tazocin – a combination of the antibiotic piperacillin and the beta-lactamase inhibitor tazobactam – which was started in 75 per cent of patients. This was followed by ceftazidime in four patients, three of whom received combination therapy with one other antimicrobial (flucloxacillin, teicoplanin or metronidazole).
The mean length of hospital stay was 19.3 days (range, 8–36 days), which was often prolonged by inadequate social care packages and the need to ensure adequate provision for improved diabetic care monitoring.
The average length of antibiotic treatment, which continued until the condition was deemed to be in remission, was 17.4 weeks (range, 6–35 weeks). Those patients with evidence of bony involvement of the temporomandibular joint, infratemporal fossa and tegmen tympani required a prolonged treatment course. The average number of antibiotics used throughout treatment was 2.9 per patient (range, 1–5 antibiotics), with an average of 1 antibiotic treatment change per patient (range, 0–3 changes).
Complications related to the antibiotic therapy were minimal. One patient experienced an allergic rash, one developed an acute kidney injury on a background of chronic kidney disease, and one developed clostridium difficile infection. The patient with pre-existing acute myeloid leukaemia developed neutropenia. There was one mortality within the study period; however, this was expected (occurring in a palliatively treated patient) and was not a direct result of malignant otitis externa.
Discussion
From the 1990s, Hospital Episode Statistics data have demonstrated a steady increase in admissions in England coded as malignant otitis externa.Reference Chawdhary, Liow, Democratis and Whiteside4 Analysis of the latest collection of Hospital Episode Statistics data shows that this upward trend continues, with 421 admissions in 2013, increasing to 748 in 2017. Explanations for this upward trend are multifactorial, but may include: an increased awareness of malignant otitis externa, an ageing population, the diabetes epidemic and possible antibiotic resistance.
Nevertheless, there remains no consensus regarding: diagnostic criteria, prognostic indicators or management pathways. This lack of clarity was highlighted in a systematic review, which identified more than 25 malignant otitis externa studies, each with its own set of diagnostic criteria.Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo5 Many existing malignant otitis externa studies involve small retrospective cohorts of patients. Diagnostic criteria are variable; some authors relied on defining individual symptoms, whilst others simply used evidence of otitis externa, possibly including severe otitis externa and thus increasing the false-positive diagnosis rate. Only one study in the review by Mahdyoun et al. included local risk factors as a diagnostic consideration.Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo5
In an attempt to prevent confusion and formulate a standardised treatment pathway, all patients presenting to our unit with suspected malignant otitis externa were reviewed and managed in a multidisciplinary setting (infectious disease, microbiology and neurotology departments) led by a single named ENT consultant. The algorithm pathway was developed to prevent heterogeneity in clinical management and to streamline care, allowing co-ordinated activity between the multiple team members.
Our malignant otitis externa pathway (Figure 3) commences by identifying those patients more at risk of developing potential malignant otitis externa. These included: older immunosuppressed or immunocompromised patients; those with recent exposure to water and/or trauma; and patients with subsequent pseudomonal infection that failed to respond to adequate treatment over a two-week period.Reference Kaushik, Malik and Saeed6
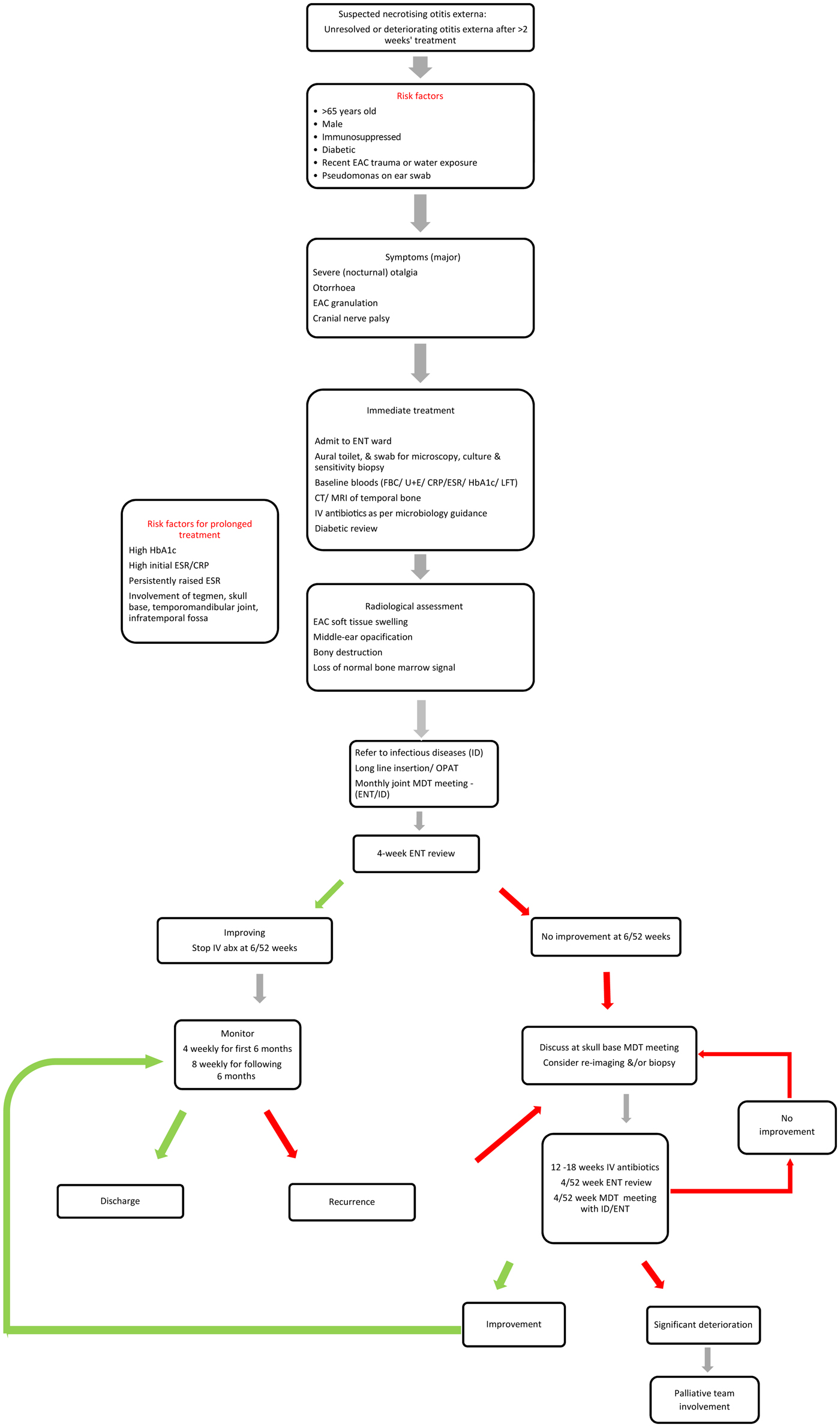
Fig. 3. Malignant otitis externa investigation and treatment pathway. Risk factors and major symptoms are outlined, followed by a standardised investigation and treatment algorithm. EAC = external auditory canal; FBC = full blood count; U + E = urea and electrolytes; CRP = C-reactive protein; ESR = erythrocyte sedimentation rate; HbA1c = haemoglobin A1c; LFT = liver function test; CT = computed tomography; MRI = magnetic resonance imaging; IV = intravenous; OPAT = out-patient parenteral antibiotic therapy; MDT = multidisciplinary team; abx = antibiotics
Unlike other studies, we have not proposed a required minimum number of symptoms for a diagnosis of malignant otitis externa. Major clinical signs and symptoms, as described in our cohort and by other authors,Reference Mahdyoun, Pulcini, Gahide, Raffaelli, Savoldelli and Castillo5,Reference Cohen and Freidman7,Reference Stevens, Lambert, Baker and Meyer8 include: severe unremitting deep-seated otalgia, otorrhoea, and granulation arising from the external auditory meatus. Included in the major signs are lower cranial nerve neuropathies that suggest progression to skull base osteomyelitis. Other symptoms worth considering, although not often reported, include malocclusion and trismus due to soft tissue involvement in the infratemporal fossa and temporomandibular joint, as noted in our cohort (37.5 per cent).
Patients with suspected malignant otitis externa underwent thorough aural microsuction, swabs for both bacterial and fungal culture testing, antibiotic sensitivity testing, and biopsies (to exclude possible malignancy). Thereafter, patients were admitted onto the ward for intravenous antibiotic therapy and in-patient imaging.
Bedside routine testing of blood was conducted; specifically, inflammatory markers (ESR, CRP) and haemoglobin A1c (in diabetics) were analysed to determine if any could be used as a prognostic marker or to ascertain the possible duration of treatment. Pearson coefficient demonstrated a weakly positive (although not statistically significant) correlation between initial ESR and CRP results and prolonged treatment courses (R = 0.4194, p = 0.135, and R = 0.2914, p = 0.27, respectively).
Haemoglobin A1c levels showed a moderately positive correlation (R = 0.7004), which was statistically significant (p = 0.02). These results contradict those of other studies that failed to show any correlation between level of glycaemic control and outcome.Reference Loh and Loh9,Reference Franco-Vidal, Blanchet, Bebear, Dutronc and Darrouzet10 It remains unclear whether the finding of raised haemoglobin A1c could simply reflect, in part, the longstanding untreated chronic infection or poor general diabetic control. There are no reported cases of diabetes mellitus presenting de novo with malignant otitis externa as the first presentation; it would, however, seem sensible to ensure that new malignant otitis externa patients are not undiagnosed diabetics.
Although ESR or CRP were not identified as predictors of outcome or treatment length, serial monitoring demonstrated a progressive downward trend in those who responded quickly to therapy, with a slower decline towards normality in those with extensive skull base disease (three patients never fully returned to normal during the treatment course). It is not yet clear whether ESR or CRP is the more accurate and useful marker; we do, however, recommend observing both whilst monitoring therapy, although we understand that not all UK National Health Service trusts will routinely measure ESR.
At present, all patients presenting to our Trust with suspected malignant otitis externa undergo both CT and MRI unless contraindicated. Computed tomography is often cited in the literature as the first-line investigation. This is because it is readily available and provides clear anatomical visualisation. Furthermore, it may highlight bone erosion, a hallmark for osteomyelitis or other destructive processes. An absence of bone erosion does not preclude osteomyelitis, as bone erosion is only seen on CT once demineralisation has occurred, and this process itself can take several months.Reference Sreepada and Kwartler11
Magnetic resonance imaging has been shown to be superior in detecting bone marrow oedema, which often precedes cortical bone erosion, and thus provides useful complimentary information in the early stages of the disease process. This is highlighted in our results, as only four patients had CT scans demonstrating cortical erosion, but another six patients demonstrated early osteitis with evidence of bone marrow enhancement on MRI (Table 3). Evidence of bone erosion, notably at the temporomandibular joint, infratemporal fossa or tegmen, is cited in numerous studies as being associated with a worse outcome and/or persistent disease.Reference Peleg, Perez, Raveh, Berelowitz and Cohen12–Reference Joshua, Sulkes, Raveh, Bishara and Nageris14 In our own study cohort, patients with these findings had longer average treatment durations (average of 190 days; range, 92–252 days), suggesting more severe disease and indicating that there are possible radiological predictive markers of the need for prolonged therapy.
Nuclear medicine imaging is widely postulated in the literature as being a tool for both diagnosis and clinical follow up of malignant otitis externa. However, because of high cost, limited availability, and low sensitivity and specificity, it is not used routinely. Nuclear medicine imaging may be considered as an adjunct modality, and has been reported as providing useful information with respect to terminating antimicrobial therapy or in those patients where MRI is contraindicated.
Seventy-five per cent of patients in our cohort grew P aeruginosa. Studies have increasingly reported culture-negative malignant otitis externa patients,Reference Carlton, Perez and Smouha15,Reference Djalilian, Shamloo, Thakkar and Najme-Rahim16 which is thought to result from the numerous antimicrobial courses in primary care before referral to an ENT specialist.
The first-line choice of antimicrobial and the treatment duration vary widely in the literature and throughout the UK. An analysis of antimicrobial choice and guidance in UK hospitals, conducted by Pankhania et al., showed that Tazocin is the most frequently suggested first-choice antibiotic for malignant otitis externa (as indicated by 41 per cent of responding institutions).Reference Pankhania, Bashyam, Judd and Jassar2 This treatment was followed by case-by-case discussion with the microbiology department to consider local disease prevalence and sensitivities. Ciprofloxacin was given as a first-line treatment in 26 per cent of responding institutions, according to Pankhania et al.Reference Pankhania, Bashyam, Judd and Jassar2 Several studies have, however, reported cases of pseudomonas that are resistant to fluoroquinolones.Reference Bernstein, Holland, Porter and Maw17–Reference Rubin Grandis, Branstetter and Yu19 Within our own cohort, we identified two patients with confirmed ciprofloxacin resistance.
We do not currently advocate the use of ciprofloxacin alone as a first-line antimicrobial, despite its advantage of being orally administered, hence avoiding protracted hospital stays. Ciprofloxacin, especially when used as a monotherapy agent, enhances the risk of induced resistance, and is associated with an increased risk of clostridium difficile infection within an already frail and vulnerable population. A systematic literature review by Pulcini et al. demonstrated better outcomes with initial combination therapy compared with single therapy (97 vs 83 per cent, p < 0.001).Reference Pulcini, Mahdyoun, Cua, Gahide, Castillo and Guevara20
The majority of our patients (75 per cent) were commenced on Tazocin initially. This allowed for broader initial treatment, with Gram-positive, anaerobic and pseudomonal cover. All patients were discharged home once treatment commenced, completing the parenteral antibiotic treatment in the community, through a peripheral long line, under the supervision of the out-patient parenteral antimicrobial therapy team. Following hospital discharge, our pathway works on a six-week cycle of antimicrobial therapy (Figure 3).
The optimal length of treatment in skull base osteomyelitis is unknown; we have only animal models of chronic osteomyelitis and the experience in treating peripheral bone infections to draw principles. Six-weekly therapy is based on the time needed for bone to re-vascularise, which is reported to require a minimum of three to four weeks in peripheral bones.Reference Courson, Vikram and Barrs21 In contrast, osteomyelitis of long bones is usually treated alongside surgical debridement; this is a considerably different regime to that for osteomyelitis of the skull base, which is now rarely debrided in the UK. Six weeks of intravenous treatment has been cited as sufficient for cure in malignant otitis externa.Reference Pulcini, Mahdyoun, Cua, Gahide, Castillo and Guevara20 The majority of our cohort required longer than six weeks of antimicrobial therapy, which we feel represents more advanced local disease secondary to delayed recognition and referral.
All cases are subsequently discussed at a monthly MDT meeting, alongside the microbiology and infectious disease departments. Changes to treatment would often follow culture results and/or changes in the clinical picture (improving or deteriorating). There remain no universally accepted criteria for determining when to terminate treatment. We therefore use the combination of improving inflammatory markers, and resolving symptoms with a normal external auditory canal on examination, as markers for disease resolution. At this point, antibiotic therapy is stopped.
Recurrence rates with skull base osteomyelitis have been reported to be as high as 20 per cent.Reference Singh, Al Khabori and Hyder22 Given this risk of recurrence, we recommend follow up every four to six weeks for the first six months, and every eight weeks for the next six months.
Failure of improvement after the initial six weeks of antibiotics and/or signs of recurrence prompt a review at the local skull base MDT meeting. The merits of re-imaging and biopsies from deep-seated sites are discussed at this point. Repeat CT and MRI scanning provide only limited information in assessing responses to treatment, given the persistent changes that occur during and after antimicrobial therapy. Al-Noury and Lotfy reported persistent cortical bone changes on repeat temporal bone CT scans conducted at 12 months, whilst MRI bone marrow abnormalities persisted in one-third of patients at 12 months.Reference Al-Noury and Lotfy23 For difficult cases and cases where imaging may be contraindicated, nuclear medicine imaging scans should be considered.
Within our study cohort, three patients required re-admission for worsening symptoms; all underwent further imaging (combination of CT and MRI), with no significant changes reported. Interestingly, in all three patients, the ESR level remained raised but stable at around 20 mm/hour. One patient had a spike in CRP and the other two had normal CRP levels.
• Malignant otitis externa is an aggressive infection of the external auditory canal, with an increasing incidence in the UK
• There remains no agreed consensus regarding diagnosis, investigation or treatment
• An at-risk population does exist: predominately but not exclusively male, elderly, and immunosuppressed or diabetic
• Trauma to the ear canal in an at-risk population appears to be a contributing factor
• A diagnostic and treatment pathway for managing patients with malignant otitis externa is proposed
• This pathway can allow for standardised care and ultimately help identify diagnostic and prognostic markers
Hyperbaric oxygen therapy has been postulated as an adjunct treatment in patients with malignant otitis externa. Currently, there remains a lack of evidence regarding its efficacy in these patients, with a paucity of any randomised control trials.Reference Phillips and Jones24 The low number of hyperbaric centres throughout the country and potential cost implications further limit this option for most UK hospitals. The pathway's main limitation is that it was developed on the basis of our own local patient population; it may not be fully applicable to all patient populations or all patterns of microbial resistance, and is governed by the limited resources of the National Health Service.
Conclusion
Malignant otitis externa appears to be on the increase within the UK and yet it remains a poorly defined clinical entity. A ‘typical’ at-risk population does appear to exist; however, this is by no means exclusive.
The relatively small numbers of malignant otitis externa cases, combined with a lack of diagnostic clarity, continue to hamper the identification of diagnostic and prognostic markers. Because of this, we are unable to draw any strong conclusions from our own study results.
By introducing a local pathway, we aim to standardise and improve care and audit outcomes, to allow future developments.
Through planned education in the primary care setting, we hope that malignant otitis externa patients will be identified and referred for appropriate, earlier treatment. Greater education will also hopefully ensure more caution around aural cleaning (syringing) in high-risk patients, thereby reducing incidences in the first place.
Competing interests
None declared