Introduction
An ectopic thyroid gland is a rare, congenital anomaly of thyroid development which occurs as a result of the failure of thyroid descent from the foramen caecum at the base of the tongue to the prelaryngeal site. Ectopic thyroid tissue can be situated anywhere along the embryonic path of descent, but 90 per cent of cases are found in the tongue, and termed lingual thyroid tissue.Reference Chiu, Su, Hwang, Chien and Eng1 Patients with lingual thyroid tissue usually present with symptoms such as dysphagia, choking, haemorrhage and dyspnoea, and occasionally life-threatening airway obstruction. In addition, malignant transformation of the lingual thyroid has been reported, albeit rarely.Reference Yaday, Singh and Aggarwal2
For patients with obstructive symptoms, thyroxine replacement should be introduced as initial therapy, to induce glandular shrinkage.Reference Mussak and Kacker3 If conservative treatment fails to reduce the size of the nodules, surgery is necessary. In over 70 per cent of patients with symptomatic lingual thyroid tissue, the ectopic glands are their only functional thyroid tissue.Reference Danner, Bodenner and Breau4 In such cases, surgical ablation would necessitate lifelong thyroid hormone replacement, which is unacceptable to most patients. Therefore, transposition of the ectopic thyroid tissue should be considered whenever possible.
In the present report, we describe a case in which the lingual thyroid was transposed from the base of the tongue to the submandibular space via a lateral pharyngotomy approach. This method is relatively safe and simple. The new bed of the transposed thyroid tissue is superficial, facilitating post-operative follow-up examination. The advantages of such treatment for this rare problem are discussed.
Case report
A 52-year-old Chinese woman was admitted to our unit with a mass at the base of her tongue. This had enlarged significantly over the previous two months and now caused dysphagia, dyspnoea and the sensation of a foreign body in her throat.
Physical examination revealed a mass 2.5 cm in diameter in the posterior third of the tongue; part of the lesion could be seen directly when the tongue was pulled forward (Figure 1a and 1b).
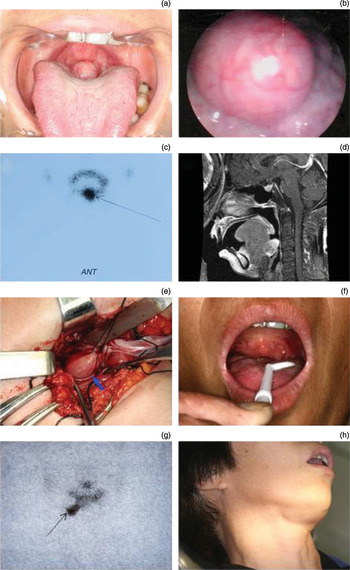
Fig. 1 (a) Clinical photograph showing a round, pink mass located in the centre of the tongue root. (b) Endoscopic view of the ectopic thyroid tissue in the tongue base. (c) Emission computed tomography scan showing concentration of Tc-99m radioactive tracer in the tongue root, with no uptake at the normal thyroid site. (d) Sagittal magnetic resonance imaging scan showed a nodular mass at the base of the tongue. (e) Surgical photograph showing the lingual thyroid (blue arrow), during transposition to the submandibular space. (f) Clinical photograph at 12-month follow up showing absence of recurrence; the patient's symptoms of foreign body sensation and dysphagia were relieved. (g) Technetium-99m scan performed 12 months post-operatively, showing the transposed thyroid gland located in the right side of the neck. (h) Clinical photograph taken 12 months post-operatively, showing barely noticeable scarring on the right side of the neck.
A B-type ultrasonic examination revealed absence of thyroid gland tissue in the pretracheal region. An emission computed tomography (CT) scan showed uptake of Tc-99m by the mass at the lingual base (Figure 1c). Magnetic resonance imaging (MRI) of the neck revealed a nodular mass at the base of the tongue (Figure 1d). These imaging results established the diagnosis of a lingual thyroid.
Thyroid function tests showed elevated levels of thyroid-stimulating hormone (TSH), at 14.7 mIU/l (normal range, 0.4–4.0 mIU/l) and reduced levels of total thyroxine (T4; 52.6 nmol/l; normal range, approximately 58.0–161.0 nmol/l).
Under general anaesthesia, using orotracheal intubation, a 9 cm skin incision was made over the right submandibular region. The subplatysmal region was dissected and the lingual artery and superior thyroid artery identified. No thyroid tissue was found in the anterior neck, after tracing the path of the superior thyroid artery. The submandibular gland was then partially elevated, and its blood supply and duct were protected. The posterior margin of the mylohyoid muscle was displaced to expose the pharyngeal mucosa on the lingual side. A transverse pharyngotomy approximately 4 cm in length was made at the level of the base of the tongue, just above the hyoid bone (Figure 2a). A well circumscribed, submucosal, 2.5 cm diameter mass was clearly identified (Figure 2b).

Fig. 2 Diagrams of the thyroid transposition procedure. (a) The surgical approach: a transverse pharyngotomy designed to enter beneath the right pharyngeal mucosa, with displacement of the submandibular gland and surrounding muscles. (b) Exposition of the lingual thyroid via a right lateral pharyngotomy approach.8 (c) Transfer of the lingual thyroid to the right submandibular space, with a muscle pedicle providing the vascular supply.
The mucosa that encapsulated the gland was removed in its entirety to avoid the formation of any cystic lesion. A frozen biopsy confirmed the presence of normal thyroid gland tissue and the absence of malignant transformation. A section of the left half of the gland was dissected from the tongue base, as the deep part was attached to the musculature of the tongue. Two incisions were made on the surface of the tongue base to prepare the muscle pedicle. The incisions extended from the ectopic gland to the right junction of the tongue and pharynx. The tongue muscle was dissected to form a muscle flap approximately 7 mm in diameter. A broad-based pedicle was formed near the pharyngeal incision, and the gland was dissected so that its right and deep sides remained attached to the pedicle. The mucosa on the muscle pedicle was removed and the wound on the tongue base was closed. The lingual thyroid was transferred through the pharyngeal incision into the right submandibular space (Figure 1e), where it was sited partially intramuscularly (Figure 2c). After complete homeostasis was achieved, the pharyngotomy opening and skin incision were closed layer-to-layer.
The patient was discharged 7 days post-operatively after an uneventful recovery.
Over the following year, the patient's foreign body sensation and dysphagia disappeared, and her breathing normalised (Figure 1f). Follow-up investigations included thyroid function tests (Table I) and Tc-99m and iodine131 scanning (Figure 1g). The levels of tri-iodothyronine and T4 gradually increased, and normalised within the first three to four weeks after surgery. A significant rise in TSH level was noted by the end of the second month, and thereafter TSH remained at a stable but high level for a prolonged period. Technetium 99m scanning showed that the transposed thyroid gland was located in the right side of the neck. The patient was satisfied with the degree of scarring, which was minimal (Fig 1h).
Table I Pre- and post-operative thyroid function

TT4 = total thyroxine; TT3 = total tri-iodothyronine; TSH = thyroid-stimulating hormone; FT4 = free T4; pre-op = pre-operative; post-op = post-operative; wk = week; mth = month
Discussion
Several surgical techniques for the treatment of symptomatic lingual thyroid tissue have been described, including transoral resection, endoscopic CO2 laser resection,Reference Minuto, Fazzuoli, Rollandi, Derchi and Biassoni6 auto-transplantationReference Wu, Zheng, Dong, Li, Zhang and Zhao7 and pedicle transposition.Reference Puxeddu, Pelagatti and Nicolai5, Reference Rojananin and Ungkanont8 In recent years, pedicle-based techniques have been confirmed to have adequate vascularity, and their use has been frequently reported.
Ectopic thyroid tissue in the tongue base can be approached surgically by a variety of methods.
The lip-split mandibulotomy technique has been a successful access procedure for lesions in the base of the tongue; however, the facial scar produced is the main disadvantage, and may not be accepted by every patient. Mandibular osteotomy causes additional trauma and tongue oedema, which may result in varying degrees of dysphagia.Reference Devine, Rogers, McNally, Brown and Vaughan9
• We report a modified technique for transposing an ectopic, tongue-root thyroid to the submandibular space
• Lateral pharyngotomy enabled adequate exposure of the lingual thyroid
• A random muscle pedicle provided the vascular supply
• Thyroid function was preserved
• This procedure is a promising treatment for the lingual thyroid
The transverse lateral pharyngotomy approach offers adequate exposure to ectopic thyroid glands in the root of the tongue, especially for large masses. Good visualisation can decrease the risk of cranial nerve injury and facilitate effective haemostasis. Avoidance of a segmental mandibular resection or mandibulotomy prevents malocclusion, masticatory dysfunction, temporomandibular joint pain and difficulty with the oral phase of swallowing.Reference Righi, Bade, Coleman and Allen10 The risk of creating a pharyngocutaneous fistula can be decreased by reconstruction with well vascularised tissue harvested from outside the zone of tissue injury.Reference Duvvuri and Myers11 The main disadvantage of this approach is the potential for a poor cosmetic outcome as a result of the scar on the lateral neck. However, this area is likely to heal well without significant tension. Also, scars on the lower lip and mental area are avoided. In the presented case, the patient was satisfied with the cosmetic outcome.
The lingual artery supplies blood to the tongue in an ‘umbrella’ fashion. In the presented case, during transposition of the thyroid gland, no obvious artery or vein was identified below the thyroid tissue, and so the gland was not transposed as a vascularised pedicle. Therefore, a random muscle pedicle flap was created at the distal end of the gland in order to furnish a blood supply, enabling the survival of the transposed thyroid.
After surgical procedures involving transposition of thyroid tissue, a hypertrophic increase in gland volume can occur; this may develop independently of TSH hypersecretion.Reference Berglund, Aspelin, Bondeson, Bondeson, Christensen and Ekberg12 Although it is possible to transpose a lingual thyroid to a position beneath the mucosa of the lateral pharynx, this could create a long-term risk of swelling into the pharyngeal cavity. In additional, it would be difficult to evaluate the newly sited thyroid gland for malignant transformation, if it was transferred to a deep position. In the presented case, the submandibular space was chosen as the new site for a lingual thyroid. As a result, the transferred thyroid tissue could be directly palpated in order to assess for hypertrophy or nodule formation, and any abnormalities promptly detected. A biopsy could also be easily performed, if necessary, to detect malignant transformation.
Conclusion
We present a promising technique for the transplantation of lingual thyroid tissue. The lateral pharyngotomy approach benefits from a shorter distance of tissue transfer and less surgical trauma, compared with other techniques. The submandibular space is an ideal recipient bed as it is close to the normal thyroid site, has a good blood supply, and is convenient for post-operative examination. The presented case demonstrated normal post-operative thyroid function and a satisfying cosmetic outcome.
Acknowledgements
This work is supported in part by the National Natural Science Foundation of China (No. 81001213).





