During an emergency, public health responders perform duties to protect the health and safety of affected individuals. The type of emergency that public health responders could be deployed to includes natural disasters (eg, hurricanes, floods, and fires), human-induced/technological disasters (eg, chemical spills), infectious disease outbreaks (eg, influenza, Zika, and Ebola virus disease), and other mass casualty events. 1 In response to natural disasters, public health responders support shelters, perform immunizations, conduct infectious disease surveillance and outbreak investigations at shelters and in the community, assess environmental exposures, and perform food safety inspections and other public health or emergency response duties as needed. Although public health responders can include staff from several government agencies,Reference Werner, Wright and Thomas 2 for the disaster response reported in this paper, public health responders were personnel from state and local health departments in Georgia and include epidemiologists, nurses, doctors, emergency medical services (EMS) personnel, environmental health specialists, emergency managers, laboratory personnel, and other public health professionals. While performing response work, public health responders may become injured or exposed to harmful environmental conditions or chemical or biological agents that could adversely impact their physical and/or psychological health.Reference Weinhold 3 , Reference Benedek, Fullerton and Ursano 4 The Georgia Department of Public Health (DPH) monitors the health and safety of public health responders during a disaster response and ensures that responders receive appropriate medical care following an injury or exposure.
On October 7, 2016, Hurricane Matthew traveled along the coasts of Florida, Georgia, and South Carolina causing high winds, flooding, and power outages. 5 , 6 In anticipation of the storm, coastal residents were evacuated, and congregate shelters were opened around the state. Public health responders from state and local health departments in Georgia were deployed to assist with response efforts in general population and functional needs shelters.
DPH did not have a centralized monitoring system or information database to systematically and efficiently track the health and safety of deployed public health responders. In response to a public health emergency, prior to Hurricane Matthew, state and local health departments would deploy their staff as needed, and monitoring of responders’ deployment roles, injuries, and exposures varied by health department.
As a result, epidemiologists along with information technology (IT) specialists at DPH rapidly developed the Web-based Responder Safety, Tracking, and Resilience (R-STaR) system as a module within our existing State Electronic Notifiable Disease Surveillance System (SendSS). R-STaR development began on October 6, 2016, and was implemented in 24 hours. R-STaR is a centralized Web-based system for rostering public health responders, tracking their deployment activities, and monitoring their health during and after deployment.
R-STaR development and content were based on the framework outlined by the Emergency Responder Health Monitoring and Surveillance System (ERHMS) developed by a consortium of 15 federal agencies, including the Centers for Disease Control and Prevention and the Federal Emergency Management Agency. The ERHMS framework provides recommendations for monitoring the health of responders during the pre-deployment, deployment, and post-deployment phases (Figure 1). 7 Given limited time and resources, DPH developed R-STaR functions and content based on the ERHMS recommendations that were the most critical to responder health monitoring during the deployment and post-deployment phases and could be quickly implemented. The ERHMS functions (see Figure 1) implemented using R-STaR during the pre-deployment phase included rostering and database management/information security. The ERHMS functions implemented using R-STaR during the deployment phase included health monitoring and surveillance, activities documentation, and communication of health monitoring and surveillance data. During post-deployment, as recommended by ERHMS, R-STaR was used for responder out-processing to assess the extent to which responders were adversely affected by their work during deployment. By incorporating these recommended ERHMS functions, we aimed to use R-STaR for the timely identification of responder exposures and symptoms and referral for medical attention to prevent or mitigate adverse health outcomes. Additionally, R-STaR was designed to inform the development of pre-event responder training and to improve disaster preparedness and response planning for future disasters.
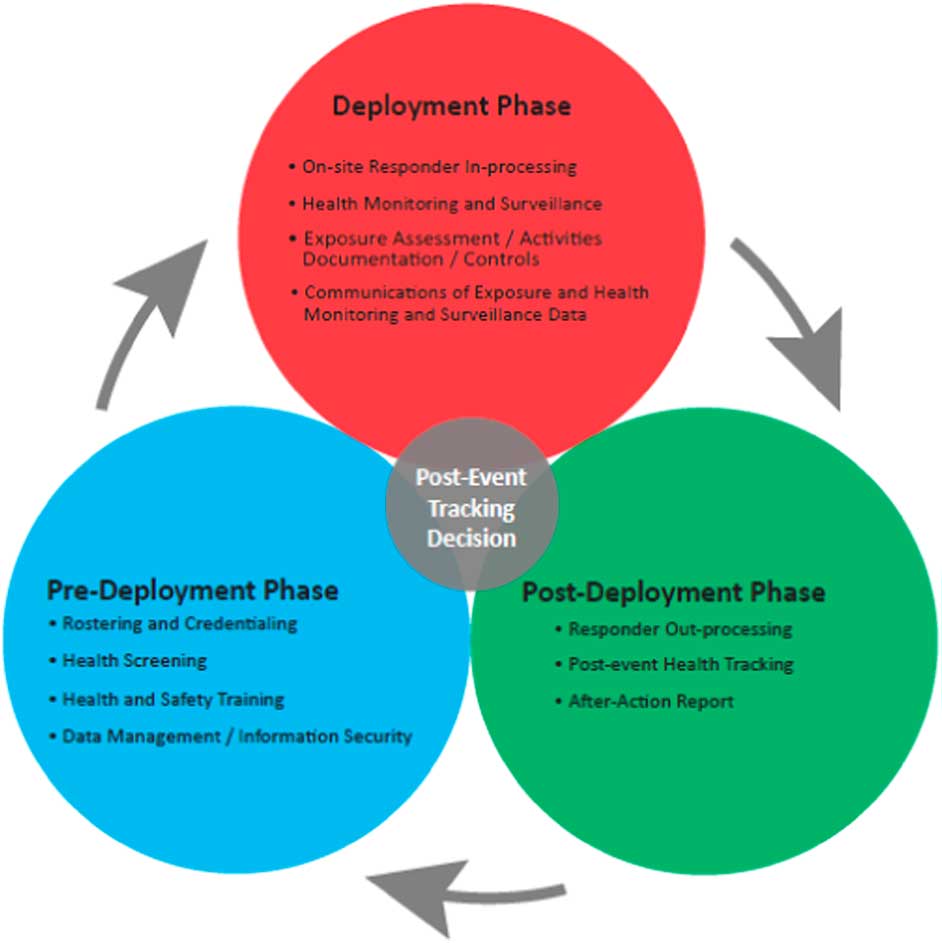
Figure 1 The Emergency Responder Health Monitoring and Surveillance System (ERHMS) Framework for Each Emergency Response Phase.
In this paper, we describe the development of R-STaR and analyze data collected using R-STaR to report on the health and safety of responders during the Hurricane Matthew response and user satisfaction with R-STaR. Last, we provide recommendations to improve R-STaR, responder training, disaster response planning, and responder health monitoring and surveillance in Georgia and at other state and local health departments and disaster response agencies.
METHODS
Informatics Development
DPH epidemiologists collaborated with IT specialists to rapidly develop the R-STaR monitoring system. The system was developed within SendSS, Georgia’s Web-based system for notifiable disease reporting. SendSS uses a Web-based application run on an Oracle database that allows for controlled privileges, secure storage of confidential information, creation of Web-based surveys and databases, and customizable interface and content. 8 Three surveys were developed in R-STaR to collect data from responders: a registration survey, a daily health and safety survey, and a post-deployment survey. Surveys were securely accessed by responders, using automatically generated links that were e-mailed to users using R-STaR. Responses for each survey were linked and stored in each responder’s R-STaR account. Because each responder’s R-STaR account is housed in SendSS, responder health information was protected using the Health Insurance Portability and Accountability Act compliant security and privacy features. Only the three epidemiologists who monitored responders had access to responders’ account information and data.
The back end of R-STaR, accessed by epidemiologists who were monitoring responders, had a dashboard view of deployment status, injuries, and harmful exposures reported by all responders (Figure 2). If a responder reported an injury or harmful exposure, an epidemiologist contacted the responder to assess the need for medical care.

Figure 2 Example of R-STaR Dashboard.
R-STaR Registration
R-STaR was used to roster responders and determine whether responders were prepared to deploy. The registration process took less than 2 minutes to complete and could be completed before or during deployment. The R-STaR registration process created an R-STaR account for each responder that could be accessed and updated as necessary by responders during or after deployment. Responders registered for R-STaR using a secure registration link to a Web-based survey (ie, registration page) that collected information on work location and department/program. The registration page also included questions on responder readiness to deploy, and asked (1) Are your immunizations up to date? (2) Can you bring a 2-week supply of needed medications? and (3) Have you received just-in-time training? Question response choices were yes or no. Just-in-time training of responders informs responders of the scope of the emergency, their duties, and how to protect themselves from injury and/or exposures during deployment. The registration link was sent via e-mail by DPH department leads for Nursing, Epidemiology, Environmental Health, and other programs at the DPH Emergency Operations Center, the centralized location for the coordination of public health resources and partners for the Hurricane Matthew response. Supervisors at state, local, and district health departments then e-mailed the registration link to their deployed or deploying staff.
Deployed Responder Monitoring
Once deployed, registered responders received a daily e-mail with a secure link to a Web-based health and safety survey in R-STaR asking about their current deployment status (ie, ready to deploy, deployed, no longer deployed), deployment county and address, duties, shift duration (in hours), and any exposures or injuries experienced during response activities (yes or no). Responders were asked to record injuries or exposures using an open-ended field. The daily health and safety survey had 10 items, took less than 1 minute to complete, and responses were monitored by DPH epidemiologists. Responders were asked to complete the health and safety survey daily, and each day was recorded as a separate entry in R-STaR. Responders could also complete the health and safety survey retrospectively.
DPH epidemiologists monitored responder data using a data visualization dashboard in R-STaR, which listed deployment status and reports of injuries or exposures for all responders (see Figure 2) and by viewing individual responder records, which displayed a chronological history of daily health and safety survey responses. These features allowed 3 epidemiologists to monitor responses for more than 100 responders, to quickly contact responders reporting injury or exposure, to assess whether medical evaluation or treatment was needed, and to detect infectious disease outbreaks and other work-related health risks among responders needing further investigation.
Post-Deployment Health and Experience Survey
After deployment, responders received a 9-question survey about their deployment experience, including barriers to health and safety and post-deployment stress responses. Disaster work can lead to mild distress responses, such as sleep disturbance, or more severe stress disorders like posttraumatic stress disorder that require clinical treatment.Reference Benedek, Fullerton and Ursano 4 Self-care (eg, getting sufficient sleep, work breaks, food, and water) can help reduce stress and prevent or mitigate distress responses and mental disorders associated with response work.Reference Benedek, Fullerton and Ursano 4 , 9 The post-deployment survey was sent to responders 3 weeks after the end of response efforts. The survey questions included (1) Who is your employer/department? (open-ended) (2) What were your deployment roles and duties? (open-ended) (3) Did you receive just-in-time training and feel prepared for your deployment role? (yes, somewhat, or no) (4) Did you feel safe while deployed? (yes, somewhat, or no) (5) Did you have the supplies and equipment needed for your deployment? (yes, somewhat, or no) (6) Were you and your family prepared for the disruption in your routine caused by your deployment? (yes, somewhat, or no) (7) Did you engage in self-care activities during your deployment (eg, getting enough rest and staying hydrated)? (yes, somewhat, or no) (8) What were your barriers to self-care? (open-ended) and (9) Did you experience lingering signs or stress after deployment such as unpleasant memories of your experience, changes in sleep patterns/appetite, and trouble concentrating? (yes, somewhat, or no). Closed-ended questions included an additional open-ended field that allowed responders to provide additional information for each question.
R-STaR Evaluation
The post-deployment survey also included questions to evaluate responders’ satisfaction with using R-STaR to report on their health during deployment. Responders were asked (1) Was the responder safety survey easy to use? (2) Did you like having your deployment activities tracked? and to (3) Describe strengths and weakness of the system and how it can be improved (open-ended). Response choices for the first 2 questions were yes, somewhat, and no and included an open-ended comments field that allowed responders to provide additional feedback.
Data Analysis
Frequency tabulations were completed for each question of each survey. Quantitative data were recoded into binary response variables (ie, yes or no) by recoding the somewhat response as yes. For each question, missing values were excluded from the analysis, and percentages were calculated using the total non-missing responses as the denominator. For open-ended questions, qualitative data were analyzed and summarized into key themes and emergent content patterns.
For the post-deployment health and experience survey, qualitative data from the comments fields were analyzed for questions that were identified as problem areas based upon quantitative data or provided insight into how R-STaR and responder health and safety could be improved. For the R-STaR evaluation, qualitative data from the open-ended question and the comments field for each question were combined. This activity did not undergo institutional review board (IRB) approval because it was public health practice, not research involving human subjects.
RESULTS
R-STaR Registration
One hundred and twenty-six public health responders, representing 11 health districts and more than 30 counties in Georgia, registered in R-STaR during the Hurricane Matthew deployment. Responders included 61% (n=77) from Nursing; 13% (n=16) from Environmental Health; 6% (n=7) from Emergency Preparedness and Response; 4% (n=5) from Epidemiology; 2% (n=3) from Immunizations; 0.8% (n=1) from EMS; and 13.5% (n=17) from other departments or programs, including Finance; IT; Administrative; and Women, Infants, and Children (WIC). During registration, 100% of responders reported immunizations being current, and 95% reported being able to bring needed medications during deployment. Prior to deployment, 56% reported receiving just-in-time training.
Responder Health and Duties During Deployment
Public health responders assisted with the sheltering of an estimated 37,000 evacuees at 50 shelters by performing shelter inspections, providing nursing assistance, and conducting infectious disease surveillance at shelters. All shelters were managed by non-profit organizations, and 38 (76%) were managed by the American Red Cross. These organizations did not provide public health or clinical personnel for the shelters. As a result, public health responders assisted with sheltering in collaboration with the managing organization. Public health responders also helped coordinate placement of patients displaced from health care settings, evacuate vulnerable populations, and perform environmental inspections. Each responder was deployed between 12 and 72 hours.
Nurses reported providing clinical support at shelters such as giving general first aid, checking vital signs, administering health assessments, and providing appropriate treatment to evacuees. Epidemiology staff reported implementing infectious disease surveillance in shelters. Environmental Health staff performed food inspections at shelters and restaurants impacted by the storm. Staff from Immunizations, WIC, and other programs provided staffing support to shelters, including performing intake and discharge of evacuees.
Six (4.8%) responders reported exposures during deployment. Exposures were all among nurses who were exposed to blood or body fluids while providing medical care to evacuees at shelters. All were contacted by an epidemiologist and none needed additional medical treatment or follow-up. No injuries were reported.
Post-Deployment Health and Experience Survey
Forty-two percent of responders (n=53) completed the post-deployment survey. In response to the post-deployment survey, 64% (n=33) of responders reported receiving just-in-time training and feeling prepared for their deployment role. Using the open-ended comments field, 21 responders provided additional feedback on just-in-time training. Although responders received little or no training on duties specific to their deployment, 1 responder commented that this had not interfered with their ability to perform assigned duties. Responders who assisted with sheltering described the shelters as busy and chaotic with a lack of clear communication on how to care for evacuees or what forms needed to be completed. Responders mentioned having had prior training in Incident Command System (ICS), National Incident Management Systems, or disaster nursing, but indicated that additional training was needed.
Ninety-two percent (n=47) reported feeling safe while deployed, and 81% (n=43) had supplies and equipment needed for deployment. Responders who felt unsafe reported the reasons being inadequate security at their shelter, the absence of visible badges or identification to distinguish evacuees from shelter staff, and the presence of mentally ill and criminal evacuees (eg, known sex offenders). Responders who had inadequate supplies reported delays in receipt of medical supplies and/or expired medical supplies.
Ninety-two percent (n=49) indicated their family was prepared for the disruption in their routine caused by their deployment, 89% (n=47) engaged in self-care activities during deployment, and 11% (n=6) had lingering signs or stress after deployment. Self-care challenges reported were related to shelter work and included not getting enough sleep due to working night shifts or staff shortages; working long shifts or not getting sufficient breaks due to staff shortages; lack of available food on-site for staff; not enough bathroom facilities and/or existing bathroom facilities poorly maintained and dirty; and inadequate housing accommodations for staff, which, at times, included no hot water for showers.
Post-Deployment R-STaR Evaluation
Eight-one percent (n=43) of responders who completed the post-deployment survey found R-STaR easy to use, and 70% (n=37) indicated that they liked being monitored. Twenty-two responders provided additional feedback on the strengths and weaknesses of R-STaR. Responders noted that R-STaR was easy to use and functional. Responders also liked the accountability that R-STaR provided and the space provided for comments. Responders reported a limitation of R-STaR as being difficulty accessing surveys on a smartphone or desktop due to limited or no Internet access at shelters. As a result, some responders were unable to complete the health and safety survey daily. Responders suggested making the daily health and safety survey available through text messaging to allow submission regardless of Internet connectivity. Other responder recommendations included conducting pre-event training of responders on R-STaR, registering responders before deployment, and enhancing the clarity of R-STaR survey questions and registration instructions.
DISCUSSION
In response to Hurricane Matthew, DPH rapidly developed R-STaR to monitor the health and safety of responders. The Web-based application was easy to use, well received by responders, and provided valuable information on responder health during and after deployment. Our results highlight the benefits of using a user-friendly, Web-based monitoring system, as well as ways to improve R-STaR, responder training, and disaster preparedness planning to more effectively monitor and protect responder health and safety.
R-STaR was rapidly developed in response to an impending hurricane, and a more robust system with improved content and functionality is currently in development. Event-specific survey templates and questions that reflect varying responder health risks will be developed to make the improved R-STaR customizable for a variety of events or emergencies (eg, hurricanes, fires, and infectious disease outbreaks). As a result, when an emergency arises in which responders will be deployed, R-STaR administrators will be able to quickly create an event in R-STaR using event-specific survey templates to begin registering and monitoring responders. R-STaR functionality will be improved to allow each R-STaR account to store survey responses from each deployment, which will enhance long-term responder health monitoring. Additionally, when a responder reports an injury or exposure, an automated alert feature will be added to R-STaR so that the system will automatically e-mail the monitoring epidemiologists to ensure timely follow-up with responders and identification of ongoing responder health hazards. The R-STaR registration process will also be improved to allow supervisors to register responders if responders are unable to self-register. Additionally, a Web application is being developed to make R-STaR available on a smartphone or tablet.
As highlighted by the evaluation, existing survey questions and response choices will be revised to improve clarity and data interpretation. Questions will be added to assess stress responses both during and after deployment and to detect deployment-related injuries or symptoms that may have developed post-deployment. The daily health and safety survey that responders complete during deployment will be expanded to include an itemized list of possible symptoms, injuries, and exposures such as heat stress; sprains; lacerations; gastrointestinal, respiratory, and dermatologic symptoms; and chemical exposure. Monitoring protocols will be expanded to ensure that responders reporting stress symptoms are contacted and, if needed, provided mental health resources. To facilitate more comprehensive credentialing of responders, registration questions will be added to R-STaR to document education, licensing, capabilities and skills, professional training (eg, in cardiopulmonary resuscitation or use of personal protective equipment), and respiratory fit testing.
Implications for Disaster Response Planning and Training
Not all responders reported receiving just-in-time training, which can be critical to responders’ ability to safely and effectively perform their deployment duties.Reference Burke, Sarpy and Smith-Crowe 10 Depending on the nature and changing dynamic of an incident, just-in-time training prior to deployment is not always feasible. Because hurricanes and other natural disasters that require sheltering occur infrequently in Georgia, public health responders in Georgia may not have shelter training or experience. Given that most responders who worked on the sheltering effort were nurses, responders may benefit from pre-event training on disaster nursing, ICS, and/or shelter management in anticipation of future emergencies that require sheltering. Materials are currently being developed by DPH for multiple disciplines that incorporate responder recommendations to improve planning, response, and recovery for events that require sheltering.
Although most responders reported engaging in self-care while deployed, responders reported experiencing significant barriers to self-care, which included insufficient sleep, unavailable food, and staff shortages. Shelters were operated and managed by the American Red Cross and other non-profit organizations. As a result, shelter volunteers from DPH and other local health departments were not always responsible for the logistics, supplies, staffing, and staff accommodations at a shelter. However, DPH can help prevent staff shortages that provide barriers to self-care by credentialing responders using R-STaR before an emergency. The credentialing process will help track all personnel who are skilled and available to deploy, making it easier to fill staff needs during an emergency. Credentialing also facilitates the creation of a roster of responders by capability, which aids with deployment assignment and health monitoring. R-STaR will be available to a wide range of public health agencies in Georgia for rostering and credentialing of their staff prior to emergency deployment. During an emergency, agencies can choose to monitor their own deployed staff or delegate monitoring to district or state epidemiologists. R-STaR is already being used during local and state-wide disaster preparedness exercises.
Limitations
Not all Hurricane Matthew responders were represented by these data. Several federal, state, and local government agencies and non-government organizations were involved in the response. However, our data represented deployed staff employed only by a state or local health department in Georgia who registered for the response in R-STaR. Due to the rapid just-in-time development of R-STaR, there was no training on how to use the system prior to the hurricane. Supervisors at state, local, and district health departments were asked to forward the registration instructions to their staff, and some responders may not have received notification to register or they chose not to register. Additionally, due to the time and resource restraints, some staff were not able to complete the health and safety survey every day. The open-ended questions for the post-deployment survey were developed to detect barriers to responder health and safety, and, as a result, qualitative data focused on challenges faced during deployment and may not reflect other positive aspects of responders’ deployment experience. For simplification of results reporting, “somewhat” responses were reported as “yes,” which may have added bias. Another limitation was that response rates varied for each survey question and between surveys, and the post-deployment survey had a low response rate. However, non-response bias is likely negligible because we sampled a very specific population of public health responders, and there are not likely to be appreciable differences between respondents and non-respondents.
CONCLUSIONS
Responder health monitoring and surveillance are important, yet often overlooked, aspects of any disaster or emergency response. The improvements planned for R-STaR will improve Georgia’s disaster response planning and emergency preparedness capability to monitor and protect the health and safety of responders before, during, and after an event. Beyond Georgia, lessons learned from the development and evaluation of R-STaR can be used to guide the development or improvement of responder health surveillance systems at other state and local health departments and disaster or emergency response agencies across the country.
An important feature of R-STaR and any responder health surveillance system is that the system is flexible and scalable and can be used to track any number and type of personnel for any size or type of event. Another key feature is that the system requires few resources to maintain and allows a small team to track the health of any number of responders. The evaluation of R-STaR highlighted the need for responder health surveillance systems to ensure health surveys are accessible in the field through Web-based technology or applications, to assess both physical and psychological health both during and after deployment, and to facilitate real-time monitoring of responders through automatic e-mail or text notifications when symptoms or injury is reported by a responder.
Although not reported on here, responder health surveillance systems like R-STaR can aid disaster response operations in many ways, in addition to monitoring responder health. Responder health surveillance systems can be used to roster and credential responders prior to an event, quantify the human resources deployed during a declared emergency, distribute responder resources post-deployment, and gather information for after-action reports. As a result, responder health surveillance systems can be a worthwhile investment for state or local health departments and disaster response agencies that can help protect the health of their responders and improve the administrative aspects of disaster response operations and recovery.
Acknowledgments
The authors would like to thank our partners in Epidemiology, Emergency Preparedness and Response, Information Technology, and the Office of EMS at DPH and state and county emergency preparedness directors. We would also like to thank the staff who assisted with registering responders and the responders who provided feedback on their experiences.
Conflict of Interest Statement
The authors declare no conflicts of interest. This activity did not undergo IRB approval because it was public health practice and not research involving human subjects. The conclusions, findings, and opinions expressed by authors in this article do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions. Use of trade names is for identification only and does not imply endorsement by the Public Health Service or by the U.S. Department of Health and Human Services.
Funding
This work was supported by the Public Health Emergency Preparedness Cooperative Agreement from the U.S. Department of Health and Human Services/Centers for Disease Control and Prevention.




