Hurricane Katrina highlighted both the crucial role of first responders in times of disaster and the resultant stress on them and their families. During and after the hurricane, first responders, including police officers, firefighters, emergency medical services personnel, and city workers, were required to meet the challenges to the community of maintaining safety, rescuing and saving lives, and helping to evacuate people with special needs. They were required to work under extremely difficult circumstances because of the flooding and resulting chaos, including an almost total lack of capacity for communication. With the many abandoned houses and neighborhoods, the new culture and mix of violence in the city, and the broken criminal justice system,Reference Garrett and Tetlow1Reference Deflem and Sutphin2 first responders' responsibilities have changed and have been challenged. First responders must continue to do the best that they can to protect the public and fight crime under extremely trying circumstances.Reference Kronenberg, Osofsky, Osofsky, Many, Hardy and Arey3
Studies have documented resilience, expectable stress responses, immediate needs, and longer-term reactions and behavioral health difficulties in the general population after hurricanes and floods.Reference Fernando and Hebert4Reference Mason, Andrews and Upton5Reference Kessler, Galea, Gruber, Sampson, Ursano and Wessely6 Level of symptomatology is associated with the presence of physical injury, fear of death, and property loss.Reference Assanangkornchai, Tangboonngam and Edwards7Reference Briere and Elliott8 Increased symptoms are associated with degree of personal and economic loss, proximity to the event, displacement, a lessened sense of self-efficacy, psychosocial resource loss, feelings of being out of control, lack of knowledge about coping with the crisis, and a relative lack of family and community support.Reference Zwiebach, Rhodes and Roemer9Reference Norris, Murphy, Baker and Perilla10Reference Wadsworth, Santiago and Einhorn11Reference Cieslak, Benight and Schmidt12Reference Smith and Freedy13Reference Glass, Flory, Hankin, Kloos and Turecki14 Previous exposure to trauma predicts increased symptoms after a hurricane.Reference Smith and Freedy13Reference Sutker, Corrigan, Sundgaard-Riise, Uddo and Allain15 Living in shelters and under stress for an extended period of time further predicts increased emotional difficulties.Reference Gittelman16 Posttraumatic stress disorder (PTSD), major depressive disorder, and symptoms that are consistent with both disorders are prevalent sequelae after hurricanes and floods.Reference Kessler, Galea, Gruber, Sampson, Ursano and Wessely6Reference Norris, Murphy, Baker and Perilla10Reference North, Kawasaki, Spitznagel and Hong17 Common symptoms of anxiety, sadness, numbness, anger, disorientation, grief, and overwhelming loss of control also are evident.Reference Shelby and Tredinnick18
Research on first responders has documented specific symptoms observed after disasters. Hypervigilance, social isolation, sadness, irritability, anxiety, poor concentration, and sleep difficulties have been reported.Reference Dowling, Moynihan, Genet and Lewis19 For first responders, the effects of the trauma, including possible injury to self, caused by the disasterReference Perrin, DiGrande, Wheeler, Thorpe, Farfel and Brackbill20 are compounded by prior trauma exposure and vicarious traumatization related to constant exposure to traumatic events. First responders are faced with personal pressures related to separation from their families, worry about their safety and well-being, and personal loss.21Reference Gersons, Carlier, Lamberts and van der Kolk22Reference Carlier, Lamberts and Gersons23Reference Osofsky, Holloway and Pickett24Reference Weiss, Marmar, Metzler and Ronfeldt25 Protective factors contributing to resilience for first responders include perceived self-efficacy, individual personality, organizational preparation and structure, loyalty to colleagues and work, social support, a sense of meaning and hope related to their work, and spirituality.Reference Weiss, Marmar, Metzler and Ronfeldt25Reference Bartone, Ursano, Wright and Ingraham26Reference Benight and Bandura27Reference Crawford, O’Dougherty Wright and Masten28Reference Ursano, Fullerton and Norwood29Reference Luthar30Reference Masten31
Events such as the Oklahoma City bombing, the terrorist activities of September 11, 2001, and Hurricane Katrina brought the nation's attention to the heroic deeds of first responders. Concurrently, mental health professionals are aware of the psychological toll that first responders endure and researchers have increasingly studied mental health issues in first responders. Benedek et alReference Benedek, Fullerton, Ursano and Ursano32 published a literature review that highlights several critical issues related to mental health consequences of disaster on first responders. The authors focused on the long-term psychological sequelae of disasters, citing that increased psychological distress in first responders has been found years and even decades after a disaster. Furthermore, they highlight the multiple layers of disaster- and nondisaster-related traumas, both work related and personal, that first responders face, focusing on how these complexities may affect the long-term psychological well-being of first responders.Reference Benedek, Fullerton, Ursano and Ursano32 First responders working in the metropolitan New Orleans area during and after Hurricane Katrina are a prime example of a group that has been affected by immediate, chronic, and professional and personal traumas and stressors.
The primary objective of this study was to describe the effects of Hurricane Katrina on first responders in the New Orleans area in the 2 years after the devastation and present findings on mental health status and symptoms. We further hypothesized that given the extent of the disaster and slowness of recovery, symptoms of PTSD and depression will not change over time. This information is targeted to guide mental health services for first responders facing future natural and technological disasters.
METHODS
Participants
A total of 1382 first responders voluntarily and anonymously participated in this study, which was conducted at 2 time periods. The first screening was done between 6 and 9 months after Hurricane Katrina (time 1). Eight hundred forty first responders (269 police officers, 374 firefighters, 64 emergency medical services (EMS) personnel, 133 city workers) completed the survey at this time. The majority of the participants were men (79%) whose ages ranged from 21 to 73 years, with a mean age of 39.85 (standard deviation 10.38). The second screening was conducted after the first anniversary of the disaster, 13 to 18 months after the hurricane (time 2). At this time, 638 first responders (321 police officers, 288 firefighters, and 29 EMS personnel) completed the survey. The majority of participants were men (82%) whose ages ranged from 19 to 63 years, with a mean age of 39.58 (standard deviation 9.50).
Sampling
All of the members of the New Orleans Police Department, the New Orleans Fire Department, the Orleans Parish EMS, and the St Bernard Fire Department, and New Orleans and St Bernard Parish city employees, including health department and water board personnel, who were directly involved in the response to Hurricane Katrina qualified for the study. The first responders were surveyed based on their availability at roll calls and at other scheduled times for study completion. Permission from the parish, police district, fire department, and EMS was obtained before administration of the survey. The purpose of the study was explained to potential participants and participation was voluntary. Six of the 8 Orleans Parish police districts, including those most heavily affected by the hurricane, agreed to participate, and the New Orleans Fire Department, Orleans Parish EMS, and St Bernard Fire Department granted full access to department members for the study. Once the survey was completed, each participant was provided an opportunity to speak privately with a clinician and was given a list of referrals for clinical services. A subsample of the total respondents, 87 (6%), voluntarily completed the survey confidentially instead of anonymously to track changes over time. Study protocol was reviewed and approved by the Louisiana State University Health Sciences Center institutional review board.
Instrument
The survey used was adapted from one used by the Centers for Disease Control and Prevention after the 2001 attacks on the World Trade Center and with firefighters and police officers after Hurricane Katrina.3334 Items were selected based on relevance for mental health purposes and items related to alcohol use and partner conflict were added. The survey consisted of questions regarding traumatic experiences, alcohol use, partner conflict, requests for services, PTSD, and depression. To assess traumatic experiences and request for services, yes/no responses were collected in the following areas: concern for family safety during the hurricane; witnessed injury or death; damage to home; injury or death of a friend; injury or death of family; personal serious injury; previous loss or trauma; and participation in mental health services. To measure alcohol use, participants responded to questions regarding their frequency and amount of drinking before the hurricane and at the time of the survey. Based on this information, a single variable, increase in alcohol consumption, was created signifying an increase in frequency of consumption, amount of consumption, or both. Partner conflict was rated on a 10-point scale before the hurricane and at the time of the survey. Based on this information, an increase in partner conflict variable was created.
A trauma measure, the PTSD Checklist Civilian Version (PCL-C), was created by Weathers et alReference Weathers, Huska and Keane35 at the Boston National Center for PTSD-Behavioral Sciences Division. The PCL-C includes 17 items that respondents rated on a 5-point Likert-type scale ranging from 1 (not at all) to 5 (extremely). The PTSD severity cutoff score of 50 was employed.Reference Weathers, Huska and Keane35 The PCL-C also produces subscale scores, which correspond to the PTSD symptoms of reexperiencing (5 items), hyperarousal (7 items), and avoidance (5 items). Symptoms rated as “moderately” or above (item scores of ≥3) are counted as present and total subscale scores correspond to the above number of items. Cutoff scores for each subscale and a total PTSD symptom pattern are consistent with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, endorsement of 1 reexperiencing item, 3 avoidance items, and 2 hyperarousal items.36 The depression measure, the Center for Epidemiologic Studies Depression Scale-Short Form (CESD-SF),Reference Weathers, Litz, Herman, Huska and Keane37 contains 10 questions and uses a 4-point Likert-type scale ranging from 0 (rarely or none of the time; <1 day during the past week) to 3 (most of the time; 5–7 days during the past week). Scores of ≥10 indicates symptoms of depression. The PCL-C and CESD have been used after disasters and are well-validated instruments.3334Reference Weathers, Huska and Keane3536Reference Weathers, Litz, Herman, Huska and Keane37Reference Roberts and Vernon38Reference Brackbill, Thorpe and DiGrande39Reference Andresen, Malmgren, Carter and Patrick40
Statistical Analysis
To address the goal of the present study—to describe the effects of Hurricane Katrina on first responders in the New Orleans area—descriptive statistics were conducted on the total sample (N = 1382). To test the research hypothesis—symptoms of PTSD and depression remained high over time—symptom scores from time 1 and time 2 were compared. McNemar χ2 tests were conducted, using the subsample of matched participants (n = 87) to assess whether percentages of respondents meeting the cutoff criteria suggesting high symptomotology of PTSD (PCL-C) and depression (CESD) at time 1 was statistically significantly different at time 2.
RESULTS
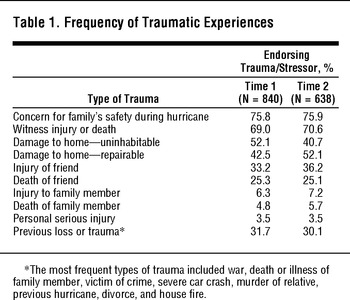
First responders who were surveyed reported that they experienced a multitude of significant losses and stressors, including loss of home, separation from family, and stressful working conditions. Table 1 details the percentage of first responders who experienced hurricane-related traumas and losses. At time 1, 44.6% of respondents reported that they would participate in mental health services if they were offered; 47.8% reported interest in mental health services at time 2. At time 2, 12.7% of respondents reported that they had received individual counseling and 3.5% had received family counseling.
TABLE 1 Frequency of Traumatic Experiences

Alcohol Use and Partner Conflict
In our sample, more than 20% of individuals reported an increase in frequency of alcohol consumption at time 1 (20.2%) and time 2 (20.6%). Participants reported an even greater increase in the amount of alcohol consumed in a single sitting in the aftermath of Hurricane Katrina. At time 1, 30.5% reported an increase in the amount of alcohol consumed in a single sitting and at time 2, 32.7% reported an increase in amount of alcohol consumed in a single sitting. Overall, at time 1, 40.6% reported an increase in either frequency or amount of alcohol consumed and at time 2, 40.1% reported an increase in either frequency or amount of alcohol consumed. Increase in partner conflict was also a commonly endorsed symptom of distress; 42.7% of respondents reported an increase in partner conflict at time 1 and 41.0% reported an increase in partner conflict at time 2.
Symptomatology
Table 2 presents the descriptive statistics for symptoms of PTSD and depression. At both time points, approximately 10% of respondents met the cutoff for symptoms of PTSD, and between 20% and 30% endorsed PTSD symptom criteria of reexperiencing, avoidance, and hyperarousal. Overall, 26.4% and 24.9% met the depression cutoff at time 1 and time 2, respectively.
TABLE 2 Descriptive Statistics on Depression and PTSD Symptoms

To test the research hypothesis—symptoms of PTSD and depression remained high over time—symptom cutoff scores from times 1 and 2 were compared. As a more conservative estimate, the PTSD severity score (cutoff of 50) was used for the analysis. McNemar tests failed to reveal statistical significance on the PCL-C, χ2(1, n = 87 ) = 24.29, P = .99, and the CESD-C, χ2(1, n = 87 ) = 11.29, P = .21. Results suggest no difference between symptom cutoff scores from time 1 to time 2 (Table 3).
TABLE 3 McNemar χ2 on Symptom Cutoff Score by Time (Time 1 vs Time 2)

DISCUSSION
Given the high incidence of trauma, it is expected that some first responders would experience psychological symptoms in the form of anxiety and depression. Specifically, more than 25% of the respondents experienced the following: witness injury or death (70%), damage to home (93%), injury to a friend (25%), and previous loss or trauma (30%). The data collected indicate that the severity of the traumas experienced from both the impact of Hurricane Katrina and subsequent recovery has important mental health implications. The data also revealed self-reports of increased alcohol use (40%) and partner conflict (41%). Although they are resilient and hard working people, first responders in the present study have an expectable incidence of PTSD symptoms (10%) and even higher incidence of symptoms of depression (25%). Consistent with other literature demonstrating the long-term effects of disaster on first responders,Reference Gersons, Carlier, Lamberts and van der Kolk22 the findings of the present study show no decrease in PTSD or depressive symptoms within 18 months of Hurricane Katrina. These findings demonstrate the need for long-term mental health services for first responders. The finding that more than 45% reported that they would participate in mental health services if they were offered reflects positively on the respondents' recognition of the need for services when necessary and their readiness to use the services that are offered.
Given the long-term psychological sequalae of this disaster, the fallout from symptoms of depression and PTSD need to be considered and preventive services put in place. With such symptoms, there is a high risk for effect on occupational and social functioning. There is also increased risk for severe psychopathology and suicide. These symptoms require evidence-based treatment, including medication when necessary to prevent or interrupt a cycle of persistent difficulty. Reports of symptoms of anxiety or depression should be attended to so as to prevent ever-increasing symptoms, which could have a negative effect on the first responder and his or her family.
Limitations
Although this study has much strength in describing the effects of Hurricane Katrina on first responders, there are unavoidable limitations to assessing individuals in a postdisaster environment that related to representation and sampling and generalizability of the findings. Because of the fluidity of emergency personnel at this time, along with city and parish furloughs, it is not possible to provide a totally accurate estimate of the population providing first-responder services. Similarly, the option of self-selection could have introduced bias to the overall sample, especially with the 87 individuals self-selecting into the follow-up subsample. Even with these limitations, the overall percentages from this study are similar to those from first responders after the Oklahoma City bombing and World Trade Center attacks, which ranged from 6% to 17% for PTSD21Reference North, Tivis and McMillen41Reference North, Tivis and McMillen42Reference Zimering, Gulliver, Knight, Munroe and Keane43Reference Daly, Gulliver, Zimering, Knight, Kamholz and Morissette 44Reference Fullerton, Ursano and Wang45 and 22% for depression.Reference Fullerton, Ursano and Wang45
CONCLUSIONS
A number of important lessons have been learned from Hurricane Katrina, with the devastation it caused and the region's resulting slow recovery from the storm's effects. First, comprehensive plans for first responders and their families need to be implemented before a disaster. Given the high percentage of first responders who reported concern for their family's safety during the hurricane (76%), first responders need to be reassured of family members' successful evacuation, safety, and whereabouts, just as family members need to have contact information, methods to obtain help, and plans for reunion. Second, the slow recovery of the community is associated with chronic stressors. First-responder infrastructure needs to be restored as rapidly as possible. Lingering displacement and restoration of equipment, together with the fragmentation of normal complementary services (hospital emergency departments and beds), contribute to declines in morale and function.
Lessons also were learned that may help the mental health community better serve first responders after a disaster. First, the Crisis Counseling Assistance and Training Program of the Robert T. Stafford Disaster Relief and Emergency Assistance Act46 needs to be modified; although helpful, it prohibits mental health diagnosis and treatment, which is so vitally needed with a disaster of the magnitude and the expectable slow recovery of Hurricane Katrina. Second, professionals and peer counselors who volunteer during the crisis should be trained before being deployed during the crisis. They should receive training that is relevant to the special needs of first responders, including the culture of first responders and their organizations. Third, mental health services are needed in the short and long term. These services need to be provided by trusted professionals who are not responsible for administrative decisions, such as fitness for duty. The professionals should be available in responder-friendly settings, be able to coordinate and collaborate with peer counselors, and provide confidential, destigmatized services. Although some services will be required to be in offices or other settings, most can be offered in the field. Providing services in this manner contributes to high acceptability and comfort for responders and their families. Finally, further research on identifying protective factors among first responders, which foster resilience and enhanced recovery, is needed. With this research, mental health professionals can deploy interventions that foster resilience and that most effectively treat the mental health needs of first responders and their families.
Author Disclosures: The author reports no conflicts of interest.
Acknowledgments: We are grateful to the courageous first responders and their families for their cooperation with the screening; without them, this project would not have been possible. We are indebted to Anthony Speier, PhD, coordinator of disaster services, Louisiana Department of Health and Hospitals, Office of Behavioral Health, for continuing leadership and guidance. We also thank Charles Curie, MA, ACSW, who at the time of the surveys was administrator with the Substance Abuse Mental Health Services Administration, US Department of Health and Human Services, for support and encouragement. We express appreciation to our staff, including Richard Costa, PsyD, Amy Dickson, PsyD, Susan Hoffman, LCSW, Tonia Jackson, PhD, Heidi Leffler, LCSW, Patricia Morse, LCSW, PhD, Edward Morse, PhD, Vanice Packer Zenon, MSW, Kerry Wiltz, and Ashley Dantagnan for data collection and management for this project.