Survival in CHD has increased markedly in recent decades due to advancement in diagnostics and treatment with approximately 90% of children living until adulthood. Adults with CHD comprise 66% of the total CHD population.Reference Baumgartner, Bonhoeffer and De Groot1 One consequence of increased survival and the predominately palliative nature of surgical treatments provided is that the majority of adults with CHD surgical patients require lifelong care. Many post-surgical issues including residual arrhythmias, heart failure and/or pulmonary hypertension,Reference Baumgartner, Bonhoeffer and De Groot1 and complications such as stroke, depression and neuropsychological symptoms, affect health-related quality of life.Reference Westhoff-Bleck, Briest and Fraccarollo2 A recent systematic review and meta-analysisReference Ladak, Hasan and Gullick3 revealed that while lower middle-income countries have higher rates of adults with CHD, little health-related quality of life research is conducted or reported from these countries. This is an important deficit given that resources to improve health-related quality of life must be carefully targeted in lower middle-income countries where poor resource availability, accessibility and affordability of services often result in late diagnosis and subsequent complications peri- and post-operatively.
Health-related quality of life issues for adults with CHD are diverse and complex and include physical limitations due to symptoms related to cardiac function uncertainty about their future, psychological challenges and coping with life following surgery.Reference Birks, Sloper and Lewin4 As a result poor health-related quality of life in adults with CHD, particularly in the domain of physical functioning,Reference Kahr, Radke and Orwat5,Reference Fteropoulli, Stygall and Cullen6 is frequently reported in systematic reviews and meta-analyses.Reference Pike, Evangelista and Doering7–Reference Walker, Temple and Gnanapragasam10 The worst health-related quality of life outcomes are primarily associated with socio-demographic factors including less financial resources,Reference Vigl, Niggemeyer and Hager11 lower national gross domestic product and healthcare system factors, with High Income Countries (HIC) demonstrating higher health-related quality of life.Reference Moons, Kovacs and Luyckx12
Early diagnosis, particularly prenatal diagnosis, and early management support better outcomes.Reference Calderon, Angeard and Moutier13 Gender may also predict outcome, again inconsistently, with one study demonstrating poorer health-related quality of life for malesReference Eslami, Macassa and Sundin14 and another for females.Reference Chen, Liao and Wang15,Reference Ladak, Hasan and Gullick16 In addition, psychosocial factors including the coping styles,Reference Eslami, Macassa and Sundin17 and self-perceptions of adults with CHD particularly in relation to the social norms and cultural values are also predictors of health-related quality of life.Reference Rassart, Apers and Kovacs18
Given the complexity of health-related quality of life in adults with CHD and the multiple factors influencing outcomes, findings from HICs may not be generalisable to lower middle-income countries.Reference Farhat, Abdul-Sater and Obeid19 We therefore conducted a mixed-methods study to address the gap in lower middle-income countries knowledge and to further understand quantitative data findings through concurrent qualitative inquiry.Reference Castro, Kellison and Boyd20 We addressed the following research questions:
1. What is the health-related quality of life of CHD surgical patients at a tertiary hospital in Pakistan?
2. How do individual and environmental considerations influence the experiences of surgery, recovery and living with CHD for these young adult patients?
Methods
Design
The convergence model of a concurrent nested mixed-methods design,Reference Castro, Kellison and Boyd20 recommended for research on outcomes, provided a comprehensive understanding of health-related quality of life from multiple perspectives. In a concurrent design, quantitative and qualitative data are collected simultaneously. While the qualitative data came from a nested sample of a larger set of participants completing health-related quality of life measurements, in our interpretation it carries equal weight (quantitative and qualitative). The convergent model means that once analysis is complete, the overall interpretation of findings occurs simultaneously and is enhanced by a joint display of data guided by Wilson and Cleary’s health-related quality of life model (see Fig 1).
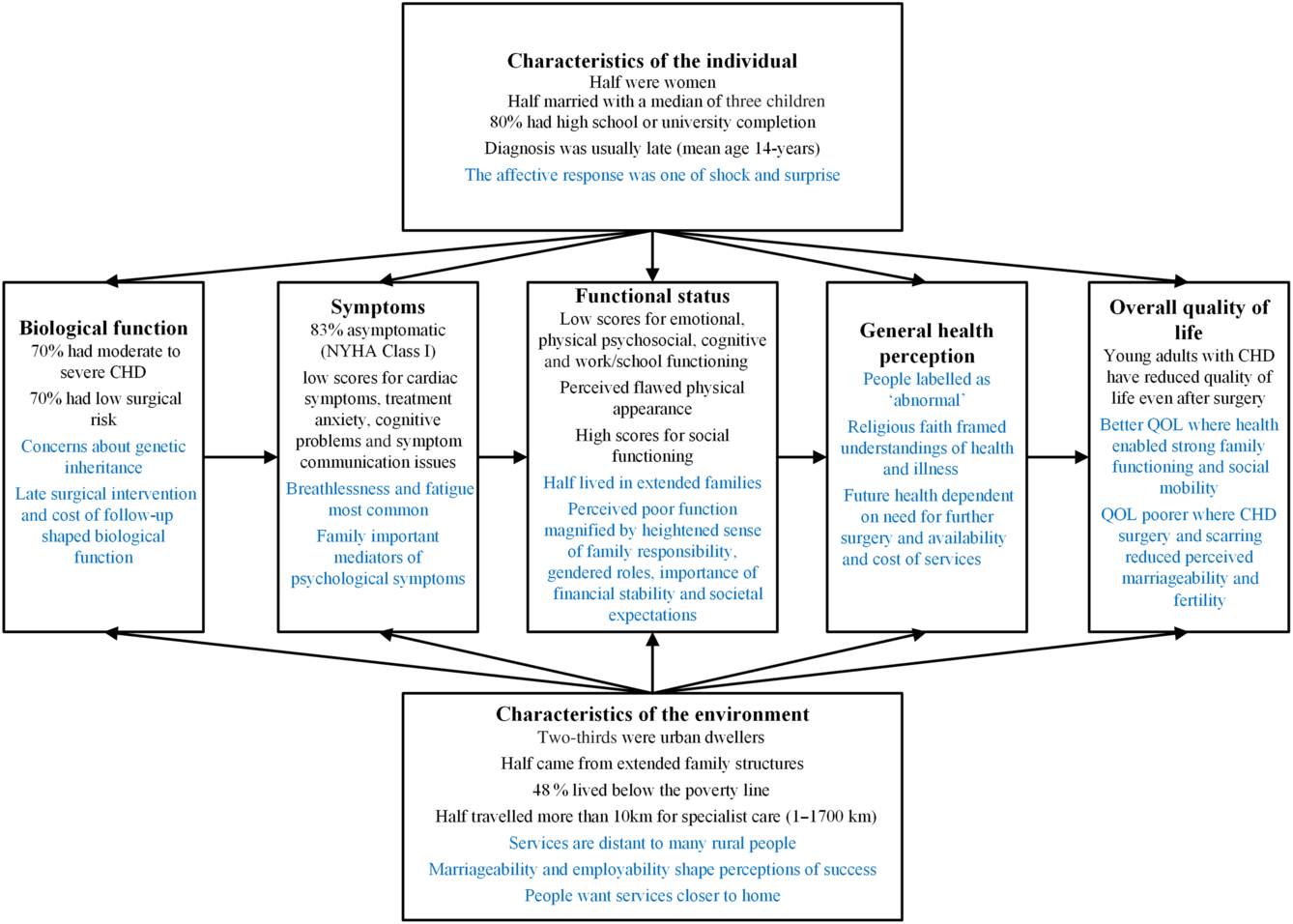
Figure 1. Revised Wilson and Cleary model for health-related quality of life – quantitative data and qualitative data.
This paper reports a sub-study of a larger study which compared health-related quality of life in CHD patients following corrective surgery with age-matched siblings and parental reports. A detailed report of the study’s methodology and theoretical framework can be accessed in our protocol paperReference Ladak, Hasan and Gullick21; however, an overview is provided below.
Theoretical framework
The modified Wilson and Cleary model of health-related quality of lifeReference Ferrans, Zerwic and Wilbur22 guided the study concept, conduct, analysis and reporting (Fig 1). This model assisted us to identify relationships between biological function, symptoms, functional status and general health perceptions, with each element influenced by both individual and environmental characteristics impacting the overall health-related quality of life. The quantitative and qualitative data are integrated within each aspect of the model to provide an in-depth understanding of the health-related quality of life of young adults in Pakistan who have experienced a surgical procedure for adults with CHD.
Sample and setting
The study was conducted at a large private teaching hospital in urban Pakistan. Eligible patients were identified from a hospital database and were mailed a letter of invitation. Alternatively, suitable participants were provided a letter of invitation during an outpatient clinic and were given time to consider their participation. This letter of invitation contained the contact details of the research team, and participants contacted the team directly if they were interested in taking part. Participants were at least 1-year post-CHD surgical correction/palliation (surgery between 2008 and 2015), were ≥ 18 years of age, had no chromosomal abnormality, could understand English and/or Urdu and were willing to attend a face-to-face interview.
A subset (n = 17) of patients enrolled in the quantitative study (n = 59) engaged in a single-qualitative, semi-structured interview focusing on the experiences of CHD and health-related quality of life before and after CHD surgery. The CHD patient recruitment process is described in Fig 2.

Figure 2. Study patients recruitment flow diagram – health-related quality of life in adult CHD surgical patients in Pakistan.
Data collection
Socio-demographic data were collected directly from participants and their clinical/surgical data from medical records. For the quantitative arm, health-related quality of life data were collected using the young adult (age 18–25 years) or adult (age 25 years above) versions of the PedsQL™ 4.0 Generic Core Scale and the PedsQL™ Cognitive Functioning Scale (Supplementary Table 1). Disease-specific health-related quality of life was explored with the PedsQL™ 3.0 Cardiac Module. All questionnaires have well-established validity and reliability.Reference Varni and Limbers23 The Mapi Research Trust approved the use and translation of questionnaires to Urdu (Pakistan’s local language).
Table 1. CHD patient socio-demographics characteristics

* Sub-sample of quantitative enrolled participants
The qualitative interviews, aided by an interview guide (Supplementary Table 2), were conducted in Urdu, audio-recorded and translated to English by the primary researcher (LAL).
Table 2. CHD patient clinical characteristics

RACHS=Risk-Adjustment for Congenital Heart Surgery.
* Sub-sample of quantitative enrolled participants
** Patients on cardiac medications: Angiotensin Converting Enzyme (ACE) inhibitors (n = 4, 6.8%), beta blockers (n = 4, 6.8%), anti-coagulant (n = 6, 10.2%), ACE inhibitors + beta blockers (n = 5, 8.5%), ACE inhibitors + anti-coagulant (n = 6, 10.2%), beta blockers + anti-coagulant (n = 3, 5.1%) and ACE inhibitors + beta blockers + anti-coagulants (n = 3, 5.1%)
Data analysis
Quantitative data were analysed using the Statistical Package for Social Sciences (IBM SPSS Statistics 22, University of Sydney, Australia). Means and standard deviation and/or median and interquartile range were calculated for continuous variables. Frequencies were calculated for categorical variables. Researcher-administered questionnaires ensured no missing data, and 80% of the participants preferred the questionnaires to be administered in the local language, Urdu. Descriptive demographic data were analysed for socio-demographic, clinical and surgical variables.
Qualitative data were initially coded inductively by two researchers (LAL, JG) using the qualitative content analysis steps described by Graneheim and Lundman.Reference Graneheim and Lundman24 A third author (RG) confirmed resonance of the identified themes. The Wilson–Cleary theoretical model of health-related quality of life then provided a further analytic lens bringing a deductive element to our analysis. This combination of inductive and deductive analysis has been used in past descriptive qualitative research to enhance theoretical rigour.Reference Jin, Neubeck and Koo25
Integration of methods
The approach to integration of qualitative and qualitative data is an important consideration in mixed-methods research.Reference Klassen, Creswell and Clark26 We have chosen the point of interface between quantitative and qualitative data to occur in the interpretation phase, using the conceptual elements of the modified Wilson–Cleary model to guide this integration and to organise presentation of findings (Fig 1).
Rigour
We considered published best practices for mixed-methods approaches in quality-of-life research.Reference Klassen, Creswell and Clark26 Our reporting of qualitative findings is guided by a quality framework for qualitative content analysis.Reference Elo, Kääriäinen and Kanste27 Back translation of key exemplars with a second bilingual researcher enhanced confidence in the data quality.Reference Van Nes, Abma and Jonsson28
Ethical considerations
The study protocol was approved by the ethics review committee of The Aga Khan University, Pakistan (3737-Ped-ERC-15). All participants provided written consent. Participants in the qualitative findings are referred to by pseudonym.
Results
Characteristics of the individual
The revised Wilson and Cleary model of health-related quality of lifeReference Ferrans, Zerwic and Wilbur22 proposes that the characteristics of the individual permeates all other domains. These individual characteristics include age, sex and marital status, biological factors such as genetic history and psychological factors such as affective response to the disease process (Table 1).
Sex was equally distributed with the mean age 29.66 ± 10.70 years. There were high levels of literacy with approximately 80% (n = 48) having high school or university completion. Despite high levels of education, around half were living below the World Health Organization’s poverty line for lower middle-income countries. Married participants comprised 48% (n = 28), 43% (n = 12) were women and these participants had a median of three children (range 0 to 6).
The CHD diagnosis occurred later than for HIC at a mean age of 14 years, and the affective response was shock and surprise. Gulzar (female, 39 years) was diagnosed at 33 years: “I was very surprised when I learned about my condition, but thank God, I was diagnosed after my marriage.” Saleem (male, 21 years) was diagnosed with a ventricular septal defect during his first year of life but did not receive surgical correction until 18 years of age. His emotional response to the shock of his diagnosis was avoidant coping: “I avoid and ignore it as an accident… and do not think about it.”
Characteristics of the environment
Wilson and Cleary’s characteristics of the environment address the physical environment (including the home, neighbourhood and workplace) and social environment (including society, culture, family structure, friends and healthcare providers).Reference Ferrans, Zerwic and Wilbur22 Approximately, two-thirds of these participants (n = 46, 78%) were urban dwellers (Table 1). The median distance of the available cardiac facility from participants’ residence was 10 km (range 1 to 1700 km). This may partly explain the substantial gap from last cardiologist follow-up of median 2.5 years (range 5.74 to 0 years). Common reasons for lack of follow-up were cost or inconvenience of travel and transportation, or that follow-up was not required by the cardiologist.
There was an equal representation from nuclear and extended families. Sadaf (female, 25 years) explained the important social function of extended family life: “In our family… my brother, sister-in-law, we all live together; we stay up ‘til late at night and talk’, we dine together…” Extended explanations of the individual and environmental characteristics are explored under the domains of biological function, symptoms, functional status, general health perceptions and overall quality of life.
Biological function
In the Wilson & Cleary Model, biological function addresses the molecular, cellular and whole organ function, including genetically linked disease. In our study, biological function is influenced by the type of CHD, and other surgical/clinical variables, particularly CHD severity. Nearly 70% of participants were acyanotic, and ~70% had moderate to severe CHD severityReference Warnes, Liberthson and Danielson29 (Table 2). Around 70% fell into Class 1 and 2 Risk-Adjustment for Congenital Heart Surgery suggesting they had low-risk surgery. Despite ~83% of patients being New York Heart Association (NYHA) Class I, half were prescribed cardiac medications including angiotensin-converting enzyme inhibitors, beta blockers and anti-coagulants (or a combination). Participants did not discuss the quantified severity of their diagnosis/procedure, rather they described the impact of the disease in terms of symptoms and function, particularly their ability to contribute to family and society. The biological impact of CHD on participants occurred at an early age.
Qualitative data suggested that an individual’s genetic history was the main biological concern of participants because of the potential impact on the health of their children. One participant’s child had received a CHD diagnosis, and another was anticipating a diagnosis based on symptoms. Their concern about transmitting a congenital defect arose from their own experiences of living with CHD symptoms and undergoing surgery.
For example, Dilshad (female, 31 years) with atrial septal defect repair and pulmonary valve replacement had a daughter diagnosed with atrial septal defect. She was concerned and protective of her daughter facing surgery: “I have been through this operation and I know how painful it is. I am very worried. How will she bear this major surgery and the pain?”
An important contextual element was the available health system and resources: the timing of corrective surgery shapes biological function, and in Pakistan, this timing is likely to be mediated by social, economic and resource factors. While Sadaf (female, 25 years) was diagnosed during her first year of life, her family decided against surgery for financial reasons, and because they feared losing their child. Sadaf pursued surgery as an adult for symptom control: “Everyone [family] was against it… but when I grew up, I took the decision… I was suffering a lot”.
The economic environment had consequences beyond the surgery itself and was also impacted by geographical factors. Participants described the burden of hospital and after-care costs to correct their biological dysfunction. Zahir (male, 32 years), a construction labourer, lived below the poverty line:
…I didn’t have funds for [surgery]. Someone else was supporting me… For patients with low income, there should be less medicines and visits… It takes 3-hours for me to travel to the hospital one-way and I miss my whole day’s wage.
Including the larger family unit in discussions about surgery and prognosis may be particularly important in a collectivist society. When the family understood the clinical importance of an individual’s surgery to prognosis and health-related quality of life, there was greater acceptance. Rufaida (female, 38 years), recently diagnosed with atrial septal defect, had immediate surgery. Her husband’s professional understanding framed his supportive and caring approach: “My sisters, brothers and most importantly my husband [a doctor] and kids supported me in having the surgery… from the time of diagnosis”
The extended family structure could provide either a buffer to the shock of diagnosis, or a catalyst to self-doubt. Shehzad (male, 22 years), living in an extended family of 27 people explained:
Most family members and neighbours were supportive at the time of operation… A few criticized me… How will I manage after heart surgery? Will I be able to work? Can I marry?… Will I be able to lead normal life?
The influence of family in decision-making had significant impact for Amina (female, 30 years). CHD as a derangement of her biological function led to her baby’s death. The family environment, and their subsequent decisions to protect her from bad news, shaped her affective response to the disease:
I found out about my heart problem in the seventh month of pregnancy and became very sad… I was delivered early because of my health issues. I was told about my daughter’s death after two-months. I was completely shocked…
Symptoms
In the Wilson and Cleary model, symptoms are defined as subjective experiences of disease. In other words, it is a paradigm shift from the cellular to the personal level. The symptom domain incorporates aberrant physical and emotional states and the person’s interpretation of these. This includes somatic perceptions of external stressors, and cognitive processing and beliefs about the disease causes, consequences, progression and cure.
About 83% of participants were asymptomatic: NYHA Class I (Table 2). Mean symptom scores related to the specific cardiac diagnoses were low across the whole cohort (79.41 ± 18.05), with no statistically significant difference in symptom scores between mild versus moderate and complex CHD severity (Table 3). The most frequent physical symptoms were breathlessness and fatigue. Participants had low scores in treatment anxiety (83.15 ± 30.88), cognitive problems (89.69 ± 17.6) and communication about symptoms and health issues (89.26 ± 22.69).
Table 3. HRQOL in CHD patients

HRQOL=health-related quality of life.
Significant p value <.05. No significant p value reported in general- and cardiac-specific HRQOL between mild and moderate CHDs.
Qualitative data confirmed that surgery improved symptoms for some participants and this seemed dependent on the type of surgery available and the complexity of their disease. Sadaf (female, 25 years) had significant improvement in physical symptoms after Aortic Valve Replacement (AVR) and ventricular septal defect repair: “Before I used to get lethargic… my heart rate was very rapid especially at night. I couldn’t sleep properly… Now I am alright; much better than before.”
For others, improvement was not always achieved or sustained. Karim (male, 23 years) had a palliative Blalock Taussig shunt for tetralogy of Fallot. Still facing breathing problems, he would have preferred corrective rather than palliative surgery: “This breathing troubles me a lot… When my heart beats fast… I breathe harder and have very bad chest pain. I wish I could have complete surgery to get rid of these symptoms.”
Participants described past symptom experiences affecting their psychological preparedness to engage in activities. For instance, 27-year-old businessman Fawad with AVR and ventricular septal defect repair described anticipatory fear of activity based on past experiences of fatigue: “I still feel tired, which I was before [surgery]… I cannot drive a car. I feel afraid [to do] any activity. I don’t feel strong or energetic.”
Co-morbid conditions worsened the symptom experience. Amina (female, 32 years) was haemodialysis-dependent: “I have kidney failure, so when water starts accumulating in my body, I get breathing problems.” She also described psychological symptoms: “I get irritated by even small issues. I start fighting and have become stubborn.”
While chronic pain was rarely described, acute pain was described post-operatively. Fozia (female, 26 years), described how after mitral valve replacement and atrial septal defect repair: “I was in deep pain… I couldn’t move… I had two tubes in my chest and when they took it out, it was a terrible experience…”.
The social environment influenced participants’ symptom experience. While psychological symptoms were less often described, when they did occur, family and social context were important mediators. Zahir (male, 32 years) explained: “After surgery, I went into depression… I used to wake abruptly and then couldn’t sleep… My family would stay with me until I went back to sleep… I thought people would say I’ve become crazy, but I was frightened.”
Zahir also experienced panic attacks in public places that limited his mobility and independence: “When I sat in a bus or went to crowded place… my heart would beat faster… I felt the bus would have an accident and I was very scared… I was sweating… I could not go anywhere alone.”
Functional status
Functional status can be viewed from both a disablement perspective, and from the point of optimisation of remaining function in physical, emotional, social and cognitive domains.Reference Ferrans, Zerwic and Wilbur22 Functional status is influenced by individual characteristics of self-efficacy or by environmental characteristics such as social support and the profile of the community.Reference Ferrans, Zerwic and Wilbur22 For general health-related quality of life, except for social functioning, mean functional status scores were low across domains with the lowest mean scores in emotional functioning (71.61 ± 20.6) followed by physical (78.81 ± 21.18), psychosocial (81.98 ± 15.29), total (81.19 ± 15.52), cognitive (82.27 ± 22.31) and work/school functioning (82.75 ± 17.6) (Table 3). Social functioning was considered high (92.88), and this may be due to around half the participants living in extended families.
The lowest health-related quality of life scores were related to heart problems/cardiac symptoms (79.41 ± 18.05), followed by treatment anxiety (83.15 ± 30.88), perceived flawed physical appearance (85.31 ± 24.48), communication problems (89.26 ± 22.69), cognitive problems (89.69 ± 17.60) and treatment-related problems (92.34 ± 11.49). There was no statistically significant difference in functional domains of health-related quality of life (either generic- or disease-specific) between mild versus moderate and complex CHD severity.
Surgery improved perceived functional status for some individuals with previous functional deficits. AVR and ventricular septal defect correction allowed Sadaf (female, 25 years) to meet functional goals that were personally satisfying and allowed her to feel normal within her community: “Before, I wasn’t able to work a lot, but now I can work on my own… I can even lift my niece and nephew. I am able to do everything I feel like… They (family, friends) perceive me as normal.” Similarly, Amina (female, 32 years) felt a drastic improvement in functional status immediately after tetralogy of Fallot correction: “After 3–4 months I started doing all the housework like cleaning, cooking, washing clothes… I was perfectly alright.”
For other participants, CHD symptoms caused physical function deficits that persisted after surgery. For example, breathlessness could be precipitated by routine daily activities. Rufaida (female, 38 years) explained that after atrial septal defect repair: “If I… bend, pick up something heavy… knead dough or even wash dishes, climb stairs or speak a lot, then I get breathless…”
Moving towards “feeling normal” was important to participants, and their normal functional status was shaped by Pakistan as a collectivist society.Reference Islam30 This was magnified by the sense of family responsibilities, the gender-specific nature of contributions, the importance of financial stability and the expectations of society. Functional status was also a gendered construct. Gulzar (female, 39 years) explained: “I try my best to complete tasks on time, but I’m always late… My friends complete their work in a few hours… but my entire day is spent completing housework”
Males, who tend to shoulder the weight of responsibility for family and extended family in Pakistan, were challenged by functional limitations. Fawad (male, 27 years) living in an extended family of nine explained:
I don’t want to go for more surgery… I am the eldest son, my father is looking after the entire business… I have an unmarried sister… I need to remain fit to fulfil all my responsibilities as a son and elder brother.
Karim (male, 23 years) shared his guilt at not supporting his mother and believed his physical limitations meant he could not contribute equally within his family: “Sometimes my mother asks me to do some work… I am not able to… I feel very bad. All my brothers work so much and I’m the only one not able to do anything. It really hurts me.”
Reduced functional capacity led to financial dependency. This was distressing because participants relied on family members who had limited financial resources. They felt more comfortable relying on parents than having a future reliance on siblings or extended family. The lack of clarity around who would support and subsidise their future health and well being brought great uncertainty. Sadaf (female, 25 years), who lived below the poverty line within an extended family, explained:
My father has passed away. If God forbid, something happens to my mother, then who is going to take care of me?… What bothers me is whether they [brothers] are going to support me financially… get my medical check-ups?
Employability was a concern with no unemployment benefits in Pakistan, exacerbating their already low family income. Some participants felt excluded from the job market because of their CHD. Karim (male, 23 years) explained: “I have completed my studies, I am looking for a job but not getting any… I have applied but I haven’t received a response. I think it’s because I told them… I have a heart problem”.
General health perceptions
We did not have quantitative health-related quality of life findings that mapped directly to general health perceptions. The Wilson–Cleary model sees general health perceptions as an overall, subjective perception of health. While inclusive of biological, symptom and functional domains, the ratings are particularly influenced by the seriousness of health issues, particularly those perceived to be life threatening.Reference Ferrans, Zerwic and Wilbur22
A few participants attributed their survival to CHD surgery. Sadaf (female, 25 years) attributed her ability to achieve general health and developmental milestones to her ventricular septal defect repair and AVR at 18 years of age: “Before surgery I was too short but… within 6-months I started to grow and even my family witnessed this change. They were thankful to God [Allah]”
The diagnosis, when unexpected, made people more aware of possible morbidity and mortality. Fayyaz (male, 32 years) did not know of his aortic stenosis until adulthood and had few symptoms. As a result, he was actively engaged in, and enjoyed, active sports. After AVR and permanent pacemaker insertion, he viewed his body as vulnerable, requiring continuing need for caution after surgery: “Now I have to be careful about things… I like playing cricket and I have to be careful if the ball hits me, or if I run fast I might have problems.”
The social environment set the bar for what was considered “normal” health for people striving to overcome the consequences of CHD. Many participants described feeling labelled as “abnormal” from both within and outside of the family. This could either challenge or support the surgical pathway. While Fozia (female, 26 years) felt normal, she found Pakistani society to be discriminating and closed-minded: “I am happy with my life. I know I’m medically fit and I have no problems… But society… is not accepting of people like us.”
Shehzad (male, 22 years) felt his need for medication would frame him as abnormal:
It was my cousin’s marriage and I was staying at his place. I didn’t feel comfortable taking medicine in front of them so I skipped my medicine… People think negatively about medicine, that I am not normal.
CHD was experienced by these Pakistani patients within the religious understandings of daily life. Gulzar’s (female, 39 years) family viewed CHD as a punishment from God, but her own faith insulated her: “My cousin told me that this disease is due to my sins, but I don’t feel that way. I think God can give disease to anyone.”
Fatima (female, 20 years) was comforted by the religious faith and practices, and the physical presence of loved ones at times of greatest need: “When I was going through this operation they all prayed for me, recited the Quran [Muslim’s holy book] for me and came to visit me…”
The greatest sources of support for general health were from parents and spouses, especially for women. Ramsha (female, 34 years) described a collaborative approach to problem-solving around her illness, “I came to know about it after my marriage so me, my husband, my family and in-laws… we discussed how to deal with this situation”
General health perceptions were sometimes clouded by the possibility of further surgery, particularly for participants with artificial valves. Fozia (female, 26 years) explained: “I might need more surgery in future… The experience was very painful and I wouldn’t want to go for it again.”
Participants voiced the need for more cardiac facilities. Fatima (female, 20 years) from a distant rural village asserted, “We want new hospitals to be constructed in our country, in all the cities and villages where heart patients can consult good doctors.”
Overall quality of life
At an individual level, the overall quality of life is measured by internal standards including values, expectations, aspirations, personal needs and how one compares oneself with others. These then interact with the environment.Reference Ferrans, Zerwic and Wilbur22
People’s personal understandings of good overall quality of life incorporated individual factors that enabled family functioning and social mobility. For married participants with children, their capacity to care for and educate their children was paramount to their quality of life. Zahir (male, 32 years), a married male with five children explained, “The most important thing is health. If your health is good, you can take care of your kids and family.”
The consequences of ongoing CHD symptoms affected the individual’s projection of future possibilities. Rufaida (female, 38 years) explained: “I want to pursue interior decoration as my career…but due to my condition, I think I’ll be unable to do it.”
In Pakistan, great value is placed on marriageability and fertility, with most participants noting this importance to overall quality of life. In Pakistan, arranged marriage, where a boy and his family formally negotiate marriage based on local measures of eligibility, is a common practice. Fozia (female, 26 years), who was well educated and worked for a multinational company, described people making excuses to avoid marriage proposals once they discovered her CHD surgery:
When I get marriage proposals, they liked my appearance, my personality, my family’s prestige… But when my father tells them about my surgery… even sharing the doctor’s report that I was fine… First, they rejected me because of my heart surgery and secondly, they fear I will not be able to conceive and I’m not medically fit. But they would come up with silly excuses…
Pakistan is a society where people do not feel comfortable discussing their sex life openly. Four female participants highlighted the need for a female counsellor to discuss their sex- and conception-related issues. While some participants shared their concerns at interview, they requested these not be recorded on the interview transcript.
The likelihood of marriage and conception was linked to the presence of a surgical scar. Although the perceived physical appearance score was low at mean 85.31 ± 24.48, most female participants wore a “hijab” (scarf that covers neck and head) and were married at the time of their surgery, reducing their concerns. Nazia (female, 20 years) accepted her scars with time, as God’s wish:
If it happened before marriage, I would have been more concerned and so would my family. I was concerned about operation marks, ‘What will my husband or in-laws think?’ but thank God, my husband is okay with it.
Discussion
This study provides consideration of important socio-cultural elements arising from characteristics of both the individual and the environment for the health-related quality of life of CHD surgical patients. It also validates the application of the revised Wilson and Cleary modelReference Ferrans, Zerwic and Wilbur22 in this condition and the paradigm shift of health-related quality of life from cellular to the individual level particularly from lower middle-income countries’ perspective.
The study highlights lower health-related quality of life in all domains of general- and cardiac-specific quality of life for CHD surgical patients. Cardiac symptoms affected participants’ health-related quality of life even after surgery, particularly their emotional and physical functioning which is in agreement with other studies.Reference Eslami, Macassa and Sundin14,Reference Ladak, Hasan and Gullick31–Reference Jackson, Hassen and Gerardo33 The APPROACH IS study (15 countries across five continents) reported an overall good quality of life and life satisfaction in adults with CHD but high cross-country variability.Reference Apers, Kovacs and Luyckx8 While these differences may arise from variability in income, the use of a linear analogue scale for life satisfaction, rather than standard health-related quality of life tools may also have been possible reasons for this variability.
The lowest functional domain of health-related quality of life in the current study was emotional functioning. Adults with CHD are at high risk of depression, and mental health compromise has been reported previously.Reference Westhoff-Bleck, Briest and Fraccarollo2 Sources of distress that were context-specific included that physical limitations prevented them from fulfilling responsibilities assigned by family and society which have a unique framing in Pakistan. Society’s perceptions and reactions following CHD diagnosis/surgery shaped participants’ sense of self within their family and community.
Health-related quality of life measurement provides a means of self-appraisal and communicates the individual’s functioning and disease,Reference Schoormans, Mulder and van Melle34 their self-control over symptomsReference Rassart, Apers and Kovacs18 and is shaped by society and culture.Reference Diener, Suh and Smith35 Although people from Western cultures tend to assign illness to its biomedical definition, non-Western cultures define illness in relation to social norms and culture.Reference Friedman36
So it was interesting to note that social functioning in this cohort was higher compared to other health-related quality of life domains. This could be explained by most participants living in an extended family structure. Family support has been highlighted as an important contributor to emotional and social supportReference Eslami, Macassa and Sundin14,Reference Larsen, Jacobsen and Emmertsen37 and informs a problem-solving approach to coping.Reference Eslami, Macassa and Sundin17 It has been proposed that social support, and family socialisation accompanied by childhood experiences of overcoming adversity, may build a sense of coherence that improves quality of life in CHD.Reference Moons and Norekvål38 Pakistan is a patriarchal society which assigns gender-specific roles to individuals.Reference Rehman and Azam Roomi39 Marriage and conception are important constructs and a measure of social success within Pakistani society. This provides context to the concerns of our participants’ marital status and its impact on a sense of normality.
Poor health-related quality of life has been associated with older age at adults with CHD surgery,Reference Knowles, Veldtman and Hickey32 and in Pakistan, this results from limited healthcare services and thus continuity in care – a common problem in lower middle-income countries. A major obstacle to continuity of care is people’s poor concordance with regular clinic and cardiologist follow-up.Reference Dearani, Connolly and Martinez40 For a population of over 210 million, Pakistan has only five paediatric facilities, 25 cardiologists and eight cardiac surgeons.41 Sixty-two percent of people live in rural Pakistan where accessibility, availability and affordability issues lead to late diagnosis, referral and surgery, aggravating the magnitude of the problem.Reference Mocumbi42,Reference Mocumbi, Lameira and Yaksh43 This requires attention, as evidence links regular follow-up for adults with CHD to less urgent cardiac management and fewer health-related issues.Reference Yeung, Kay and Roosevelt44
Research from HICs has demonstrated that nurse-led heart failure clinics can improve both self-care behaviours and survival.Reference Liljeroos and Strömberg45 With training, specialist nurses can contribute to building adolescent and young adult skills in care participation, self-advocacy, career planning and job suitability.Reference Lantin-Hermoso, Berger and Bhatt46
This study highlights that health-related quality of life should be part of routine clinical screening to ensure realistic expectations by patients and family for symptom and functional improvement at the least, but also to inform decision-making about treatment options, health expenditure and appropriate referrals.Reference Ladak, Hasan and Gullick16 There is an urgent need to develop national registries to consolidate meaningful epidemiological and health-related quality of life data and to respond with contextual strategies that have underpinned important advancements in HICs.
There are some limitations to this study. First, the study was conducted in a single-centre, private hospital that may have attracted participants with a skewed socio-demographic profile. While this study hospital sees patients from across Pakistan and provides subsidised care to people with poor financial resources, findings should be generalised to public settings with caution. Second, we used a convenience sample of eligible patients willing to come for study interviews. As many potential patients could not be contacted, or were not recruited due to travelling issues, we may have missed patients from particular CHD diagnoses or enrolled a biased sample. Although we conformed to the translation policy of the Mapi research institute, this is the first time the PedsQLTM was used in this setting, making cross-cultural bias possible. Future research could consider a longitudinal and multi-site mixed-methods approach.
Conclusions
CHD surgical patients reported low health-related quality of life in almost all domains of generic and cardiac-specific health-related quality of life in Pakistan, where social and cultural factors shape illness experience and hopes for the future. The greatest scope for enhanced support is in the area of emotional functioning. Mixed-methods study design provided the opportunity to understand the complex phenomena of health-related quality of life. Clinicians should target improved functional capacity in ways that optimise people’s contribution to family and community life.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951120001663
Availability of Data and Material
Data have been shared as supplementary files.
Acknowledgements
Not applicable.
Author’s Contributors
LAL is a PhD candidate who conceived the study, contributed to the study design, conducted data collection, data analysis, drafted and revised the manuscript.
–RG contributed to the study design, assisted in data analysis and provided critical feedback on the manuscript drafts.
BSH contributed to the study design and provided critical feedback on the manuscript drafts.
KA contributed to the study design and provided critical feedback on the manuscript drafts.
AA contributed to the study design and provided critical feedback on the manuscript drafts.
JG contributed to the study design, assisted in data analysis and provided critical feedback on the manuscript drafts.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Financial Support
This project is unfunded. However, as this study is a component of a PhD thesis, LAL received an International Post-Graduate Research Scholarship and an Australian Post-Graduate Award from The University of Sydney, Australia to pursue Doctoral studies.
Conflicts of Interest
None.
Ethical Standards
This study has received ethical approval from The Aga Khan University, Pakistan, 3737-Ped-ERC-15. Informed consent was obtained from the study participants.
Consent for publication: Informed consent was obtained for the publication. Pseudo names have been used in the manuscript to ensure confidentiality.







