On January 12, 2010, a magnitude 7.0 earthquake devastated the nation of Haiti. Centered approximately 16 miles from the population center of Port-au-Prince, an estimated 230 000 people were killed and another 300 000 were injured. Most of the city's public buildings, roads, private residences, hospitals, sanitation, and water systems were destroyed. More than 2 million people were left homeless in the aftermath. The level of devastation, the island nation's geographic isolation, and the relative lack of options for in-country land-based medical evacuations resulted in an unprecedented need for the treatment of casualties weeks after the quake.
In response to the disaster, the US Naval hospital ship, USNS Comfort (T-AH 20), was activated on January 13, 2010, and dispatched in record time on January 16, 2010, from its home port in Baltimore, Maryland. For 40 days of its 2 months' service, the USNS Comfort provided medical and surgical care to earthquake victims. In conjunction with military units ashore, Operation Unified Response represented one of the largest disaster relief efforts in the US Navy's 235-year history.
The USNS Comfort is 1 of 2 Navy hospital ships and is designed as a fully functional trauma facility at sea. During combat operations, the ship has a theoretical inpatient capacity for up to 1000 patients, including 80 intensive care beds. The ship has radiology services to include fixed and portable x-rays, ultrasonography, 64-slice computed tomography, and an interventional radiology suite. Its blood bank stores up to 3000 units of fresh red blood cells, 2000 units of frozen blood, and carries a limited supply of fresh frozen plasma and cryoprecipitate. The main surgical complex has 12 fully functional operating rooms.
For peacetime operations, the ship can be arranged into 2 primary configurations that differ based on the mission type. The first mission organization is known as humanitarian civil assistance (HCA). This configuration is designed for long-term humanitarian missions such as Operation Continuing Promise, the annual mission to the Caribbean and South America. During these missions, the ship is equipped to meet lower acuity needs. The second mission configuration is disaster response (DR). In comparison with the HCA configuration, in the DR configuration the USNS Comfort is equipped to deal with a higher number of acutely injured patients, although not as high as the theoretical inpatient capacity for combat operations. For the mission to Haiti, the DR configuration was adopted to deal with the high volume of burns, head trauma, amputation, and crush injury expected in the early phase of the response.
Surgical services available on this mission included adult and pediatric anesthesiology,Reference Thomas1 orthopedic surgery, orthopedic trauma surgery, pediatric orthopedic surgery, trauma surgery, adult and pediatric general surgery, vascular surgery, plastic surgery,Reference Ray, Lindsay and Kumar2 otolaryngology, oral surgery,Reference Ray, Lindsay and Kumar2 dermatology,Reference Galeckas3 obstetrics and gynecology, ophthalmology, neurosurgery, and urology. Medical specialties represented on board the ship included internal medicine,Reference Amundson, Dadekian and Etienne4 emergency medicine, family practice, critical care, adult and pediatric cardiology, adult and pediatric infectious diseases, nephrology, gastroenterology, general pediatrics, pediatric endocrinology, developmental pediatrics, pathology,Reference Hussey, Dukette and Dunn5 radiology, neurology,Reference Etienne, Powell and Faux6 and physical therapy. Also present were nurse practitioners, physicians assistants, nurse midwives, and independent duty corpsmen. Translation services were provided by 76 embedded military translators and Red Cross volunteers. At maximum, 1380 military and civilian staff members were on board the ship in support of clinical operations.
The USNS Comfort arrived off the coast of Haiti on the evening of January 19, 2010, and received its first 2 casualties by helicopter as soon as it was within range of its sister ship, the USS Carl Vinson, an aircraft carrier that had arrived 2 days earlier. During operations, patients were triaged by 1 of 2 rapid assessment teams (RATs) comprising a combat-experienced, fellowship-trained trauma surgeon and a communication detail. A RAT was stationed at 2 separate helicopter landing zones (LZs) in Port-au-Prince, and worked with local treatment facilities to identify which patients would be transferred. Patients were transferred primarily by helicopter to the ship and assessed in casualty receiving (CASREC), a 50-bed trauma emergency department. When possible, escorts were transported to the ship alongside injured family members, registered in CASREC, and housed on the inpatient wards. All patients were assessed and interviewed in the presence of a Creole-speaking translator to record the patient's chief complaint, demographics, and medical history. The medical provider recorded a clinical note to include a brief history, physical examination findings, diagnosis, and treatment plan. All patients received a screening portable chest radiograph to assess for evidence of tuberculosis. Other radiographs or imaging studies were ordered according to the patient's medical condition. Specialty surgical consultation was immediately available in CASREC as patients were triaged and assessed.
The broad objective of this report is to document the work of the ship during its 40 days of service in Haiti. More specifically, we provide an analysis of the unique set of circumstances that led the ship to serve an uncommon role in disaster response: that of a foreign tertiary trauma center. Moreover, we illustrate the challenges of triage and treatment in a mass-casualty humanitarian response through observational analysis of the USNS Comfort's patient cohort. Finally, we describe the collaboration between the US military, the Haitian Ministry of Health, and the humanitarian responders to the earthquake, and recognize a useful balance between the responders' differing strategies and resources.
METHODS
The data analyzed included all patients who were evaluated and treated on board the USNS Comfort between January 19 and February 27, 2010, when the last patient was discharged from the ship. On arrival in CASREC, the ship's patient administration department registered all patients and created a medical chart with a unique identifier. Consent for treatment and data collection was obtained at the time of admission in either oral or written form as circumstances dictated. Prospective databases managed by patient administration, radiology, blood bank, laboratory services, and surgical services were combined using the patients' unique medical identifiers to create an overall patient care database, which was retrospectively reviewed for this analysis. Approval for the study was obtained from both the National Naval Medical Center's institutional review board and the Commanding Officer of the USNS Comfort.
RESULTS
During the USNS Comfort's 40 days of operation, 872 patients and 185 patient escorts were processed aboard the ship. The majority of patients were local nationals. In addition, a small number of American citizens and US and Canadian military personnel received care. The 872 patients (817 inpatients and 55 outpatients) ranged in age from younger than 1 day to 89 years (Table 1). Of the 817 inpatients, 773 were Haitian nationals, 26 were US military members, 15 were American civilians, and 3 were members of the Canadian Air Force. The 55 outpatients, defined by stays aboard the ship less than 24 hours, consisted of 21 Haitian nationals, 26 US military members, and 8 American civilians. As the Haitian age of emancipation is 16 years, pediatric patients were defined as being younger than or equal to 16 years of age. A total of 237 (27%) pediatric patients were treated. Adult inpatients totaled 605 (74%); 278 (46%) were males and 327 (54%) were females.
TABLE 1 Age Distribution of Patients Aboard the USNS Comfort, January 19-February 27, 2010a
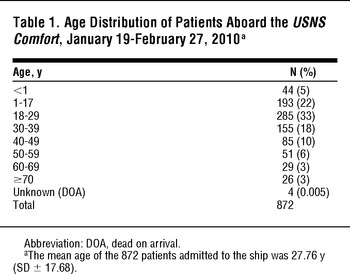
The 817 inpatients plus 185 escorts resulted in 1002 ward admissions; on day 10, the hospital's inpatient census reached a maximum of 411 inpatients and 102 patient escorts. The maximum number of patients admitted in a single day was 103 on January 21, the second full day of clinical operations. The 60-bed combined neonatal, pediatric, and adult intensive care unit (NICU/PICU/ICU) admitted a total of 186 patients during the 40 days (Figure 1) and did not necessarily reflect the full theoretical capacity of the ship, but the ship's capacity to provide safe and effective care given the available personnel and resources during the operation. Notably, the initial surge of patients reached the limit of staffing capabilities and led to fears of creating a substandard or even unsafe care environment. Subsequently, both rates of admission and levels of admitted patients' acuity were adjusted according to the on-board clinical capabilities. The average length of stay for all inpatients was 8.0 days; adult patients averaged 7.6 days, while pediatric patients averaged 9.1 days. The average length of stay for Haitian nationals was 8.8 days, with an average of 8.6 days for adults and 9.1 days for pediatric patients.
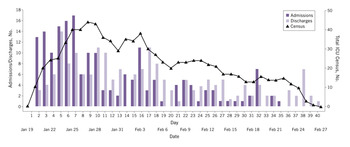
FIGURE 1 Intensive Care Unit (ICU) Admissions, Discharges, and Total Census Aboard the USNS Comfort, January 19-February 27, 2010.
Data represents total admissions to the combined neonatal ICU (NICU), pediatric ICU (PICU), and adult ICU. In total, 186 patients were admitted to intensive care.
The need for surgery was substantial: 454 patients went to the OR 843 times for a total of 927 procedures. Surgeries were divided into 7 categories: burns, craniotomy, extremity, head and neck, pelvis, spinal, and miscellaneous (Figure 2). Miscellaneous procedures included cesarean sections, exploratory laparotomies, sacral decubitus ulcer debridements, skin grafting, and other procedures that did not fall into the cited categories. Pediatric patients accounted for 25.7% of surgical procedures performed. Of the 669 extremity procedures, 122 were femur fracture repairs. Patients often had more than one major category of surgical injury; moreover, 161 (36.1%) required more than one trip to the OR (Table 2). The daily operative caseload peaked at 50 on January 28 (Figure 3). On average, 21.1 operations were performed daily.
TABLE 2 Total OR Visits per Patient Aboard the USNS Comfort, January 19-February 27, 2010
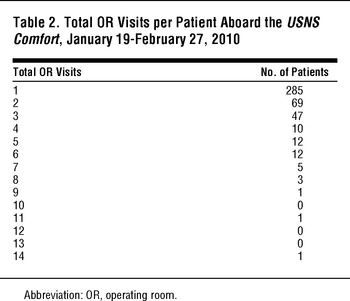
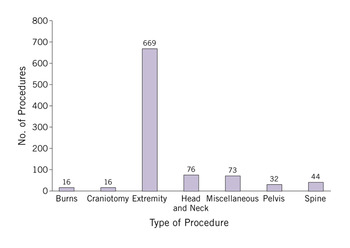
FIGURE 2 Breakdown of Surgical Procedures by Category Aboard the USNS Comfort, January 19-February 27, 2010.

FIGURE 3 Daily and Cumulative Operating Room (OR) Visits Aboard the USNS Comfort, January 19-February 27, 2010.
OR visits peaked at 50 on January 28, the Comfort's 10th day in port. In total, 454 patients received 843 operations, of which 927 were unique procedures.
Twenty-one patients arrived aboard the ship with previously performed amputations requiring revision and closure; 5 were upper extremity and 16 were lower extremity amputations. The ship's surgeons performed an additional 37 primary amputations on 5 upper and 32 lower extremities. A total of 105 amputation revisions were performed on these 58 patients during the first 30 days of surgery (Figure 4).
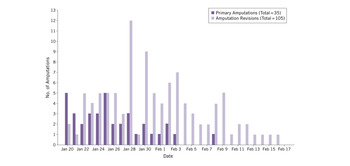
FIGURE 4 Primary and Revision Amputations Aboard the USNS Comfort, January 20-February 17, 2010.
In total, 35 primary and 105 revision amputations were performed; 21 patients who underwent amputation revision received the primary amputation before arrival to the ship.
Dialysis services were provided for 10 of 22 patients with renal insufficiency. Patients with oliguric renal failure were given priority for dialysis treatment. The most common indication for dialysis was hyperkalemia secondary to massive crush injuries. The 12 non-oliguric, hyperkalemic patients did not undergo dialysis; instead, their condition was stabilized with bicarbonate-based intravenous fluids, sodium polystyrene sulfonate, calcium chloride, insulin, and glucose.Reference Amundson, Dadekian and Etienne4 Of the 10 patients who received dialysis, 8 underwent only 1 treatment and 1 patient required 2 sessions. The tenth patient had a prior diagnosis of chronic renal insufficiency and received 14 treatments while waiting transfer to a shore facility. Three of the 10 patients who received dialysis therapy died of their diseases. The ship's dialysis services and the basis for these treatment decisions have been further described elsewhere.Reference Amundson, Dadekian and Etienne4
Blood products available aboard the ship included fresh packed red blood cells, frozen red blood cells, fresh frozen plasma, cryoprecipitate, and platelets. A total of 348 units of fresh red blood cells, 51 of frozen red blood cells, 16 units of fresh frozen plasma, 1 unit of cryoprecipitate, and 12 units of platelets were used during the mission.Reference Hussey, Dukette and Dunn5 The maximum amount of fresh red blood cells transfused in a single patient was 9 units. The maximum number transfused in a single day was 27 units on January 21, the second day of clinical work in Haiti.Reference Hussey, Dukette and Dunn5
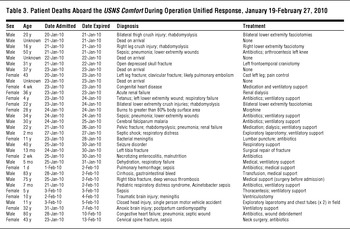
During the 40 days of clinical care, 33 deaths occurred. Four patients were dead on arrival to the ship. Of the remaining 29 who died, 13 (45%) were pediatric patients. There was a pathologist aboard the ship, but no autopsies were conducted. Cause of death was determined by clinical suspicion and patient history (Table 3).
TABLE 3 Patient Deaths Aboard the USNS Comfort During Operation Unified Response, January 19-February 27, 2010
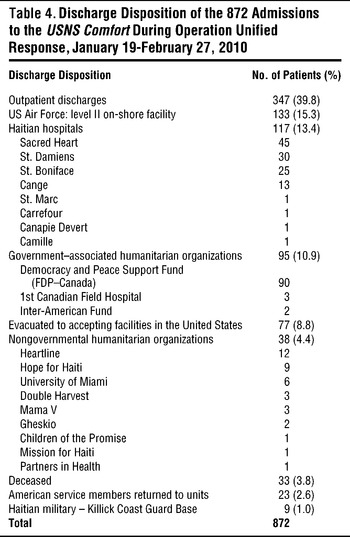
A team of discharge nursing coordinators conducted the disposition of patients once they were stable for discharge. Of 872 inpatients, 77 (9%) were transferred to accepting facilities in the United States via the National Disaster Medical System by representatives from US Health and Human Services. Haitian citizens constituted 69 of 77 (89.6%) evacuees to the United States, and they were cared for as part of the humanitarian effort. The other 8 patients were American citizens and service members. Haitians were evacuated to the United States only when the complexity of their injuries exceeded levels of care available both on board and ashore. Ten (14.5%) of these patients were aged 1 to 17 years, 33 (47.8%) were 18 to 29, 8 (11.6%) were 30 to 39, 10 (14.5%) were 40 to 49, 6 (8.7%) were 50 to 59, and 2 (2.9%) were 60 to 69. No evacuated patient was younger than 1 or older than 70 years. In terms of injuries as classified in the scheme described, 50% were extremity, 14.9% miscellaneous, 13.5% pelvis, 10.8% craniotomy, 5.4% spinal, 3.8% head and neck, and 1.3% burn. Of note, 9 patients sustained multiple injuries that fell into more than 1 category, and 4 patients' injuries were unrecorded. Of the inpatients who returned to Haiti, they were most commonly discharged to Port-au-Prince, with further treatment presumably rendered on an outpatient basis (n = 347). If continued care was required, patients were transferred to accepting facilities on shore (n = 448) (Table 4).
TABLE 4 Discharge Disposition of the 872 Admissions to the USNS Comfort During Operation Unified Response, January 19-February 27, 2010
COMMENT
The scope of the Haitian earthquake's destruction was essentially unprecedented in the recorded history of the Western Hemisphere. The most comparable disaster to which the US Navy had previously responded was the December 2004 Indonesian tsunami. However, the experience of Operation Unified Response dwarfed that of the previous mission. While the USNS Mercy admitted 176 patients and performed 193 surgical procedures in Indonesia,Reference Morrow and Llewellyn7 the USNS Comfort admitted 872 patients and performed 927 procedures in Haiti. This difference was mainly attributable to 2 factors. First, the Comfort arrived in Port-au-Prince comparatively soon after the event: almost exactly 1 week later. The Mercy arrived in Banda Aceh, Indonesia, more than 5 weeks after the tsunami.Reference Morrow and Llewellyn7 This dramatic difference is attributable to both Haiti's geographic proximity and the rapid decision to deploy the ship. Second, Haiti's already fragile health care infrastructure was almost completely devastated by the earthquake; as a comparatively developed nation, Indonesia was better equipped to provide its own health care response.Reference Joyce8
These factors combined to place the Comfort in an unprecedented role in disaster relief: a foreign tertiary trauma center. This function was primarily due to the ship's controlled on-board surgical environment, an invaluable resource, particularly in the disaster's early phase. The ship's function in this regard is most readily demonstrated by the high percentage of surgical admissions, 52.1%, and the fact that 32.1% of amputees were transferred from outside facilities. This experience contrasts with the prior disaster literature: successes of foreign medical teams (FMTs) responding to disasters are typically questionable, particularly with regard to surgical care.Reference Kirsch9Reference Redmond, O’Dempsey and Taithe10Reference Abolghasemi, Radfar, Khatami, Nia, Amid and Briggs11 The lack of surgical impact is due largely to the delayed response time inherent to a foreign relief mission: by the time the team mobilizes, travels, and arrives, those requiring surgical intervention have either died or received their operation from domestic surgeons.Reference Joyce8Reference Kirsch9Reference Abolghasemi, Radfar, Khatami, Nia, Amid and Briggs11 Therefore, FMTs typically provide more effective and efficient relief by focusing on caring for uninjured survivors through provision of supplies and prevention of communicable disease.Reference Joyce8Reference Kirsch9Reference Abolghasemi, Radfar, Khatami, Nia, Amid and Briggs11Reference Krin, Giannou and Seppelt12
While the Comfort's response was by no means rapid when judged on the typical time-scale for injury response, it found itself thrust into a role as a trauma referral center essentially immediately on its arrival. This role existed for 3 reasons. First, in spite of the regrettable certainty that the vast majority of untreated severely injured patients had died by the time the ship arrived, the magnitude of the disaster was such that an overwhelming number of these patients survived that week even without intervention. Second, as mentioned, Haiti had minimal capacity to provide its own care. Third, a number of nongovernmental humanitarian organizations (NGOs) provided trauma support in the acute phase,Reference Auerbach, Norris and Menon13Reference Ginzburg, O’Neill, Goldschmidt-Clermont, de Marchena, Pust and Green14Reference Jaffer, Campo and Gaski15Reference McIntyre, Hughes and Pauyo16 but overwhelmed resources and uncontrolled field hospital environments limited the care they were able to provide. Thus, many of their temporized patients were awaiting definitive management when the USNS Comfort arrived.Reference Auerbach, Norris and Menon13Reference Jaffer, Campo and Gaski15Reference McIntyre, Hughes and Pauyo16
Transfer of patients began immediately. The ship anchored in Port-au-Prince harbor, as the earthquake had destroyed the pier. The majority of patients were transferred by helicopter. Patient collection points (PCPs) were established at helicopter LZs, and RAT personnel triaged patients at these locations. As previously stated, 2 combat-experienced trauma surgeons performed initial triage; their goal was to maximize the number of patients receiving the Comfort 's level of care by identifying appropriate patients and transporting them as quickly as possible. In the first 7 days after the ship's arrival, numerous critically injured and ill patients were brought to the LZs. Those with earthquake-related injuries and illnesses considered threatening to life, limb, and eyesight were given priority. Initially, the walking wounded and those triaged as expectant were not transported. The unfortunate reality in a disaster of this magnitude is that not every patient who presented to the LZs could have or should have been transferred. This situation required many difficult decisions to be made on a daily basis. The expertise required, as well as the physical and emotional demands on the RAT, were extensive; these ethical dilemmas have been examined elsewhere.Reference Etienne, Powell and Amundson17 Nevertheless, we strongly believe that by positioning the most experienced surgeons in triage, we responded to the disaster most effectively. Once patients arrived on board, they were brought to CASREC, reassessed, and dispositioned; additional surgeons were present to determine which patients required immediate operative intervention. This system allowed the ship's resources to be expeditiously allocated to the patients who could benefit most from its care.
The survivor and transfer bias led to a marked preponderance of orthopedic injuries among patients transferred to the Comfort: in the first 48 hours, 85% of triaged injuries involved orthopedic trauma; moreover, 669 of the mission's 927 procedures (72.2%) were performed on extremities. Admittedly, while a prevalence of orthopedic injuries had been anticipated, the Comfort was initially unprepared for this dramatic predominance. The ship had been augmented with surgical subspecialists including 3 general surgeons, a pediatric surgeon, a urologist, an obstetrician and gynecologist, a plastic surgeon, an otolaryngologist, an ophthalmologist, and 2 neurosurgeons, but only 1 orthopedic surgeon. To fill this void, 5 military orthopedic surgeons were deployed to the Comfort by day 4; moreover, an additional 8 civilian orthopedic surgeons volunteered and arrived by day 10.
Once patients were admitted to the ship, our on-board treatment strategy was developed through an attempt to balance the ethics of disaster response,Reference Etienne, Powell and Amundson17 sound medical practice, and appropriate humanitarian intervention. Our data reflect this.
Ethical considerations were manifest not only in our described triage system, but also in imperatives to both value life over limb and provide the greatest good to the greatest number of patients. In spite of the magnitude of the disaster, with more than 230 000 people killed and countless severely injured, a minority of our cohort (21.3%) required intensive care. Moreover, despite the crush mechanism of earthquake injury, only 21 of Comfort 's patients were diagnosed with crush syndrome; 12 of those patients were managed successfully without dialysis. In addition, this traumatically injured population received relatively few transfusions. On average, patients received 0.49 units of blood product through transfusion, and the most aggressively treated patient received only 9 units. Most strikingly and importantly, only 33 of 872 patients died, a mortality rate of 3.8%. For the most part, these were the most severely injured patients transferred to the Comfort; this low percentage reinforces their treatment as the exception rather than the rule. The survivor bias consequent to the Comfort's arrival 7 days after the earthquake contributed to this relatively stable population, but, as mentioned, an overwhelming number of severely injured patients remained in Haiti when the Comfort anchored. Regrettably, acceptance of a large proportion of these patients would have dramatically limited our capacity to provide care.
Our desire to care for as many patients as possible was also countered by the medical necessity of repeated debridement. All soft tissue wounds were at least a week old. Many had gone untreated. Consequently, all were grossly infected. Extremities amputated either onshore or on board were grossly purulent at initial intervention. Many patients with sepsis required life-saving “guillotine” amputations. These stumps and wounds required repeated debridement every 48 hours, and, often, proximal amputation revision before closure or skin grafting. Performing both 105 amputation revisions on 58 amputees and more than 1 procedure on 36.1% of the surgical population reflected this strategy.
Whenever appropriate, we chose to meet but not exceed the standard of care available in Haiti before the earthquake.Reference Etienne, Powell and Amundson17 Much has been written regarding the importance of this measure.Reference Abolghasemi, Radfar, Khatami, Nia, Amid and Briggs11Reference Welling, Ryan, Burris and Rich18 For example, when choosing between treatment options, the plan that could receive reliable follow-up in the Haitian medical system was selected. This decision was manifest in our preference for plain gauze dressings over vacuum-assisted closure devices. Moreover, plaster casts were used instead of fiberglass to allow removal by water soaking, as cast saws were not readily available on the island. Also, we endeavored to avoid breaking up families by admitting 185 surviving relatives to the ship as escorts. However, as manifested by the fact that only roughly 21% of patients were admitted with an escort, this proved formidable; we can only acknowledge that we were not successful in every instance. Numerous factors influenced this rate, including the onshore chaos, the ship's capacity to house additional civilians, and a lack of surviving family members. Nonetheless, the challenging necessity of providing either ship-to-shore patient-family communication or on-board escort housing remained a significant lesson of the operation, and was an obvious area for the improvement of future missions.
The decision to withdraw the Comfort was made at the levels of the Pentagon and the White House. In preparation for withdrawal, rates of admissions were decreased and eventually ceased, and disposition of inpatients was coordinated. At the time of discharge, each patient was given a full course of medications and provided with written documentation of hospitalization and treatment. Patient transfer was accomplished by boat and helicopter. Transfers required coordination not only with the MOH, but also Haitian and NGO treatment facilities for those needing continued inpatient care, as well as ground transportation services for those returning to private residences. The essential interagency cooperation was most evident in disposition of the Comfort 's patients, 250 (28.7%) of whom were discharged either directly to the care of a humanitarian organization or to a Haitian hospital facilitated with the help of a humanitarian organization. Patients were discharged from the ship only after they were deemed appropriate for accepting facilities. To ensure that the proper levels of care were available, we visited unknown facilities before patient transfer occurred.
The multi-agency cooperation evident in patient transfer, reinforcement of the Comfort's staffing, and discharge of patients from the ship was unique and extraordinary. Previous reports have criticized the lack of cooperation between NGOs and the military during humanitarian medical missions.Reference Joyce8Reference Welling, Ryan, Burris and Rich18 Perhaps this is understandable: military responses are inexorably linked to political motivations in spite of the best intentions of the responders, while NGOs espouse humanitarian impartiality.Reference Joyce8 While the Navy attempted to partner with NGOs during its mission to Indonesia,Reference Morrow and Llewellyn7 the results were mixed.Reference Joyce8 However, in this instance, having been involved at the request of the Haitian government, the military was able to serve a complementary role, providing both ground security and a tertiary trauma center for NGOs,Reference Auerbach, Norris and Menon13 while NGOs stabilized patients in the disaster's aftermath, facilitated discharge of patients from the ship, and, in many instances, completed patients' treatment courses.
CONCLUSIONS
The magnitude of this disaster was epic. The near total decimation of Haiti's limited health care resources led to almost complete reliance on FMTs for trauma care, even weeks after the earthquake. The USNS Comfort's service as a tertiary trauma facility in this unprecedented situation was directly analogous to the ship's intended function: support of battlefield casualties. It is difficult to present our experience as a model; it is hoped that the set of circumstances that allowed the ship to function in its natural role will remain unique. Moreover, while the US government has not released the mission's specific costs, the resources available to the ship are extraordinary. Nonetheless, the cooperation demonstrated between the US military and the NGOs in support of the Haitian MOH is evidence not only of the adaptability of these groups but also the remarkable synergy of their respective resources. In this instance, both philosophies had much to offer and much to gain from the others' assistance. This successful mutual collaboration should remain a mainstay of future humanitarian response, irrespective of a disaster's locale or scale.










