Introduction
The survival rate of patients who have underwent out-of-hospital cardiac arrest (OHCA) has been increasing, and bystander intervention has been indicated as one of the main contributors to this improvement.Reference Hasselqvist-Ax, Riva and Herlitz 1 In Japan, approximately 120,000 individuals are transported to hospitals annually after OHCA, 2 and it has been reported that the number of cases receiving bystander cardiopulmonary resuscitation (CPR) has increased.Reference Kitamura, Kiyohara and Sakai 3
While CPR plays a central role in maintaining perfusion to the brain and coronary arteries during cardiac arrest, it can potentially have adverse effects such as iatrogenic chest injuries related to chest compressions or ventilator support.Reference Black, Busuttil and Robertson 4 Efficient CPR requires hard and fast chest compressions with minimum interruption,Reference Kleinman, Brennan and Goldberger 5 and it is reported that chest injuries due to chest compressions occur rarely if compressions are performed employing an appropriate position and strength.Reference Seiro, Takafumi, Yasuhiro, Jun, Hideki and Hirohisa 6 However, most bystanders at the scene are laypersons, not health care providers, and it is very difficult to maintain high-quality CPR in out-of-hospital settings due to the lack of standardized conditions. Furthermore, although CPR is continued during transportation to a hospital by paramedics, the quality of CPR in an ambulance has been reported as unstable because of car swaying, limited number of paramedical staff, and limited activity space.Reference Katoh, Sugimoto, Yasuda, Tanaka, Kumagawa and Tsunoda 7 Therefore, out-of-hospital CPR itself has been hypothesized to carry independent risk for adverse effects.
To the author’s knowledge, there have been few reports to date that have focused on out-of-hospital CPR separately and evaluated the association between out-of-hospital CPR and the risk of adverse events. In this study, the authors assessed the risk of out-of-hospital CPR for chest injuries in patients with OHCA.
Methods
Study Design and Setting
This retrospective, observational study to evaluate the association between CPR performed in out-of-hospital settings and the incidence of chest injuries was conducted in an emergency department of a rural tertiary emergency critical care medical center. Since there are few emergency hospitals in the region, it typically takes longer to transport patients to this hospital compared to previously reported times in urban areas.Reference Masterson, Wright and O’Donnell 8 In Japan, paramedics are not permitted to terminate resuscitation in the field; therefore, OHCA cases requiring long transportation times can occur in rural regions. Within the study period, out-of-hospital CPR by paramedics for all included patients was based on Japanese CPR guidelines, and in-hospital CPR for all included patients was performed in accordance with the 2010 American Heart Association (AHA; Dallas, Texas USA) Guidelines for CPR and Emergency Cardiovascular Care (ECC).
This study complied with the principles laid down in the 1964 Helsinki Declaration and its later amendments or comparable ethical standard. The ethics committee of the Matsudo City Hospital (Matsudo City, Chiba, Japan) approved this study (#28-14).
Study Populations
Consecutive OHCA patients who were transferred to Matsudo City Hospital from April 2013 through August 2016 were included. Patients less than 18 years old, with cardiac arrest due to trauma, who received open-chest CPR, and who received CPR using an automated chest compressions device (only three patients) were excluded, because the aim of this study was to evaluate the instability of out-of-hospital CPR performed by bystanders or paramedics. The authors also excluded patients whose CPR duration was not recorded or who did not undergo chest computed tomography (CT) examination.
Data Collection
Data were collected by trained medical doctors, and a standard abstraction form was used to ensure uniform data handling. Collected data were monitored, and suspected outliers were confirmed or corrected by other chart abstractors. The following data were collected retrospectively from medical records including emergency department records, paramedic reports, inpatient charts, nursing notes, and other clinical records. The following data were collected retrospectively from medical records: age, sex, presence or absence of a witness of the cardiac arrest, presence or absence of bystander CPR before paramedics’ arrival at the scene, whether or not return of spontaneous circulation (ROSC) was achieved, in-hospital CPR duration, out-of-hospital CPR duration, and status at hospital discharge (ie, survived or deceased). The authors also collected data regarding the incidence of rib or sternal fractures and pneumothoraces caused by CPR from medical records and chest CT findings. Chest injuries related to CPR were assessed by findings of 64-slice CT scans. Chest CT examination was performed as a part of clinical practice for OHCA patients whenever the cause of cardiac arrest was not clearly diagnosed, according to the standard operating procedure of the study hospitals. Radiological findings were interpreted by at least two board-certified emergency physicians. Short periods of transient ROSC were included in total CPR duration in this study.
Definitions and Outcome Measures
Patients were defined as patients in OHCA who were unresponsive, with no breathing or only gasping, and whose carotid arteries were not palpable within 10 seconds, as previously described.Reference Kleinman, Brennan and Goldberger 5 The study outcome was defined by the composite of rib fractures, sternal fractures, and pneumothoraces related to CPR.
Statistical Analysis
Data were presented as counts and percentages for categorical variables and as means (standard deviation) for numeric variables. The authors used a univariate analysis to identify the factors associated with chest injuries. The continuous variables were compared using Student’s t-test or Mann-Whitney U test, and categorical variables were compared using the χ2 test or Fisher’s exact test. A multivariate logistic regression analysis was also performed to assess the independent risk factors for chest injuries related to CPR and their adjusted odds ratios and 95% confidence intervals. The variables incorporated into the multivariate model were determined by the results of univariate analysis (cut-off: P value<.1), previous reports,Reference Black, Busuttil and Robertson 4 , Reference Seung, You, Lee, Park, Chung and Park 9 and clinical relevance. The adjusted odds ratios for the incidence of chest injuries were assessed in patients stratified by out-of-hospital CPR duration to evaluate the point of increased injury risk.
All statistical analyses were performed with EZR for Windows (Saitama Medical Center, Jichi Medical University; Saitama, Japan), a modified version of R Commander designed to add statistical functions frequently used in biostatistics. Two-sided P values<.05 were considered statistically significant.
Results
The patient flow diagram is shown in Figure 1. A total of 727 OHCA patients were identified during the study period, of whom 255 patients were excluded according to the exclusion criteria, and the remaining 472 patients were analyzed. Among those 472 patients, chest injuries caused by CPR were identified in 233 patients (49.4%). The details of chest injuries are shown in Supplemental Figure 1 (available online only). The most frequent chest injury caused by CPR was isolated rib fractures, followed by pneumothoraces with rib fractures.
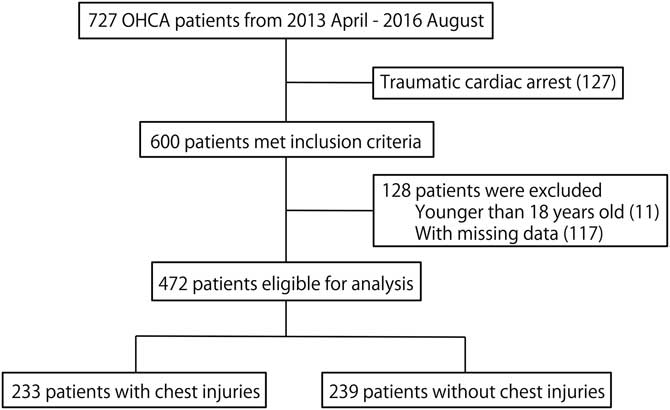
Figure 1 Flow Diagram of Patient Selection. Abbreviation: OHCA, out-of-hospital cardiac arrest.
The baseline characteristics of patients stratified by the presence or absence of chest injuries caused by CPR are shown in Table 1. Patients in the chest injury group were older than those without chest injury [mean=77.6 years (SD=11.3) versus 66.4 years (SD=16.5); P<.001]. There was no statistically significant difference between men and women (P=.092). Both ROSC and survival to hospital discharge were observed less frequently in patients with chest injuries [ROSC: 76 patients (31.5%) versus 128 patients (55.4%); P<.001; and survival to hospital discharge: 10 patients (4.2%) versus 30 patients (13.0%); P=.003].
Table 1 Baseline Characteristics
Abbreviations: CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
The results of univariate analysis are shown in Table 2. Significant differences were observed only in age and out-of-hospital CPR duration. In addition to these variables, variables of sex and in-hospital CPR duration, of which P values were less than .1, were included in the subsequent multivariate logistic regression model. Furthermore, the variable of presence/absence of bystander CPR was also incorporated into the model because of the importance from clinical perspective. As the result, age and out-of-hospital CPR duration were identified as independent risk factors for chest injuries related to CPR, and in-hospital CPR duration was not a statistically significant independent risk factor (Table 3).
Table 2 Univariate Logistic Models for the Relation to Thoracic Injuries

Abbreviation: CPR, cardiopulmonary resuscitation.
Table 3 Multivariate Logistic Analysis for the Relation to Thoracic Injuries

Abbreviation: CPR, cardiopulmonary resuscitation.
Figure 2 shows the relationship between the cumulative number of patients with chest injuries and out-of-hospital CPR duration. The number of cases with chest injuries increased steadily with increasing duration of out-of-hospital CPR. The odds ratios for the incidence of chest injuries stratified by 5-minute increments of out-of-hospital CPR are shown in Figure 3. When the duration of out-of-hospital CPR exceeded 15 minutes, the likelihood of chest injuries was increased, though this change was not statistically significant [adjusted odds ratio=1.81 (95% CI, 0.84 to 3.93)].

Figure 2 The Association between the Cumulative Number of Patients with Chest Injuries and Out-of-Hospital CPR Duration. Abbreviation: CPR, cardiopulmonary resuscitation.

Figure 3 The Odds Ratios for the Incidence of Chest Injuries Stratified by 5-Minute Increments of the Duration of Out-of-Hospital CPR. Abbreviation: CPR, cardiopulmonary resuscitation.
Discussion
The guidelines of the AHA and ECC emphasize the importance of high-quality CPR,Reference Seung, You, Lee, Park, Chung and Park 9 and it is reported that chest injuries due to chest compressions occur rarely if they are performed employing the correct position and strength.Reference Seiro, Takafumi, Yasuhiro, Jun, Hideki and Hirohisa 6 However, there have been reports of serious complications due to chest compressions,Reference Hickey, Gill, Seidman and Webber 10 - Reference Dupont, Rougé-Maillart, Gaudin, Jeanneteau, Jousset and Malbranque 13 and the number of such adverse events was reported to increase after the publication of the 2010 AHA guidelines. Because CPR in out-of-hospital setting is often performed in confusing situations, the authors hypothesized that out-of-hospital CPR is an independent risk factor for chest injuries. In this study, the authors retrospectively evaluated the risk of chest injuries caused by CPR in 472 OHCA patients.
In this study, the duration of CPR performed in out-of-hospital settings and in-hospital settings were analyzed separately. In the multivariate model, only age and out-of-hospital CPR duration were found to be independent risk factors for the chest injuries caused by CPR. Although there has been a report describing total CPR duration as the risk for chest injuries,Reference Kashiwagi, Sasakawa and Tampo 14 the result of this study, for the first time, showed that out-of-hospital CPR duration, not in-hospital CPR duration, is an independent risk factor of chest injuries related to CPR. Age is the previously identified risk factor,Reference Black, Busuttil and Robertson 4 , Reference Seung, You, Lee, Park, Chung and Park 9 , Reference Kashiwagi, Sasakawa and Tampo 14 and the impact of age can be explained by the bone weakening due to the aging. Sex and the presence or absence of a bystander CPR before Emergency Medical Service arrival at the scene were not the statistically independent risk factor.
In out-of-hospital settings, the majority of initial CPR providers are laypersons, not health care providers, who typically lack sufficient knowledge of CPR. It has been also reported that the actual time of chest compressions in out-of-hospital settings (including inside an ambulance) is less than half of the total out-of-hospital CPR duration, suggesting the unreliability of CPR quality provided in out-of-hospital settings.Reference Wik, Kramer-Johansen and Myklebust 15 A previous study in Japan14 reported that rib fractures and pneumothoraces after CPR were observed more frequently in the right side compared to left side. Because of the structure of Japanese ambulances, Japanese paramedics always perform CPR on the right side of a patient during transport. These structural characteristics of ambulances are considered as the reason for the laterality of chest injuries, and it also suggested that the CPR quality performed in an ambulance is unstable. On the basis of these evidence and the present study, which indicated the duration of out-of-hospital CPR as an independent risk factor for chest injuries, it may be feasible to utilize a device such as an automated chest compressor to overcome such unstable conditions during transport in cases requiring long transportation times.
The use of automated chest compressors has been reported as non-inferior to manual chest compressions for survival to emergency department discharge, survival to hospital discharge, and neurological outcome in OHCA patients.Reference Bonnes, Brouwer and Navarese 16 The in-hospital survival rate of patients who undergo CPR with an automated chest compressor was also reported as non-inferior to that of patients who receive manual chest compressions for in-hospital cardiopulmonary arrest.Reference Couper, Yeung, Nicholson, Quinn, Lall and Perkins 17 The consistent CPR quality provided by an automated chest compressor may be useful for OHCA patients requiring long transportation times. However, the use of automated chest compressors has also been associated with a risk of rib and sternal fractures.Reference Lardi, Egger, Larribau, Niquille, Mangin and Fracasso 18 - Reference Koga, Fujita and Yagi 20 Further large-scale studies are required to assess the efficacy and safety of automated chest compressor use in out-of-hospital settings.
The definition of “long transportation time” should also be discussed. In this study, the odds ratios for the incidence of chest injuries in patients stratified by 5-minute increments of out-of-hospital CPR duration were calculated and suggested that 15 minutes was a candidate for the threshold defining a long transportation time, after which the risk for the chest injuries caused by out-of-hospital CPR increases. The odds ratios and associated confidence intervals did not significantly differ, possibly due to the limited sample size; however, the employed cut-off value of 15 minutes appears to be pragmatic from a clinical perspective.
In this study, fewer patients with chest injuries achieved ROSC. It was unclear whether the incidence of chest injuries was a cause or a consequence of the lower rate of ROSC; however, the failure of thoracic compliance could be a reason for insufficient chest compressions. Because circulation during CPR is achieved by the positive and negative pressure obtained by chest compressions, patients with rib fractures or massive pneumothoraces cannot maintain sufficient circulation, which may be one of the reasons for their lower rate of ROSC. Considering the increasing incidence of CPR in unstable out-of-hospital settings, some measures are required to provide adequate quality of CPR and to avoid chest injuries. Utilization of an automated chest compressor is considered as one of the alternative means for further improvement in quality of out-of-hospital CPR.
Limitations
This study has several limitations. First, it is a single-center, retrospective study with a limited sample size. Second, the authors could not identify the occupation of the bystanders, such as whether they had medical training or were laypeople. Third, because CPR-related injuries were assessed based on the findings of CT without the use of a contrast agent, abdominal solid organ injuries could not be assessed. Despite these limitations, the author’s results indicated the significant risk of out-of-hospital CPR duration for chest injuries, and the authors proposed a cut-off point of CPR duration in out-of-hospital settings at which the risk for chest injuries increased. Further prospective studies evaluating the efficacy of alternative chest compressions methods, such as automated chest compressors, are warranted in cases involving long transportation times.
Conclusion
The results of this single-center, retrospective, observational study demonstrated that age and out-of-hospital CPR duration, not in-hospital CPR duration, were independent risk factors for chest injuries caused by CPR. Further studies to assess the efficacy of alternative CPR devices, such as automated chest compressors, are warranted in cases requiring long transportation times.
Acknowledgments
The authors thank all included patients and their families, physicians, nurses, paramedics, and all staff for performing CPR and for their assistance in data acquisition. In addition, the authors thank Dr. Atsushi Senda, Dr. Nao Urushibata, Dr. Junichi Aiboshi, Dr. Kiyoshi Murata, Dr. Kenichi Hondo, and Dr. Shunske Yoshikawa for direct patient care and their review and feedback for the author’s manuscript.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X18000201








