INTRODUCTION
Motor neuron diseases (MND), including amyotrophic lateral sclerosis (ALS), are characterized by a progressive degeneration of upper and lower motor neurons. Depending on the location of the degeneration in ALS, it gives rise to progressive symptoms such as weakness, spasticity and hyperreflexia, speech and swallowing problems, muscular atrophy, wasting, fasciculation, and hyporeflexia (Winhammar et al., Reference Winhammar, Rowe and Henderson2005). The survival time from the first symptoms is a few years (Worms, Reference Worms2001; Forbes et al., Reference Forbes, Colville and Cran2004), but about 10% survive 5 years or more (Forbes et al., Reference Forbes, Colville and Cran2004). The most common cause of death is respiratory failure (Neudert et al., Reference Neudert, Oliver and Wasner2001a; Winhammar et al., Reference Winhammar, Rowe and Henderson2005) with a peaceful and not a choking death (Neudert et al., Reference Neudert, Oliver and Wasner2001a). ALS is an incurable disease that can cause both physical damage and psychosocial problems. Palliative care and support with a focus on the families' specific needs and wishes are needed from the time of the diagnosis throughout the course of the disease.
Most measurements of patients' quality of life (QoL), anxiety, and depression are made at one single examination, and results have been found to vary. This may depend on the use of different methods and instruments (Bromberg & Forshew, Reference Bromberg and Forshew2002; Chio et al., Reference Chio, Gauthier and Montuschi2004; Bungener et al., Reference Bungener, Piquard and Pradat2005; Wicks et al., Reference Wicks, Abrahams and Masi2007). It has been reported that patients' health-related quality of life (HRQoL) deteriorates whereas individual QoL is fairly constant over time (Neudert et al., Reference Neudert, Wasner and Borasio2004). The Physical Component Summary (PCS) was found to decrease over time whereas the Mental Component Summary (MCS) in SF-36 did not (Norquist et al., Reference Norquist, Jenkinson and Fitzpatrick2003; De Groot et al., Reference De Groot, Post and van Heuveln2007). Most patients have no or a low level of anxiety or depression at one single examination (Bungener et al., Reference Bungener, Piquard and Pradat2005; Wicks et al., Reference Wicks, Abrahams and Masi2007) and over time (Rabkin et al., Reference Rabkin, Albert and Del Bene2005; Gauthier et al., Reference Gauthier, Vignola and Calvo2007). It has been suggested that individual QoL, MCS in SF-36, anxiety, and depression do not interrelate with physical function (Norquist et al., Reference Norquist, Jenkinson and Fitzpatrick2003; Neudert et al., Reference Neudert, Wasner and Borasio2004; De Groot et al., Reference De Groot, Post and van Heuveln2007; Krampe et al., Reference Krampe, Bartels and Victorson2008; Vignola et al., Reference Vignola, Guzzo and Calvo2008) whereas PCS in SF-36 does (Norquist et al., Reference Norquist, Jenkinson and Fitzpatrick2003; De Groot et al., Reference De Groot, Post and van Heuveln2007).
QoL has been claimed to be moderately high and the level of depression low in both patients and caregivers (Trail et al., Reference Trail, Nelson and Van2003), but it also has been shown that patients have better individual QoL (Bromberg & Forshew, Reference Bromberg and Forshew2002). Patients' QoL and depression have been found to be relatively constant whereas their caregivers have shown an increase in depression and burden (Gauthier et al., Reference Gauthier, Vignola and Calvo2007). In contrast to those results, it has been reported that spouse carers do not have increased anxiety and depression but do show an increase in psychological distress over time (Goldstein et al., Reference Goldstein, Atkins and Landau2006).
A diagnosis of ALS emotionally affects both the patient and the next of kin. To increase our understanding of the physical and emotional consequences that the disease might have, both the patient and the next of kin must be studied in terms of health-related and individual QoL and the possible presence of anxiety and depression. It may be possible to gain a broader perspective of the QoL in patients with ALS and their next of kin if matched pairs and not only groups of patients/next of kin are studied over time with different QoL instruments. The aim of this study was to examine HRQoL, individual QoL, and self-estimates of anxiety and depression in patients with ALS and their next of kin in relation to patients' physical function over time.
METHODS
Participants and Demographics
Patients with probable or definite ALS according to the El Escorial criteria (Brooks, Reference Brooks1994) who were under treatment by the ALS/MND team at Sahlgrenska University Hospital from January 2006 onward were asked to participate in the study. Patients or next of kin who were in such physical or psychological condition that they were not able to give informed consent and patients who were in a terminal stage of the disease were excluded.
Forty-seven consecutive patients were eligible for inclusion in the study. One man was excluded because of poor performance in the Swedish language and four men and one woman did not wish to participate. Because of the focus on patients versus next of kin, only patients with a next of kin were included, which excluded a further six patients. One of these six patients was also excluded because of a cognitive impairment. The final number was 35 patients and 35 next of kin at the start of the study. At entry to the study, the mean age of the patients was 63.4 years (median 64 years, range 28–84 years) and of their next of kin 61.3 years (median 64.5 years, range 27–86 years).
All patients lived at home during the study. Next of kin was defined as a person closely related with a near contact to the patient. This term was found to be suitable, because not all of them assisted the patients in their daily life. Thirty of the next of kin were married or cohabited with the patient, three were children, one was a sister, and one had previously been married to the patient.
Instruments
Patients and their next of kin estimated their HRQoL by the Short Form-36 Health Survey (SF-36; Sullivan et al., Reference Sullivan, Karlsson and Ware1995), their individual QoL by the Schedule for Evaluation of Individual Quality of Life-Direct Weighting (SEIQoL-DW; Hickey et al., Reference Hickey, Bury and O'Boyle1996), and their experience of anxiety and depression by the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, Reference Zigmond and Snaith1983). The patients' physical function was estimated by two physical functional scales, the Amyotrophic Lateral Sclerosis Functional Rating Scale-Revised (ALSFRS-R; Cedarbaum et al., Reference Cedarbaum, Stambler and Malta1999) and the Norris scale (Norris et al., Reference Norris, Calanchini and Fallat1974). At entry to the study, the patients were evaluated by the Mini-Mental State Examination (MMSE; Myers, Reference Myers1987) to exclude major signs of cognitive impairment.
The SF-36 includes 35 items divided into eight multi-item scales, physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH), and one single item reporting health transition over the past year (Sullivan et al., Reference Sullivan, Karlsson and Ware1995; Sullivan & Karlsson, Reference Sullivan and Karlsson1998). These eight scales are divided into two major dimensions of health: the Physical Component Summary (PCS) and the Mental Component Summary (MCS; Persson et al., Reference Persson, Karlsson and Bengtsson1998). Higher scores reflect better QoL (Sullivan et al., Reference Sullivan, Karlsson and Ware1995).
The SEIQoL-DW is a semistructured interview in which the person nominates the five most important areas of life. Functioning/satisfaction in each area are then rated on a visual analogue scale where 0 is “as bad as can be” and 100 is “as good as can be.” The importance of the five areas is then weighted against each other. The person's self-rating of functioning/satisfaction in each area is subsequently multiplied by the corresponding area weight. This gives five products that are summarized to obtain a global quality of life score that ranges from 0 to 100. Higher scores reflect better QoL (Hickey et al., Reference Hickey, Bury and O'Boyle1996; Neudert et al., Reference Neudert, Wasner and Borasio2001b).
The HADS estimates anxiety (HADa) and depression (HADd) in two subscales with seven items each. The subscales are rated on 4-point scales (0–3). A score of 7 or less indicates no case of anxiety or depression, 8–10 points indicate doubtful cases and scores over 11 indicate definite cases. Higher scores reflect poorer ratings (Zigmond & Snaith, Reference Zigmond and Snaith1983).
The physical function of patients was rated by the ALSFRS-R (Cedarbaum et al., Reference Cedarbaum, Stambler and Malta1999) and the Norris scale (Norris et al., Reference Norris, Calanchini and Fallat1974). ALSFRS-R measures gross and fine motor tasks and bulbar and respiratory functions. The scores range from 0 to 40, where 40 is normal functioning (Cedarbaum et al., Reference Cedarbaum, Stambler and Malta1999). The Norris scale is a 100-point scale where higher levels indicate better function. It measures bulbar, respiratory, trunk, arm, leg, and general domains, reflexes, fasciculation, and muscle atrophy (Norris et al., Reference Norris, Calanchini and Fallat1974; Winhammar et al., Reference Winhammar, Rowe and Henderson2005). Both scales were used because they partly rate some different items of physical function. In the same study group, Olsson et al. (in press) reported decreased physical function over time in the ratings by ALSFRS-R and the Norris scale (Table 1).
Table 1. Changes over time in patients and their next of kin.
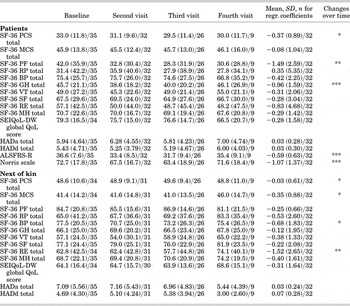
Mean (±standard deviation)/number of patients/next of kin at every visit and for the regression coefficients. P levels in the table indicate deterioration over time from baseline to the last visit for each patient/next of kin.
*significant time effect p < .05, **significant time effect p < .01, ***significant time effect p < .001.
Procedure
Patients and their next of kin were consecutively included in the study from January 2006. The study ended in December 2007. Patients were examined every fourth to sixth month, with an ambition of six months, one to four times, by the ALS/MND team at the Department of Neurology, Sahlgrenska University Hospital. The SF-36 and HADS forms were sent home to the participants, who were requested to complete the questionnaires on their own before the following visit to the physician. The physician examined the patients using the ALSFRS-R and Norris scales. The patients and next of kin were then seated in separate rooms and interviewed by the research nurses with the SEIQoL-DW. At entry to the study, one research nurse tested all patients with the MMSE.
Analysis
Data were paired and two-tailed tested. A level of p < .05 was considered significant.
To avoid an erroneous interpretation of multiple testing of changes over time in the instruments, a regression coefficient was calculated for each patient and next of kin. The coefficient describes the slope of the graph, where x-values are the time of the visits (at 0, 6, 12, and 18 months) and y-values are the variables investigated. A regression calculation was made for every patient/next of kin with more than one visit, and every regression coefficient was given an equal weight regardless of whether the participant attended the study sessions two, three, or four times. The participants who were used to calculate the regression coefficients were taken from those who still remained in the study at Visit 2 and onward. Using the slopes/coefficients, Fisher's test for paired comparison was employed to test whether the coefficient was different from 0, that is, whether there was a change over time.
Paired comparisons between patients and their next of kin were analyzed with the Wilcoxon Signed Ranks Test. The Mann–Whitney test was used to analyze differences between genders. Correlations between the physical functional scales and SF-36, SEIQoL-DW, and HADS were analyzed by Spearman's rho.
Ethics Approval
Ethical approval was obtained from the Regional Ethical Review Board in Gothenburg, approval No. 297-05.
RESULTS
Changes over Time in SF-36, SEIQoL-DW, and HADS
Among patients, changes were found over time in the subscales PCS, PF, and GH in SF-36. Next of kin had changes over time in the subscales MCS, PF, BP, and RE. The global QoL score in SEIQoL-DW and the HADS showed no changes over time in either the patients or their next of kin (Table 1). There were no differences with respect to gender.
Comparisons between Patients and Their Next of Kin
At Visit 1, patients estimated poorer PCS, physical functioning, role physical, and general health (p < .003) in SF-36 than did the next of kin. The next of kin had a poorer global QoL score in SEIQoL-DW than the patients (p < .001). There were no differences in the changes over time in paired comparisons between patients and their next of kin in the SF-36, SEIQoL-DW, or HADS except in SF-36 physical functioning (p < .05), where patients' physical functioning decreased. The differences found between the pairs at Visit 1 were similar at following revisits in the study. The patients still had poorer estimates in the SF-36 PCS and in the subscales of PF, RP, and GH, and their next of kin still had poorer estimates in the global score in SEIQoL-DW, which can be seen in the mean values (Table 1).
Areas in SEIQoL-DW
Patients and their next of kin indicated 96 areas as being important in the SEIQoL-DW. After a reduction of those areas, patients showed 36 areas and their next of kin 31 areas. To prevent the areas from concealing the meaning of the content and preventing risks that the areas might show an overlap in item content, we chose not to further reduce the areas. The areas chosen did not change a great deal over time in either the patients or their next of kin.
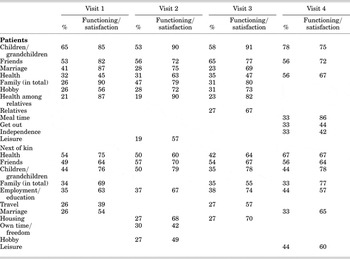
Both patients and their next of kin estimated relations such as children/grandchildren, family, marriage, and friends as important areas of life. However, the functioning/satisfaction was often better among patients than their next of kin. There were also some differences between the pairs in the chosen areas. Patients estimated, for example, hobbies as being more important whereas next of kin estimated employment/education and travel. The most important areas at each visit and their ratings of functioning/satisfaction are shown in Table 2. Figures 1 and 2 show the most important areas at Visit 1. Hobby was defined as less active interest areas (such as betting on horses, having household pets, and watching movies) and leisure was defined as more active areas of interest (such as outdoor activities).
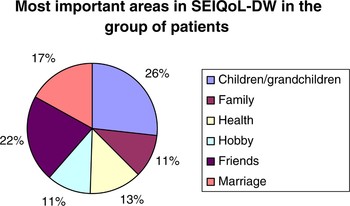
Fig. 1. (Color online) Most important areas in SEIQoL-DW among patients at Visit 1. Relations constitute 76% of important areas.
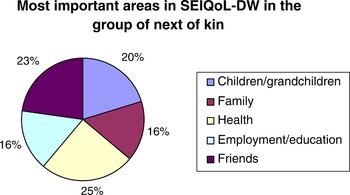
Fig. 2. (Color online) Most important areas in SEIQoL-DW among next of kin at Visit 1. Relations constitute 59% of important areas.
Table 2. Most important areas are shown in percentage of the number of participants that chose the area and mean values are calculated in functioning/satisfaction
Correlations between Physical Functional Scales ALSFRS-R and Norris Scale versus SF-36, SEIQoL-DW, and HADS
Among the patients, ALSFRS-R correlated with PF (p = .025, r = .396) and MH (p < .001, r = .566) in SF-36 over time. The Norris scale correlated with patients PCS (p = .002, r = .518), PF (p < .001, r = .471), BP (p = .016, r = .423) and MH (p = .04, r = .365) in SF-36 over time. No other correlations were found between the physical functional scales and SF-36, SEIQoL-DW, or HADS over time in patients or their next of kin except between patients' ALSFRS-R and next of kin physical functioning (p = .024, r = .397).
DISCUSSION
Our study showed an absence of change over time in SEIQoL-DW and HADS. Among patients, PCS, but not MCS in SF-36, decreased over time, which is in agreement with other studies (Norquist et al., Reference Norquist, Jenkinson and Fitzpatrick2003; De Groot et al., Reference De Groot, Post and van Heuveln2007). The lower rating in PCS is explained by the progression of the disease. The decreases in the next of kin in SF-36 might be explained by patients' increased physical needs of help and the pain of privity in their predictive loss of their spouse or relative. Burden among the next of kin over time will probably increase, which is in accordance with other studies (Chio et al., Reference Chio, Gauthier and Calvo2005; Gauthier et al., Reference Gauthier, Vignola and Calvo2007). Anxiety was found to be in a borderline range and depression in a normal range in spouse carers (Goldstein et al., Reference Goldstein, Atkins and Landau2006), which is in agreement with our study: No changes were found over time in the HADS, but the mean values for anxiety were on a level between normal and slightly increased at the two first study visits. It might therefore be important that attention is paid to these factors when caring for these families.
Few differences were seen over time between patients and their next of kin. However, it was found in the physical subscales in SF-36, where patients had poorer ratings, and in the individual QoL, where next of kin had poorer ratings. It needs to be observed that, even if there were few differences between the pairs over time, the differences between the patients and their next of kin in each pair at Visit 1 remained over time. Patients had still worse estimates in some of the subscales in SF-36 and their next of kin had worse estimates in the global score in SEIQoL-DW over the study visits. It seems that different parts of the spectrum of QoL are affected in patients and their next of kin. For this reason, it is important to give individual support according to need during the entire progression of the disease.
Patients' global scores in SEIQoL-DW in our study confirm the findings of both single investigations and studies conducted over time (Chio et al., Reference Chio, Gauthier and Montuschi2004; Neudert et al., Reference Neudert, Wasner and Borasio2004; Felgoise et al., Reference Felgoise, Stewart and Bremer2009). In our study and one other study (Bromberg & Forshew, Reference Bromberg and Forshew2002), next of kin/caregivers showed poorer global scores than their patients. A possible explanation is a greater burden among the next of kin that might cause them to renounce their own needs.
The areas chosen were often found in different varieties of relations, which might explain why they were nearly unchanged over time. If areas with a greater number of physical activities had been chosen, there could probably have been a greater change because of the successive deterioration of physical function. Both patients and next of kin reported health and relations such as children/grandchildren, friends, marriage, and family (in total) to be important areas of life. Patients more often described hobbies whereas next of kin more often described employment/education as important areas. The differences might depend on patients' loss of physical function. The patients were not able to work whereas their next of kin were healthy and worked outside the home, which was given great priority. In almost all equally important areas of life found in both patients and their next of kin, the next of kin estimated worse functioning/satisfaction than the patients (Table 2). That shows the difficulty in the next of kin's life situation, and these findings further emphasize the importance of supporting them. This is in accordance with findings by Nolan et al. (Reference Nolan, Kub and Hughes2008), who found that caregivers expressed the need of psychological, physical, and spiritual support (Nolan et al., Reference Nolan, Kub and Hughes2008).
At later study visits, patients also estimated independence, getting out, and meal times as important areas in the SEIQoL-DW. Even if there were few changes over time in the chosen areas, these areas might supervene because of the decrease in physical function. Travelling and own time/freedom were mentioned more often as important areas by the next of kin. It is possible that their own life and needs diminish in importance because their priority is to help the sick person. Housing was also an important area among the next of kin. Fear of losing the house/apartment because their economic situation had become worse or the fear that the patient would become too ill to live at home, forcing them to seek housing that better conformed to the patient's needs might underlie the ratings of these factors. Other studies have also found important areas to be family, friends, health, and hobbies. Spirituality and religion were found to be other important areas (Lo Coco et al., Reference Lo Coco, Lo Coco and Cicero2005; Felgoise et al., Reference Felgoise, Stewart and Bremer2009). These two areas were infrequently described in our study. The differences in our results and those of other researchers might have to do with cultural differences, because Sweden is a strongly secularized country.
Every patient and next of kin who had participated more than one time was given one regression coefficient, and every regression coefficient had the same rating regardless of whether the person participated two, three, or four times. The significant changes over time in Table 1 indicate decreased values regardless of whether they left the study after two, three, or four visits. This makes the fourth visit less crucial: For many patients, the participation in the study ends at Visit 2 or 3. Participants left the study successively owing to an inability to participate because of the progression of the disease or death or because of an inability to attend further visits before the study ended. Patients who participated all four times were usually in better physical condition than a patient who participated only one or two times. For that reason, the mean values at the third or fourth visit were sometimes equal to or even better than the mean values at the start of the study. To reduce risks of problems with mass significance, we focused on patterns and not single p values. However, as there were fluctuations of the QoL in patients and next of kin between the different visits, the method of using regression coefficients as a basis for evaluating QoL during the course of the disease smoothes the individual values at each visit, which hides some of the significances found when statistics are analyzed at each study interval point.
Patients diagnosed with ALS and their next of kin all go through a difficult period when they receive the diagnosis. To gain greater knowledge of their life situation and whether and how it differs over time, longitudinal studies are needed that focus on both individual and health-related QoL as well as anxiety and depression. In our study it seems that patients are more affected in HRQoL whereas next of kin are affected in both HRQoL and individual QoL. Both patients and next of kin show some changes over time in important areas of life. Our results indicate the importance of support throughout the course of the disease to both patients and their next of kin. Because ALS is an incurable disease that, sooner or later, proceeds into a palliative state, the aim must be to give as good care as possible according to the patients' and their next of kin's own needs. Because there are some different needs between the pairs, support should preferably be given both individually and in the patient/next of kin pair. With support, supervision, and confirmation of the difficult situation, there might be a possibility to improve QoL.
Information gathered by using the SEIQoL-DW might also give physicians, nurses, and other staff indications about what they should focus on to help the family achieve increased functioning/satisfaction in the areas of life that are felt to be important. It might also be easier for patients and their next of kin to find coping strategies to handle the situation when areas have been clarified. A possibility for patients and their next of kin to be able to talk with each other more openly might allow a deeper understanding of the other's priorities and needs and bring family members closer to each other.
ACKNOWLEDGMENTS
This study was supported by the Swedish Association of Persons with Neurological Disabilities, Foundation for Neurological Research, and Foundation for Neuromuscular Research. We wish to express our gratitude to Helena Johansson for providing help and guidance with the statistical methods used in the data processing.






