Introduction
Filarial infection is an important cause of morbidity in many coastal areas of India. It presents as fever, lymphatic obstruction, tropical pulmonary eosinophilia and sometimes asymptomatic microfilaraemia. Many reports are available describing microfilariae in tissue preparations, biopsies and bone marrow preparations in many diseases, including haematological malignancies (S. Gupta et al., Reference Gupta, Sodhani, Jain and Kumar2001; K, Gupta et al., Reference Gupta, Sehgal, Puri and Sidhwa2002; Singh et al., Reference Singh, Pujani and Pujani2010; Arundhati et al., Reference Arundhati, Kumar and Kumar2011). In laboratory diagnosis (Cheesbrough, Reference Cheesbrough2006), microfilariae are commonly demonstrated in peripheral blood and cytological smears or in histological preparations. This is the first report of the detection of microfilariae in conventional cytogenetic preparations.
Case reports
Case 1
A 40-year-old man presented with low-grade pyrexia, dry cough and bronchospasm of 2 weeks’ duration. Complete blood counts (CBC) showed haemoglobin (Hb) 9.8 g/dl, a white blood cell count of 8.4×103/μl and platelets 106 × 103/μl. A peripheral blood smear showed a normal differential count with normocytic, normochromic red blood cells and hyperglobulinaemia. His serum protein electrophoresis showed an M (monoclonal) band. Bone marrow aspirate showed hypercellular marrow with 42% plasma cells. There was a relative suppression of erythroid and myeloid elements. Erythropoesis was normocytic and normochromic. Microfilariae were detected in the cytogenetic preparation and the final diagnosis was multiple myeloma with filariasis.
Case 2
A 65-year-old man was diagnosed with repeated left ventricular failure. Investigations showed Hb 10 g/dl, white blood cell counts of 10 × 103/μl, platelets 140 × 103/μl with a normal differential count. The patient showed biventricular hypertrophy with restrictive cardiomyopathy. Bone marrow aspirate showed 15% plasma cells with hypercellular marrow. Plasma protein electrophoresis showed a monoclonal band, and Bence Jones protein was found in the urine. Bone marrow karyotype preparation showed microfilariae and abdominal fat biopsy showed amyloidosis. A diagnosis of multiple myeloma with cardiac amyloidosis and circulating microfilariae was made.
Case 3
A 21-year-old man presented with fever, pallor, general weakness and generalized pigmentation. Bleeding manifestations, such as petechiae and gum bleeding, were also seen. On examination a generalized lymphadenopathy, splenomegaly and hepatomegaly were observed. Investigations showed Hb 4.1 g/dl, total white blood cell count 56 × 103/μl, lymphoblasts 72%, polymorphs 8%, lymphocytes 20% and platelets 20 × 103/μl. Immunophenotyping revealed that marrow haematopoietic cells were positive for CD10, CD19, CD20, CD22 and HLA-DR and a diagnosis of B-cell acute lymphoblastic leukaemia was made. The bone marrow of this patient was processed for cytogenetic evaluation and microfilariae were detected in the cytogenetic preparation (fig. 1).
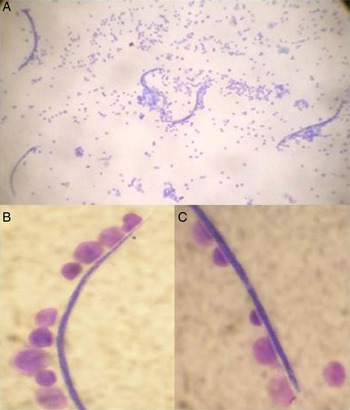
Fig. 1. (A) Microfilariae of Wuchereria bancrofti (Giemsa, ×10). (B) Distal and (C) proximal end of microfilariae with hyaline sheath and somatic granules with palisading leucocytes (Giemsa, ×100).
Case 4
A 35-year-old man presented with a dry cough, generalized body ache and anorexia of 2 months’ duration. He had abdominal fullness and generalized weakness for 15 days. CBC revealed Hb 9.2 g/dl, total white blood cell count 263×103/μl, neutrophils 67%, myelocytes 13%, basophils 2%, eosinophils 1%, myelocytes 9% and platelets 376×103/μl. Bone marrow aspiration smear showed hypercellular marrow, erythroid cells 6%, promyelocytes 1%, myelocytes and metamyelocytes 30%, bands and neutrophils 56%, basophils 2%, lymphocytes 1% and myeloblasts 4%. The erythroid series was relatively reduced and showed megaloblastic maturation. The myeloid series presented marked hyperplasia and sequential maturation was seen up to the neutrophilic stage with demonstrable giant precursors. The megakaryocyte series showed micromegakaryocytes, and the case was diagnosed as chronic myeloid leukaemia. Cytogenetic investigation revealed a Ph +ve karyotype, and microfilariae were also detected in this preparation. Hence a diagnosis of chronic myeloid leukaemia, in the chronic phase, with filariasis was made.
Discussion
Filariasis is a common global problem (Cheesbrough, Reference Cheesbrough2006). There are eight species of filarial parasites that are specific to humans. In India bancroftian filariasis is widely distributed, comprising 98% of the total filarial infections. Brugian filariasis (Brugia malayi) is found 2% of cases, and is localized in the central part of Kerala state along the coast, small pockets of Andhra Pradesh, Tamilnadu, Assam, Orissa and Madhya Pradesh (Russel et al., Reference Russel, Rao, Khamre, Praharaj and Rao1980).
Detection of microfilariae from peripheral blood, bone marrow and other tissues is achieved by screening pathological smears. However, in our cases, microfilariae were not detected in blood/bone marrow smears which were prepared to rule out leukaemia. Patients were also asymptomatic for filariasis. Microfilariae were only detected in cytogenetic preparations when sent to us for cytogenetic investigation. This could be due to the low concentration of parasites in the blood and bone marrow, and the cytogenetic method acted as a microfilaria concentration technique (Kerketta et al., Reference Kerketta, Babu Rao and Ghosh2012). There are many reports of the co-existence of microfilariae in many cancers, which raises the question whether they are merely accidental passengers in the tissues or if these patients are more prone to filarial infection due to their immunocompromised status, or whether microfilariae could have a role in the pathogenesis of these disorders, as chronic parasitic infections are associated with lower immunosurveillance, and chronic antigenic stimulation due to parasites may sustain the proliferation of immunoeffector cells (Tajima et al., Reference Tajima, Tominaga, Shimizu and Suchi1981; Hoerauf et al., Reference Hoerauf, Satoguina, Saeftel and Specht2005; Emmanuel et al., Reference Emmanuel, Kawira, Ogwang, Wabirga, Magatti, Nukruma, Neequaye, Bhatia, Brubaker, Biggar and Mbulaiteye2011). This angle needs to be studied further in detail. Moreover, the Indian Cancer Registry shows a higher prevalence of lymphoproliferative disorders in areas of endemic filariasis (Nandkumar, Reference Nandkumar2001; Sabesan et al., Reference Sabesan, Vanamali, Raju and Jambulingam2010).
In our present observation of a small series of patients, a significant number had microfilariae (4/209; 2%) compared to none in the similarly processed equivalent number of marrow smears with non-malignant disorders (Chi square test, P < 0.05). Hence, there is a persuasive argument for confirming this finding through a large-scale, well-defined epidemiological study in filaria-endemic areas, using a sensitive technique, such as the circulating filarial antigen test for bancroftian filariasis (Weil et al., Reference Weil, Lammie and Weiss1997), to prove or disprove such an association convincingly.
Financial support
The authors gratefully acknowledge the Indian Council of Medical Research for financial assistance to carry out this project.
Conflict of interest
None.



