Introduction
Botswana is besieged by a severe heterosexually driven HIV/AIDS epidemic, which has continued to devastate the country and shows very little sign of abating, despite an early comprehensive and multi-sectoral response strategy to contain the epidemic (Statistics Botswana, 2013). Botswana’s response to the HIV/AIDS epidemic has been driven through a three-pronged strategy – the promotion of Abstinence; Being faithful to one partner who has no other partners; and correct and consistent use of Condoms – otherwise known as the ABC Strategy. Of the three prongs, promotion of correct and consistent use of condoms (C) has enjoyed the most support and publicity, while the promotion of abstinence (A) and being faithful to one partner who has no other partners (B), have not received as much attention in research or implementation. Abstinence has been encouraged mostly in relation to young people delaying onset of sexual activity, while faithfulness to one partner, while desirable, has been widely questioned by many in the face of a seemingly widespread phenomenon of ‘serial monogamy’ and multiple concurrent sexual partnerships (Steffenson et al., Reference Steffenson, Pettifor, Seage, Rees and Cleary2011; Mercer et al., Reference Mercer, Aicken, Tanton, Estcourt, Brook, Keane and Cassell2013).
The HIV/AIDS epidemic has significantly elevated the risk associated with partner infidelity in sexual relationships, making such relationships themselves risk factors for HIV infection (Parker et al., Reference Parker, Pettifor, Maman, Sibeko and MacPhail2014; Wamoyi et al., Reference Wamoyi, Renju, Moshabela, McLean, Nyato, Mbata and Bonnington2017). In Botswana, this elevated risk is compounded by socio-cultural and behavioural factors such as the prevalence of multiple concurrent sexual partnerships; prevalence of STDs, especially the ulcerating kind; frequent change of sexual partners; and unequal gender relations and traditional gender norms that increase women’s risk of infection (Phaladze & Tlou, Reference Phaladze and Tlou2006; Letamo, Reference Letamo2011). Thus, the discourse on partner fidelity or infidelity has been elevated beyond the traditional realms of morality, romance, broken trust and lost love, to a much grimmer realm whereby partner infidelity equates to increased risk of HIV infection and life-long negative health consequences resulting in HIV infection, including sickness and death.
The subject of partner infidelity requires even more attention in the context of high HIV prevalence rates such as that in Botswana (17.6%) (Statistics Botswana, 2013). According to Ferrand and Mounier (Reference Ferrand, Mounier and Spira1994) it is important to understand AIDS-related risk due to infidelity, as faithfulness is a plausible strategy to reduce the risk of infection in the Botswana context (Shisana & Davids, Reference Shisana and Davids2004; Painter et al., Reference Painter, Diaby, Matia, Lin, Sibailly and Kouassi2007). On the other hand, lack of faithfulness is likely to increase the risk of exposure to HIV infection. Thus, partner infidelity, whether real or perceived, might prompt the other partner to adopt behaviour that is meant to minimize risk of infection, such as consistent use of condoms, or to leave the relationship, and end up initiating a new relationship. Furthermore, the other partner might end up being involved in serial monogamous sexual relationships (Parker et al., Reference Parker, Pettifor, Maman, Sibeko and MacPhail2014), which in the long run have the effect of increasing the risk of HIV infection. Perceived partner infidelity has been observed to have the opposite effect. For instance, an individual who feels violated by their partner’s infidelity is likely to engage in behaviour that is meant to exact emotional revenge on the unfaithful partner, such as engaging in concurrent sexual relationship, which unfortunately only increases the risk of contracting HIV (Harrison & O’Sullivan, Reference Harrison and O’Sullivan2010; King et al., Reference King, Wamai, Khana, Johansson, Lindkvist and Bunnell2012).
In the context of high levels of HIV infection, the issue of partner infidelity is likely to influence how individuals conduct themselves within sexual and intimate relationships (Mah & Maughan-Brown, Reference Mah and Maughan-Brown2013). When people have a perception (correct or incorrect) of their partner’s faithfulness, this is likely to influence their sexual and reproductive behaviour and practices. In fact, studies have found evidence of a significant association between the perception of partner unfaithfulness and having multiple sexual partnerships (Steffenson et al., Reference Steffenson, Pettifor, Seage, Rees and Cleary2011; Cox et al., Reference Cox, Babalola, Kennedy, Mbwambo, Likindikoki and Kerrigan2014; Chialepeh & Sathiyasusuman, Reference Chialepeh and Sathiyasusuman2015; Kenyon et al., Reference Kenyon, Tsoumanis, Schwartz and Maughan-Brown2016), and negative outcomes such as STIs (Fishbein et al., Reference Fishbein, Hennessy, Zer and Curtis2004; Fagbamigbe et al., Reference Fagbamigbe, Lawal and Idemudia2017) and HIV infection (Mishra, Reference Mishra, Rathavuth, Simona and Bernard2009; Mah & Shelton, Reference Mah and Shelton2011). As for a more specific case, Mishra et al. (Reference Mishra, Rathavuth, Simona and Bernard2009) found a significant inverse association between level of partner faithfulness and HIV infection among cohabiting couples in sub-Saharan Africa.
According to Pongou and Serrano (Reference Pongou and Serrano2009), faithfulness is an important quality and an ethical principle in most types of social and economic relationships. It forms the cornerstone of many types of relationships, including marriages, and has the capacity to determine the outcome of relationships. While fidelity is essential to sustain relationships, infidelity within intimate relationships does not only have dramatic social and economic consequences, but is also responsible for first-time divorces (Pittman, Reference Pittman1990, Reference Pittman1999). Norms about partner faithfulness can be quite different in different social contexts or social circles (Young, Reference Young2005), but generally most such norms prescribe actors to exchange truthful information regarding the kind of social and sexual life they have (Whisman & Snyder, Reference Whisman and Snyder2007; Parker, Reference Parker2009). Moreover, several studies in sub-Saharan Africa have shown that infidelity has negative social consequences such as risky sexual behaviours, broken trust and even divorce (Cox et al., Reference Cox, Babalola, Kennedy, Mbwambo, Likindikoki and Kerrigan2014; Kenyon et al., Reference Kenyon, Tsoumanis, Schwartz and Maughan-Brown2016; Fagbamigbe et al., Reference Fagbamigbe, Lawal and Idemudia2017).
Although Botswana’s HIV prevalence rate is still high (17.5%) there is little available empirical evidence implicating infidelity as a possible factor responsible for HIV transmission. Consequently, little is known about the influence of partner infidelity on sexual and reproductive health practices in the country. This is despite the fact that HIV prevalence among people aged 10–34 years is higher (25.9%) than the national HIV prevalence (Statistics Botswana, 2013). Understanding the influence of partner infidelity on the sexual and reproductive health practices of people aged 10–34 years will serve to reduce unfaithfulness and the transmission of HIV at an early age.
This study investigated the level and determinants of perceptions of partner infidelity, and the association between the perception of partner infidelity and respondents’ sexual and reproductive health practices. The main hypothesis tested was whether the perception of partner infidelity prompts people to adopt behaviour that is meant to compensate for the increased risk of infection posed by their partner’s infidelity, or prompts people to engage in behaviour that magnifies the risk associated with partner infidelity.
Methods
Data
The Botswana AIDS Impact Survey IV (BAIS IV) was conducted in 2013 by Statistics Botswana in close collaboration with the National AIDS Coordinating Agency (NACA). This is the latest in a series of nationally representative sample surveys aimed at providing up-to-date information on Botswana’s HIV /AIDS epidemic. The survey collected data on the behavioural patterns of the population aged 10–64 years and the HIV prevalence and incidence rates among people aged 18 months and above at national, district and sub-district levels.
A stratified, two-stage probability sampling design was used for the selection of the sample during BAIS IV. The first stage of sampling involved the selection of Enumeration Areas (EAs) and Primary Sampling Units (PSUs). These were selected with the Probability Proportional to Size (PPS) method, where Measures of Size (MOS) were the number of households in the EAs as defined by the 2011 Population and Housing Census. The second stage involved systematic selection of households from a fresh list of occupied households prepared at the beginning of the survey fieldwork. At the household level all eligible individuals aged 10–64 years were selected to respond to the face-to-face individual questionnaire. Data were collected using smartphone tablets (Statistics Botswana, 2013). The BAIS questions were validated and adapted from the previous Botswana AIDS Impact Surveys questionnaires.
The total sample for BAIS IV was 10,140, from which a sample of 6985 individuals aged 10–34 years was selected. The selection criteria for the study were being aged between 10 and 34 years and sexually active during the year preceding the survey. Selection of this cohort was based on the high HIV prevalence rate in this relatively young population group.
Measurement of variables
The dependent variables were (a) condom use consistency, (b) number of sexual partners during the year leading up to the survey and (c) having multiple and concurrent partnerships (MCP). Condom use consistency was derived from responses to questions relating to condom use with the current as well as previous sexual partners so that a composite variable was derived from the following three questions: Did you always use condoms with your most recent partner in the past 12 months?; Did you always use condoms with your next most recent partner in the past 12 months?; and Did you always use condoms with your second most recent partner in the past 12 months? All the ‘yes’ responses were summed to denote condom use consistency, while a ‘no’ answer to any, or all of, the three questions indicated inconsistent condom use. Number of sexual partners was derived by re-coding responses to the question relating to the number of sexual partners during the year leading up to the survey, whereby reporting to have no or one sexual partner meant safe sexual behaviour, and having more than one partner meant otherwise. Multiple concurrent partnership status was derived from information relating to date of last sexual activity with current and previous sexual partners, such that an overlap in the dates of sexual activity with current and previous partners was used to determine concurrency or otherwise. The coding and utilization of these variables was informed by the empirical literature (Mah & Shelton, Reference Mah and Shelton2011; Yi et al., Reference Yi, Tuot, Chhoun, Pal, Tith and Brody2015).
The main independent variable was perception of partner infidelity, which was measured through responses to questions on whether the respondents thought that their current partner (or most recent partner for those who did not have a sexual partner at the time of survey) has/had other sexual partners.
Socio-demographic characteristics were used as covariates. Conceptually these variables have been found to be associated with sexual risk behaviours and infidelity (Halperin & Epstein, Reference Halperin and Epstein2007; Mah & Halperin, Reference Mah and Halperin2008). Age was categorized as 10–14, 15–19, 20–24, 25–29 and 30–34 years. Place of residence was aggregated as city/town, urban village and rural. Marital status was categorized as never married, ever married (currently and formerly married) and living together. Educational level achieved was measured as never having attended school and among those who attended school, whether they had primary, secondary, higher, non-formal or non-standard curriculum. For the purpose of this study, three categories of education were created. Those who never attended school, those who attended non-formal school or who had a non-standard curriculum and primary level education were combined to create the category ‘primary and below’ education. Secondary and tertiary educational levels remained unchanged. Religion included three categories: Christian, non-Christian (Islam, Buddhism, Hinduism, Badimo, Sikhism, African traditional religion) and no religion
Statistical analysis
In order to investigate the association between perception of partner infidelity and respondents’ sexual and reproductive health practices, descriptive and multivariate analyses were conducted. The descriptive analyses focused on exploring levels of infidelity, while the multivariate analysis focused on the correlation between partner infidelity and sexual and reproductive health practices by socio-demographic variables. A logistic regression model was used to analyse the relationship between several explanatory variables and the qualitative response variables. The models were run in SPSS, which contained all the explanatory variables and interactions believed to influence the sexual and reproductive health practices of respondents. From the initial stage, regression analysis with the stepwise selection procedure was used to select significant variables. The adjusted model was fitted to the data to assess the association between selected sexual and reproductive health practices and perception of partner infidelity controlling for socio-demographic variables. The results are presented as odds ratios (ORs). Data analysis was done using SPSS version 25. The complex samples module in SPSS was used since the BAIS used a stratified cluster sampling design. For all comparisons, p<0.05 was considered statistically significant. Marital status was considered only for individuals aged over 18 years in the multivariate model.
Results
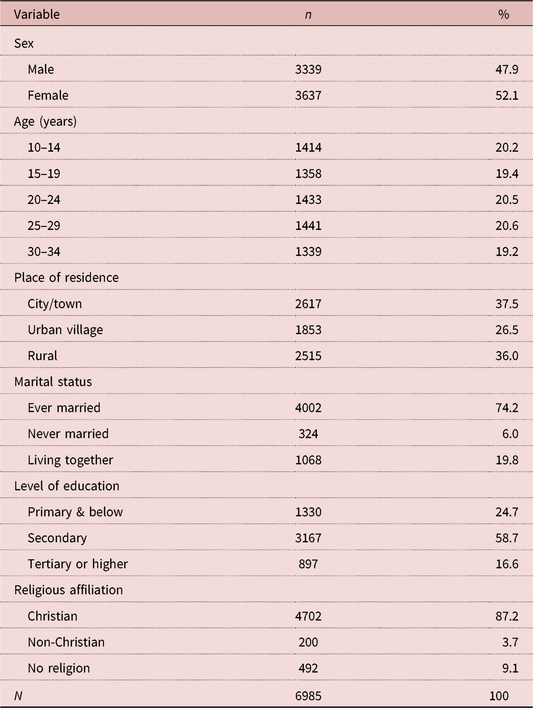
A total of 6985 people were included in the study sample, of which 52% were female (Table 1). The sample was almost equally distributed across age groups between the ages of 10 and 34 years, with about 20% in each age category. For education, 58.7% had secondary education, 24.7% primary education or less and 16.6% had tertiary education or over. The table shows that 74.3% were never married, 19.8% were in a cohabiting relationship with a sexual partner, while only 6% were married. The majority of respondents (87.2%) reported being Christians, with 9.1% reporting no religion and 3.7% non-Christian. For residence, 37.5% resided in cities and towns, 26.5% in urban villages and 36% in rural areas.
Table 1. Characteristics of sample of sexually active 10- to 34-year olds, Botswana 2013
The proportion of individuals who perceived that their current or most recent partner had other partners was 39.6%, and 79.9% felt that their previous partners had other partners (Table 2). In fact, 45.3% of respondents felt that both their current and previous partners had other partners. It was also seen that 36% of respondents used condoms inconsistently with their current partner, while 38.2% used condoms inconsistently with their current and previous partners. A tenth of the sampled population (10.4%) reported being in multiple and concurrent sexual relationships. On the other hand, 3.6% were in a serial monogamous relationship with more than one person during the year leading up to the survey, while 86% were in monogamous relationships during the year leading up to the survey.
Table 2. Perception of partner infidelity, condom use consistency and type of sexual relationship

Prevalence of perception of partner infidelity and respondent sexual risk behaviour
The proportion of respondents who had two or more sexual partners during the year leading up to the survey was much higher among those who suspected partner infidelity (32.9%) compared with those who did not (11.9%) (Table 3). The percentage of respondents who reported having multiple and concurrent sexual partnerships (MCPs) was considerably higher among respondents who suspected partner infidelity (17.8%) compared with those who did not suspect partner infidelity (6.4%). Also, the proportion of respondents who used condoms inconsistently was significantly lower (31.8%) among respondents who perceived partner infidelity compared with those who did not (39.5%).
Table 3. Association between perception of partner infidelity and sexual risk behaviours

** p<0.05.
Perception of partner infidelity and its influence on sexual risk behaviour
The adjusted model showed a significant association between perception of partner infidelity, marital status and level of education only (Table 4). The odds of perceived partner infidelity were 2.5 times (AOR=2.533, p<0.001) higher among never-married respondents compared with respondents who reported being in cohabiting relationships, while being married was associated with a 54% (AOR=0.468, p<0.001) decline in the odds of perceiving partner unfaithfulness. Secondary education was associated with increased odds (AOR=1.527, p<0.001) of perceiving partner infidelity compared with having tertiary education or higher.
Table 4. Logistic regression odds ratios (ORs) showing the likelihood of the perception of partner infidelity by socio-demographic characteristics
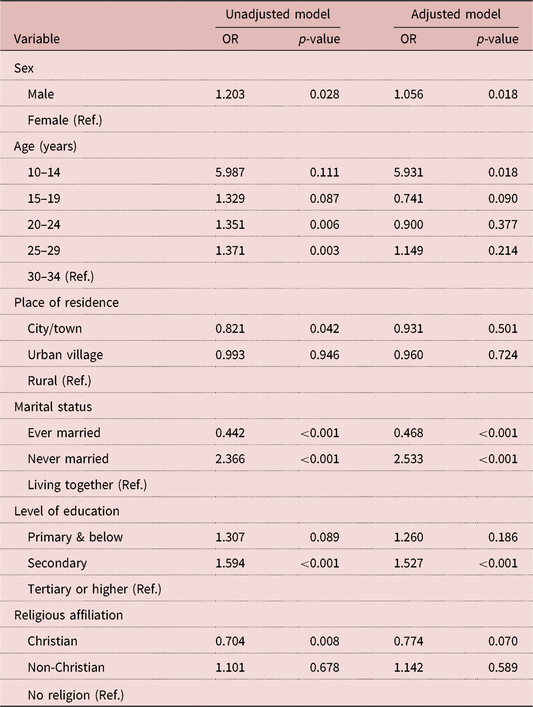
Ref.: reference category.
The adjusted model results for the association between perception of partner infidelity and number of sexual partners showed a significant association between perception of partner infidelity and number of sexual partners (Table 5). The odds of reporting multiple sex partners were 3.8 times (AOR=3.750, p<0.001) higher among respondents who suspected partner infidelity than among those who did not suspect partner infidelity. Other significant covariates of multiple sex partners were being male (OR=3.490, p<0.001) and having primary (AOR=1.686, p=0.002) or secondary education (AOR=1.265, p=0.015).
Table 5. Logistic regression odds ratios (ORs) showing the association between the perception of partner infidelity and likelihood of having two or more sexual partners by socio-demographic characteristics
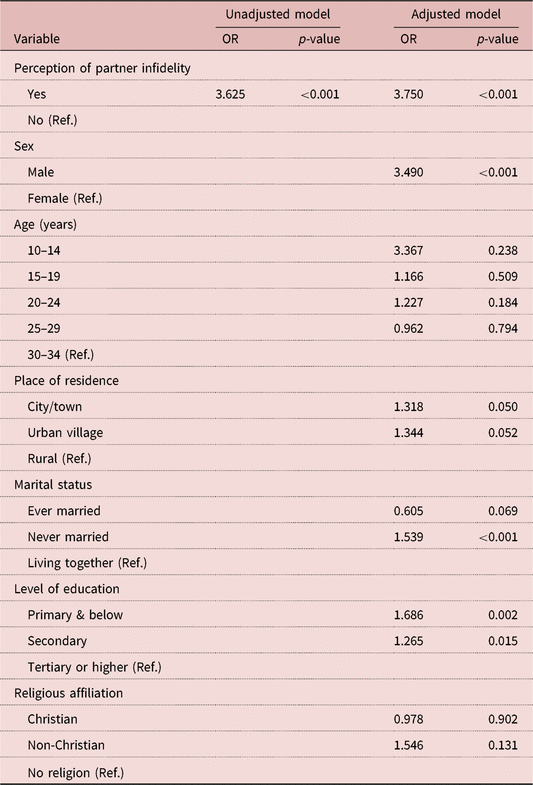
Ref.: reference category.
Perception of partner infidelity was significantly associated with having MCPs in the adjusted model (Table 6). The odds of MCP were 3.5 times (AOR=3.524, p<0.001) higher among those who suspected partner infidelity compared with those who did not suspect partner unfaithfulness. Meanwhile, there were gender differences in the odds of reporting MCP, with males being 3.4 times (AOR=3.411, p<0.001) more likely to report MCP compared with females. For education, respondents with primary education (AOR=0.342, p=0.002) and those with secondary education (AOR=0.666; p=0.021) were less likely to report having MCPs compared with respondents with tertiary education. Conversely, there was no statistically significant association between perception of partner infidelity and the likelihood of inconsistent condom use (Table 7). However, being male (AOR=0.727, p<0.001), residing in cities and towns (AOR=0.756; p=0.012) and urban villages (AOR=0.806; p=0.078) and being in a cohabiting relationship (AOR=0.560, p<0.001) were associated with a decline in the odds of reporting inconsistent condom use.
Table 6. Logistic regression odds ratios (ORs) showing the association between the perception of partner infidelity and likelihood of having multiple and concurrent sexual partnerships (MCPs) by socio-demographic characteristics

Ref.: reference category.
Table 7. Logistic regression odds ratios (ORs) showing the association between perception of partner infidelity and likelihood of inconsistent condom use with most recent partner by socio-demographic characteristics
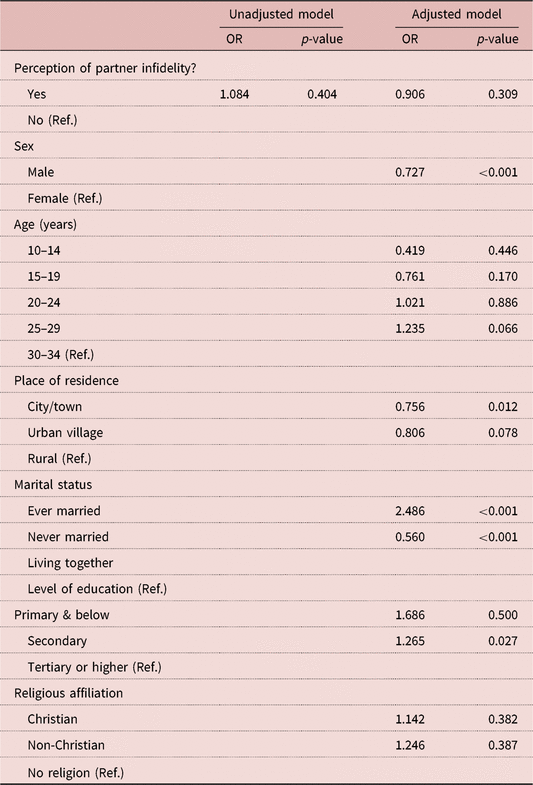
Ref.: reference category.
Discussion
The discourse on HIV prevention is a significant part of Botswana’s HIV prevention strategy. In addition to abstinence and consistent condom use, faithfulness to one sexual partner who does not have other sexual partners is fundamental. Overall, the study findings indicate the existence of a perception of partner infidelity in the sampled population. For instance, it was found that the odds of perceived partner infidelity were higher among single and secondary educated individuals. On the other hand, being married was associated with a decline in the odds of perceiving partner unfaithfulness. Perception of partner infidelity is likely to translate into unfaithfulness in the long term (Parker et al., Reference Parker, Pettifor, Maman, Sibeko and MacPhail2014) because infidelity often carries with it a more significant risk beyond embarrassment and loss of trust; it increases the risk of infection with STIs, including AIDS, and the lifelong consequences of contracting HIV (Painter et al., Reference Painter, Diaby, Matia, Lin, Sibailly and Kouassi2007; Gebeyehu et al., Reference Gebeyehu, Henk and Seydel2011; Ali Abdulai et al., Reference Ali Abdulai, Baiden, Afari-Asiedu, Gyabaa-Febir, Adjei, Mahama and Owusu-Agyei2017). As a result, partner infidelity, real or perceived, should form an important part of Botswana’s HIV epidemic research.
Contrary to previous evidence, which indicates that perception of partner infidelity is more common among men (Pittman, Reference Pittman1990, Reference Pittman1999; Ali Abdulai et al., Reference Ali Abdulai, Baiden, Afari-Asiedu, Gyabaa-Febir, Adjei, Mahama and Owusu-Agyei2017), the findings of this study show that women are equally as likely as men to suspect partner infidelity. Thus, despite the often traditionally held view and stereotype of men’s tendency for sexual infidelity, evidence emanating from these data suggests that women are also practising sexual infidelity. A plausible explanation for this scenario could be that while men are thought to maintain multiple relationships just for the kick of it, or because of cultural expectations, women are motivated to have multiple and often concurrent sexual partnerships for economic reasons (Mah & Shelton, Reference Mah and Shelton2011; Mah & Maughan-Brown, Reference Mah and Maughan-Brown2013). Additional sex partners through infidelity are likely to increase the likelihood that an individual will contract STIs such as the human papillomavirus (HPV) (Javanbakht et al., Reference Javanbakht, Gorbach, Amani, Walker, Cranston, Datta and Kerndt2010) or bacterial STIs (Kraut-Becher & Aral, Reference Kraut-Becher and Aral2003).
Consistent with the findings of other studies, it was found that people who perceived their partner to be unfaithful were more likely to report being involved in multiple sexual partnerships. Similarly, Gebeyehu et al. (Reference Gebeyehu, Henk and Seydel2011) found that in a sample of largely illiterate male respondents in Ethiopia, those who perceived their partner to be unfaithful were themselves often involved in other sexual relationships. The fact that the perception of partner infidelity was found to be significantly associated with reporting multiple serial sexual relationships and multiple concurrent sexual relationships shows that, indeed, the perception of partner infidelity has a significant influence on sexual practices. Actually, people who perceive partner infidelity may not only be worried about the increased risk of infection with STIs emanating from their partner’s lack of faithfulness, but are also likely to engage in risky behaviours such as frequent change of partners and maintenance of MCP (Schonian, Reference Schonian2013). Unfortunately, this is likely to further increase their risk of infection. Other studies, such as that conducted by Kenyon et al. (Reference Kenyon, Tsoumanis, Schwartz and Maughan-Brown2016) in South Africa, have made a similar observation, that partners who perceive infidelity are more likely to engage in frequent change of partners and continue in MCPs.
This study set out to investigate whether perception of partner infidelity prompts young people to adopt behaviour that is meant to compensate for the increased risk of infection posed by their partner’s infidelity; or whether it prompts young people to engage in behaviour that magnifies the risk associated with partner infidelity. It found that the perception of partner infidelity influences people’s sexual behaviours in a way that may increase the risk of infection. Specifically, it was found that people who perceived their partner to be unfaithful were more likely to engage in multiple sexual relationships, and multiple concurrent sexual relationships. It is thus important for Botswana’s HIV/AIDS prevention strategies to seriously consider and re-emphasize fidelity to one partner as the most effective HIV prevention strategy. This may involve strategies to improve partners’ trust and confidence within relationships by enhancing individuals’ skills to communicate with each other. Further studies need to be undertaken, especially qualitative studies, to understand in-depth socio-cultural attitudes in Botswana towards infidelity. These studies will shed more light onto the best strategies to encourage partner faithfulness in order to reduce HIV transmission in Botswana. These strategies may not succeed if socio-cultural attitudes underlying infidelity are unknown.
Acknowledgments
The authors are especially grateful to the University of Botswana for providing both the time and space in which this research has conducted. They also thank Statistics Botswana for graciously allowing the use of this dataset. The authors are also grateful to the many reviewers, some anonymous, including friends and colleagues in the Department of Population Studies and Faculty of Social Sciences, University of Botswana, for providing invaluable insights that contributed to improving this manuscript.
Funding
This research used secondary data and therefore did not receive any grant from a funding agency, commercial entity or not-for-profit organization.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.









