Introduction
Several definitions of the term novel/new psychoactive substances (NPS) are in use, with the term ‘new’ not necessarily referring to new inventions but to substances that have recently been made available (UNODC, 2013). Hence, ‘new’ can include a failed pharmaceutical or an old patent which has been ‘rediscovered’ and marketed for its potential use as a ‘recreational’ substance. Conversely, the term ‘novel’ can also express something newly created, or a compound that has come back into fashion after a period of absence from the recreational drug scene, or indeed a known NPS molecule being used in an innovative or unusual way, hence presenting with a ‘novelty’ appeal (Corkery et al., Reference Corkery, Orsolini, Papanti, Schifano, Miolo, Stair and Zloh2018a). Another distinction being made is between NPS and Emerging Psychoactive Substances (EPS), where the latter term captures all NPS as well as drugs that may not be newly invented, but have recently experienced a resurgence of, or increase in, use (Sutherland and Barratt, Reference Sutherland and Barratt2016).
Number and types of NPS in both real and online scenarios
Between 2009 and 2017, a total of 803 NPS were reported by 111 countries/territories (UNODC, 2018a; 2018b). In the EU, by the end of 2017 the number of NPS was over 670, of which 632 were notified after 2004 (EMCDDA, 2018); most molecules were synthetic cannabinoids, synthetic cathinones, phenethylamine derivatives and synthetic opioids.
Both the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) and the United Nations Office on Drugs and Crime (UNODC), however, include an index NPS in their database only when the NPS is seized, chemically analysed and notified to them. However, one could argue that the NPS scenario is much larger than that formally identified by international agencies. Hence, an approach aiming at describing what is being discussed online by the web-based NPS enthusiasts ‘e-psychonauts’ (Orsolini et al., Reference Orsolini, Papanti, Francesconi and Schifano2015) has been considered as potentially useful to identify in advance the NPS availability, market and diffusion. In fact, the online NPS scenario, with its related concerns, typically predicts the real-life NPS scenario (Corazza et al., Reference Corazza, Assi, Simonato, Corkery, Bersani, Demetrovics, Stair, Fergus, Pezzolesi, Pasinetti, Deluca, Drummond, Davey, Blaszko, Moskalewicz, Mervo, Furia, Farre, Flesland, Pisarska, Shapiro, Siemann, Skutle, Sferrazza, Torrens, Sambola, van der Kreeft, Scherbaum and Schifano2013). Consistent with this, a risk of violent behaviour associated with NPS intake has been identified in patients presenting to London (UK) acute mental health services (Shafi et al., Reference Shafi, Gallagher, Stewart, Martinotti and Corazza2017). Furthermore, both the psychopathological and aggression issues associated with the Ibiza clubbing scenario drug intake (Martinotti et al., Reference Martinotti, Cinosi, Santacroce, Papanti, Pasquini, Mancini, Corbo, Fiori, Sarchione, Marchetti, Verrocchio, Di Giannantonio, Torrens, Schifano, Morlan Coarasa and Merino Del Villar2017) had been somehow predicted by previous studies (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015, Reference Schifano, Papanti, Orsolini and Corkery2016) based on the observation of the evolving ‘e-psychonauts’ scenario.
Aims
In this study, we aimed at: (a) identifying and describing the large number of NPS available as identified from a range of psychonauts', NPS-related, online sources; and (b) describing the short-/long-term clinical effects of the NPS most commonly associated with the onset of those psychopathological consequences which are of interest for mental health professionals. These NPS include synthetic cannabinoids/cannabimimetics; new synthetic opioids; ketamine-like dissociatives; novel stimulants and novel psychedelics; prescription and over-the-counter (OTC) medicines (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015).
Methods
To facilitate the process of early recognition of the increasing dissemination of new substances online and the variability of information sources, a crawling/navigating software (i.e. the ‘NPS.Finder®’, 2019) was designed to automatically scan the open/surface web for new/novel/emerging NPS. This was meant to map on a 24/7 basis the large variety of psychoactive molecules mentioned/discussed within a range of major and representative online psychonaut web sites/fora (the full list of these sites is available upon request). The NPS.Finder® was designed to extract a range of information regarding NPS, including chemical and street names; chemical formula; three-dimensional image and anecdotally reported clinical/psychoactive effects. Resulting data were checked against the EMCDDA and UNODC NPS databases. The collection of further information was completed by consulting a range of open libraries and chemistry databases referring to the index item, if existing. These data were then automatically stored in an online, restricted access/password-controlled database located within firewall protected, highly secure and consistently performing servers. After completion of proper piloting searches, a range of specific web scraper/crawler activities, to extract all accessible posts/entries from 26 November 2017 and up to end of May 2019, were carried out. When any new item was detected during the automated web scan, the system sent an e-mail notification/alert to the core researchers' mailing list. Eventually, these data were screened for relevance and to exclude possible duplications. Finally, using chemical structure identification and published related data, researchers assigned each molecule to its NPS drug class (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015). Although the language most typically used by psychonauts was English, further languages here analysed by NPS.Finder® (2019) included: Dutch, French, Turkish, Swedish, Spanish, German, Russian and Italian.
To describe the medical and psychopathological issues most typically associated with the range of NPS intake, the Medline/PubMed database(s), were searched for papers using the terms ‘new psychoactive substances’, ‘novel psychoactive substances’, ‘designer drugs’ and ‘emerging drugs of abuse’. A similar search was carried out for the main groups of pre-selected NPS molecules and related medical and psychopathological consequences.
Results
Preliminary data from the NPS.Finder® web crawling activities
After about 18 months of operation, the number of substances identified by the web crawler activities was 5922. By the time of writing, some 4204 unique NPS molecules were included in the database and 1718/5922 (29.01%) remaining molecules resulted to be false positives/duplicates. Most popular NPS mentioned in the psychonauts' fora included: psychedelic phenethylamines (1262; 30%); synthetic cannabimimetics (1248; 29.7%); synthetic opioids (460; 10.9%); GABA-A/GABA-B receptor agonists (172; 4.1%); synthetic cathinones (171; 4.1%); prescribed/OTC medicinal compounds (157; 3.7%); novel stimulants (82; 1.9%); novel psychedelics (38; 0.9%) and PCP/ketamine-like compounds (36; 0.8%).
Synthetic cannabinoids/cannabimimetics (SC)
Whilst low-dosage levels of synthetic cannabinoids (SC) produce similar psychoactive effects to cannabis/THC, with higher dosages auditory/visual hallucinations, anxiety and intense feelings of paranoia often occur (Winstock and Barratt, Reference Winstock and Barratt2013a; Wessinger et al., Reference Wessinger, Moran, Seely, Campolongo and Fattore2015; Bonaccorso et al., Reference Bonaccorso, Metastasio, Ricciardi, Stewart, Jamal, Naasir-Ud-Dinn, Theleritis, Ferracuti, Ducci and Schifano2018). Other psychiatric and neurological effects include: behavioural dyscontrol and agitation (Brakoulias, Reference Brakoulias2012); mood swings (Celofiga et al., Reference Celofiga, Koprivsek and Klavz2014); suicidal ideation, suicide attempts (Glue et al., Reference Glue, Al-Shaqsi, Hancock, Gale, Strong and Schep2013); panic attacks; thought disorganisation and agitated/excited delirium (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2017). A florid/acute/transient psychosis; relapse/worsening of a pre-existing psychosis and bipolar disorder (Oluwabusi et al., Reference Oluwabusi, Lobach, Akhtar, Youngman and Ambrosini2012; Ustundag et al., Reference Ustundag, Ozhan Ibis, Yucel and Ozcan2015) and the persistent psychotic disorder ‘spiceophrenia’ (Papanti et al., Reference Papanti, Schifano, Botteon, Bertossi, Mannix, Vidoni, Impagnatiello, Pascolo-Fabrici and Bonavigo2013; Schifano et al., Reference Schifano, Papanti, Orsolini and Corkery2016) have all been described. With synthetic cannabinoids, similar to what being described for a range of remaining NPS (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015), the total or partial recurrence of perceptual disturbances that appeared during previous hallucinogenic intoxications, typically known as Hallucinogen-Persisting Perception Disorder (HPPD), may occur (Martinotti et al., Reference Martinotti, Santacroce, Pettorruso, Montemitro, Spano, Lorusso, di Giannantonio and Lerner2018) (Table 1).
Table 1. Main categories of Novel/New Psychoactive Substances (NPS) and their effects
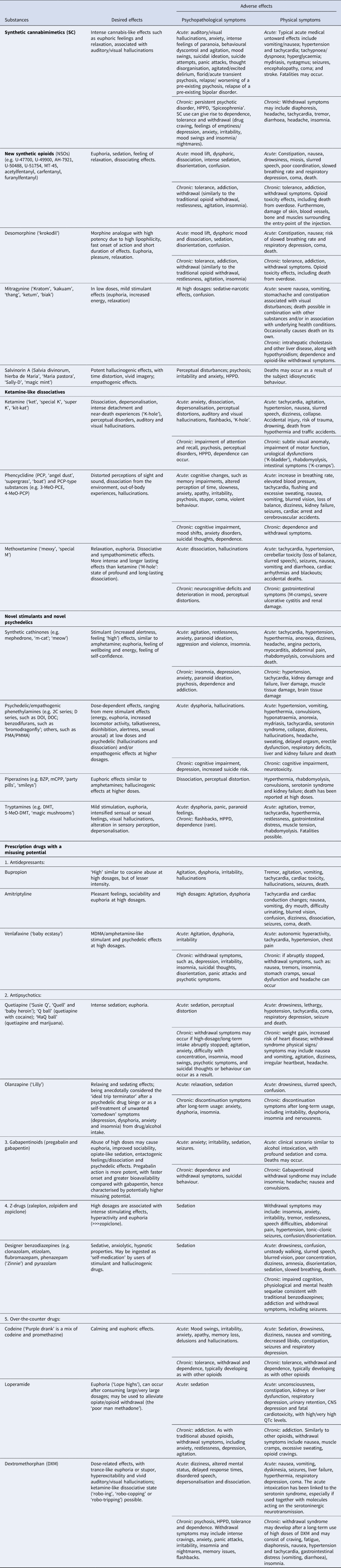
DXM, dextromethorphan, SC, synthetic cannabinoids, HPPD, hallucinogen-persisting perception disorder.
The intoxication/acute toxic effects of SCs appear to be more akin to those experienced with sympathomimetic/stimulant drug use (Wood and Dargan, Reference Wood and Dargan2012; Naviglio et al., Reference Naviglio, Papanti, Moressa and Ventura2015). Typical medical untoward effects include: vomiting/nausea; hypertension and tachycardia; tachypnoea/dyspnoea; hyperglycaemia; mydriasis (Hermanns-Clausen et al., Reference Hermanns-Clausen, Kneisel, Szabo and Auwärter2013; Winstock and Barratt, Reference Winstock and Barratt2013b; Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015); nystagmus; seizures (Hopkins and Gilchrist, Reference Hopkins and Gilchrist2013); encephalopathy (Louh and Freeman, Reference Louh and Freeman2014); coma and stroke (Mir et al., Reference Mir, Obafemi, Young and Kane2011; Freeman et al., Reference Freeman, Rose and Myers2013; Rose et al., Reference Rose, Guerrero and Mokin2015). Ultimately, deaths have been associated with the use of synthetic cannabinoids, either on their own or in combination (Corkery et al., Reference Corkery, Claridge, Loi, Goodair and Schifano2014; Tait et al., Reference Tait, Caldicott, Mountain, Hill and Lenton2015; Trecki et al., Reference Trecki, Gerona and Schwartz2015; Angerer et al., Reference Angerer, Jacobi, Franz, Auwärter and Pietsch2017; Maeda et al., Reference Maeda, Kikura-Hanajiri, Kawamura, Nagashima and Yoshida2018; Olsen, Reference Olsen2018; Paul et al., Reference Paul, Simms, Amini and Paul2018). These may result from direct lethality of the molecule; behavioural dyscontrol or suicide (Rosenbaum et al., Reference Rosenbaum, Carreiro and Babu2012; Shanks et al., Reference Shanks, Dahn and Terrell2012; Patton et al., Reference Patton, Chimalakonda, Moran, McCain, Radominska-Pandya, James, Kokes and Moran2013; Lászik et al., Reference Lászik, Törő, Vannai, Sára-Klausz, Kócs, Farkas, Keller and Róna2015) (Table 1).
Finally, SC long-term use can give rise to dependence/tolerance phenomena (Gunderson et al., Reference Gunderson, Haughey, Ait-Daoud, Joshi and Hart2012; Spaderna et al., Reference Spaderna, Addy and D'Souza2013); a withdrawal syndrome, characterised by: profuse sweating, tachycardia, tremor, diarrhoea, headache, drug craving, feelings of emptiness/depression, anxiety, irritability, mood swings and insomnia/nightmares has been described (Macfarlane and Christie, Reference Macfarlane and Christie2015) (Table 1).
New synthetic opioids (NSOs)
New synthetic opioids (NSOs) emerged in recent years as part of the alarming worldwide opioid crisis (Van Amsterdam and van den Brink, Reference Van Amsterdam and van den Brink2015; CDC, 2016, 2018; Armenian et al., Reference Armenian, Vo, Barr-Walker and Lynch2017; EMCDDA, 2017; Lucyk and Nelson, Reference Lucyk and Nelson2017; Prekupec et al., Reference Prekupec, Mansky and Baumann2017; Suzuki and El-Haddad, Reference Suzuki and El-Haddad2017; Drummer, Reference Drummer2018; Graddy et al., Reference Graddy, Buresh and Rastegar2018). NSOs are a large group of narcotic analgesic drugs having structural similarities, but much greater potency of action and receptor affinity, with respect to morphine (Tracy et al., Reference Tracy, Wood and Baumeister2017; Marchei et al., Reference Marchei, Pacifici, Mannocchi, Marinelli, Busardò and Pichini2018; Solimini et al., Reference Solimini, Pichini, Pacifici, Busardò and Giorgetti2018). This group includes compounds which were originally synthesised by pharmaceutical companies but never commercialised and then diverted into the illegal market, e.g. benzamide (U-47700, U-49900, AH-7921); acetamide (U-50488, U-51754); piperazine derivatives (MT-45) (Zawilska, Reference Zawilska2017) and several illicitly manufactured fentanyl analogues, e.g. acetylfentanyl; carfentanyl; furanylfentanyl; 3-methylfentanyl; sufentanyl; etc. (Armenian et al., Reference Armenian, Vo, Barr-Walker and Lynch2017; Suzuki and El-Haddad, Reference Suzuki and El-Haddad2017; Marchei et al., Reference Marchei, Pacifici, Mannocchi, Marinelli, Busardò and Pichini2018). These molecules may be used alone; as adulterants in heroin; or as constituents of other illicit products or counterfeit medications (Prekupec et al., Reference Prekupec, Mansky and Baumann2017; Abdulrahim et al., Reference Abdulrahim and Bowden-Jones2018).
NSOs' toxicity includes drowsiness, sedation, disorientation, slurred speech, confusion, dizziness, nausea, miosis, slowed breathing and respiratory depression to coma (Suzuki and El-Haddad, Reference Suzuki and El-Haddad2017). Conversely, NSOs' psychotropic effects include sedation; euphoria; feeling of relaxation; mood lift, dysphoric and dissociating effects (Solimini et al., Reference Solimini, Pichini, Pacifici, Busardò and Giorgetti2018) (Table 1).
Due to their high potency, their continued use (or abuse) may induce tolerance, with the risk of overdose and death being elevated. Physical dependence and addiction may rapidly rise, and withdrawal symptoms occur if their use is rapidly reduced or suddenly stopped. These include symptoms similar to the traditional opioid withdrawal, such as restlessness, agitation, muscle and bone pain, insomnia, diarrhoea, vomiting and cold flashes with goose bumps (Suzuki and El-Haddad, Reference Suzuki and El-Haddad2017; Zawilska, Reference Zawilska2017).
Other compounds classified among NSOs are desomorphine (‘krokodil’), mitragynine and 7-hydroxymitragynine (alkaloids found in ‘kratom’/Mitragyna speciosa; Liu et al., Reference Liu, Wheeler, Venkataramanan, Rymer, Pizon, Lynch and Tamama2018; Corkery et al., Reference Corkery, Streete, Claridge, Goodair, Papanti, Orsolini, Schifano, Sikka, Korber and Hendricksin press) and salvinorin A, with its analogue herkinorin, which are the main Salvia divinorum components. Salvinorin A psychoactive effects include perceptual disturbances, psychosis, irritability and anxiety (Ventura et al., Reference Ventura, Carvalho and Dinis-Oliveira2018) (Table 1).
Ketamine-like dissociatives
Ketamine and phencyclidine (PCP) were both originally developed as general anaesthetics for veterinary and human use, but soon became street drugs. Despite the strong dissociative effects on post-operative patients, ketamine is used as anaesthetic mostly in veterinary practice, but also in emergency medicine (Baumeister et al., Reference Baumeister, Tojo and Tracy2015). Ketamine (‘special K’) can be injected, snorted, smoked or administered rectally, at a dosage range of 25–300 mg, inducing feelings of relaxation, dissociation, depersonalisation and psychotic experiences, with hallucinations lasting even longer than the anaesthetic effects.
Ketamine intoxication may include cardiovascular and respiratory symptoms and, due to its anaesthetic and dissociative effects, related risks may include trauma, drowning, death from hypothermia and traffic accidents (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015) (Table 1). The ‘K-hole’, which may result after the ingestion of large dosages of ketamine, is a typical out-of-body/near-death experience, with the user becoming trapped in a state of detachment from his/her physical presence. Residual symptoms, such as flashbacks and perceptual distortions, may follow.
Long-term ketamine use may present with both urological (‘K-bladder’) and intestinal (‘K-cramps’) symptoms (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015). Compared with ketamine, PCP (‘angel dust’) appears to determine much wider and unstable range of symptoms, with cerebrovascular accidents and cardiac arrest occurring (Baumeister et al., Reference Baumeister, Tojo and Tracy2015). Chronic use of PCP may impair memory and thinking, and determine mood shifts, anxiety and suicidal thoughts (DEA, 2013) (Table 1).
Further related dissociatives recently entered the market (Wallach et al., Reference Wallach, Kang, Colestock, Morris, Bortolotto, Collingridge, Lodge, Halbertstadt, Brandt and Adejare2016), including 4-MeO-PCP (Morris and Wallach, Reference Morris and Wallach2014); the 1,2-diarylethylamines (e.g. diphenidine, ephenidine, methoxydiphenidine and various analogues such as fluorolintane and N-ethyl-lanicemine) and the β-keto-arylcyclohexylamines (e.g. methoxetamine, deschloroketamine and 2-fluoro-2-deschloroketamine) molecules (Wallach and Brandt, Reference Wallach and Brandt2018). They primarily act as uncompetitive antagonists at glutamatergic NMDA receptors, but may also bind at opioid and monoaminergic receptors (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015). Their effects are diverse and dose-dependent, generally inducing a mind-altering state, with sensory hallucinations, tactile distortions, euphoria, derealisation and depersonalisation (Wallach et al., Reference Wallach, Kang, Colestock, Morris, Bortolotto, Collingridge, Lodge, Halbertstadt, Brandt and Adejare2016; Tracy et al., Reference Tracy, Wood and Baumeister2017) (Table 1).
Novel stimulants and novel psychedelics, including psychedelic phenethylamines
Novel stimulant and novel psychedelic compounds include phenethylamines, cathinones, piperazines, tryptamines, pipradrols/piperidines, aminoindanes, benzofurans and amphetamines; all of these present with varying levels of stimulant, entactogenic and hallucinogenic effects. They exert an inhibitory action on the monoamine reuptake, increasing the quantity of noradrenaline/NA, dopamine/DA and serotonin/5-HT in the synaptic cleft (Miliano et al., Reference Miliano, Serpelloni, Rimondo, Mereu, Marti and De Luca2016). Consistent with their pharmacological profile, those molecules that present with high serotonin:dopamine ratios may be considered analogous to entactogenic substances, such as MDMA. Conversely, high dopamine:serotonin ratios might predict a strong stimulant experience. Furthermore, high or low affinity to modulation of noradrenergic systems might be anticipated to be associated with varying sympathetic nervous system activation, whereas activation of 5-HT2A/1A receptors would more likely predict hallucinogenic effects (Baumeister et al., Reference Baumeister, Tojo and Tracy2015) (Table 1).
Presenting with structural similarities to amphetamines (Feng et al., Reference Feng, Battulga, Han, Chung and Li2017), synthetic cathinones (EMCDDA, 2017) are mostly inhibitors of the serotonin (SERT), dopamine (DAT) and noradrenaline (NET) transporters. These molecules can be further sub-categorised as: (1) cocaine/MDMA-like (3,4-methylenedioxy-N-alkylated cathinones e.g. butylone): these act as inhibitors at SERT, DAT and NET and as serotonin releasers; (2) methamphetamine-like (N-alkylated or ring-substituted cathinones e.g. buphedrone): these act as inhibitors at SERT, DAT and NET and as dopamine releasers and (3) pyrovalerone-like cathinones (N-pyrrolidine cathinones e.g. MDPV (3,4-methylenedioxypyrovalerone)): these are very potent at DAT and do not induce any monoamine substrate release (Simmler et al., Reference Simmler, Buser, Donzelli, Schramm, Dieu, Huwyler and Liechti2013).
Apart from mephedrone (Dargan et al., Reference Dargan, Albert and Wood2010; Winstock, Reference Winstock2010; Winstock et al., Reference Winstock, Mitcheson, Ramsey, Davies, Puchnarewicz and Marsden2011; Freeman et al., Reference Freeman, Morgan, Vaughn-Jones, Hussain, Karimi and Curran2012; Prosser and Nelson, Reference Prosser and Nelson2012; Karila et al., Reference Karila, Megarbane, Cottencin and Lejoyeux2015, Reference Karila, Billieux, Benyamina, Lançon and Cottencin2016; De Sousa Fernandes Perna et al., Reference De Sousa Fernandes Perna, Papaseit, Pérez-Mañá, Mateus, Theunissen, Kuypers, de la Torre, Farré and Ramaekers2016), the psychopathological consequences of most cathinones have not been fully studied. With mephedrone, low mood, loss of appetite, difficulty sleeping, levels of paranoid ideation, cognitive impairment, changes in perception, agitation, hallucinations, delusions, amnesia, confusion, violence and suicidal thoughts have been reported (Kehr et al., Reference Kehr, Ichinose, Yoshitake, Goiny, Sievertsson, Nyberg and Yoshitake2011; Capriola, Reference Capriola2013; Herzig et al., Reference Herzig, Brooks and Mohr2013; John et al., Reference John, Thomas-Rozea and Hahn2017; Lovrecic and Lovrecic, Reference Lovrecic and Lovrecic2017; Homman et al., Reference Homman, Seglert and Morgan2018; Kaizer-Będkowska and Kucia, Reference Kaizer-Będkowska and Kucia2018). Users reported as well positive effects e.g. euphoria, improved psychomotor speed, alertness and talkativeness (Dargan et al., Reference Dargan, Albert and Wood2010; Cheng et al., Reference Cheng, Yeo, Brown and Regan2012; Mdege et al., Reference Mdege, Meader, Lloyd, Parrott and McCambridge2017). Cathinone-induced acute intoxication may include symptoms of the serotonin syndrome, associated with aggression and hyperthermia, psychotic disorders, catatonia and excited delirium syndrome (Otachbachi et al., Reference Otachbachi, Cevik, Bagdure and Nugent2010; Penders and Gestring, Reference Penders and Gestring2011; Mugele et al., Reference Mugele, Nanagas and Tormoehlen2012; Penders et al., Reference Penders, Gestring and Vilensky2012; Warrick et al., Reference Warrick, Wilson, Hedge, Freeman, Leonard and Aaron2013; Hohmann et al., Reference Hohmann, Mikus and Czock2014; Denysenko et al., Reference Denysenko, Freudenreich, Philbrick, Penders, Zimbrean, Nejad, Chwastiak, Dickerman, Niazi, Shim and Soellner2015; Weaver et al., Reference Weaver, Hopper and Gunderson2015). Other acute intoxication issues included dehydration, hypertension, tachycardia, kidney and liver impairment, electrolyte imbalance, metabolic toxicity, cerebral oedema and death (Borek and Holstege, Reference Borek and Holstege2012; Adebamiro and Perazella, Reference Adebamiro and Perazella2013; Imam et al., Reference Imam, Patel, Mahmoud, Prakash, King and Fremont2013). Suicides by hanging and deaths from firearm injuries have frequently been reported (Marinetti and Antonides, Reference Marinetti and Antonides2013; Barrios et al., Reference Barrios, Grison-Hernando, Boels, Bouquie, Monteil-Ganiere and Clement2016), as well as deaths from toxicity (Corkery et al., Reference Corkery, Goodair, Claridge, Corazza and Roman-Urrestarazu2018b). Although the long-term effects of synthetic cathinones' use are largely unknown, they may include insomnia, depression, anxiety, psychosis and dependence (Capriola, Reference Capriola2013).
Phenethylamines are synthetic compounds available in tablets, capsules and powder. They act on serotoninergic receptors, hence leading to psychedelic effects, but some of them inhibit the NA/DA reuptake as well. 3,4-Methylenedioxy-methamphetamine (MDMA, ‘ecstasy’) is one of the most popular drugs among youngsters/clubbers, because of its stimulant effects. Recently the emergence of a range of other psychedelic phenethylamines, including the 2-C and 2-D series drugs; the benzodifurans (e.g. 3-C-bromo-dragonfly) and others (e.g. 4-MTA, 6-APB, 4,4′-DMAR and PMA), has been reported (Miliano et al., Reference Miliano, Serpelloni, Rimondo, Mereu, Marti and De Luca2016). Their psychoactive effects are dose-dependent, ranging from stimulant effects at lower doses to hallucinogenic and entactogenic effects at higher doses. Phenethylamines' intake may be associated with loss of appetite, tachycardia, hypertension, anxiety, nausea, headache, dizziness, skin irritation, hyperthermia, convulsions, respiratory deficits, liver/kidney failure and death (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015). Psychotic symptoms are associated with a high dosage intake (Baumeister et al., Reference Baumeister, Tojo and Tracy2015) (Table 1).
The lead compound in piperazines, N-benzylpiperazine (BZP), has a typical central nervous system stimulant structure. Structurally similar to amphetamine and initially developed as an antidepressant, BZP triggers the release of DA and NA whilst inhibiting the uptake of DA, NA and 5-HT (Miliano et al., Reference Miliano, Serpelloni, Rimondo, Mereu, Marti and De Luca2016). Piperazines' toxicity causes hallucinations, seizures, hyponatraemia, serotonin syndrome, renal failure and ultimately death (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015) (Table 1).
Tryptamines, with the most common molecule being the lysergic acid diethylamide/LSD, are a group of monoamine alkaloids very similar to the endogenous neurotransmitter serotonin. They act both as 5-HT2A receptor agonists and serotonin reuptake inhibitors. A large range of novel tryptamines, including 5-MeO-AMT, 5-MeO-DALT, 4-HO-DALT, 5-MeO-DIPT and 5-MeO-DMT, have appeared on the drug scene (Miliano et al., Reference Miliano, Serpelloni, Rimondo, Mereu, Marti and De Luca2016). Some of them are found in nature, e.g. Delosperma species plants (containing dimethyltryptamine/DMT; 5-MeO-DMT); hallucinogenic fungi (psilocin; 4-OH-DMT) and amphibians (bufotenin) (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015). The predominant clinical effects of tryptamines consist of visual hallucinations, alterations in sensory perception, distortion of body image, depersonalisation, marked mood lability and anxiety/panic. Untoward effects include agitation, tachyarrhythmia and hyperpyrexia. There are small numbers of tryptamine-related fatalities (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015) (Table 1).
Prescription and OTC drugs
Over the past decade, the recreational use of several psychoactive pharmaceuticals has emerged in the NPS scene, including antidepressants; antipsychotics; gabapentinoids; Z-drugs and designer benzodiazepines and OTC drugs (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015, Reference Schifano, Chiappini, Corkery and Guirguis2018).
Antidepressants
Antidepressants emerged as being misused, raising public health concerns on their prescription control policies (Evans and Sullivan, Reference Evans and Sullivan2014). Bupropion inhibits both the NA and DA reuptake (Schifano and Chiappini, Reference Schifano and Chiappini2018a) and, being a cathinone derivative, presents with stimulant activities (Evans and Sullivan, Reference Evans and Sullivan2014; Baumeister et al., Reference Baumeister, Tojo and Tracy2015). It may be consumed orally, insufflated or injected, with high dosages provoking a ‘high’ similar to cocaine (Vento et al., Reference Vento, Schifano, Gentili, Pompei, Corkery, Kotzalidis and Girardi2013). Adverse effects range from nasal pain to irritability, agitation, cardiac toxicity, hallucinations and seizures. Vulnerable users are inmates and patients with past histories of substance misuse (Schifano and Chiappini, Reference Schifano and Chiappini2018a) (Table 1).
Amitriptyline anecdotally emerged as the most abused among tricyclic antidepressants giving, at high dosages, ‘pleasant feelings’ and euphoria. Its anticholinergic and antihistamine effects may contribute to its abuse liability (Evans and Sullivan, Reference Evans and Sullivan2014). Tachycardia and cardiac conduction changes are common in patients ingesting high dosages of tricyclic antidepressants; overdoses may be fatal (Shenouda and Desan, Reference Shenouda and Desan2013) (Table 1).
At high/supratherapeutic doses (e.g. 400–4000 mg/day), the phenylethylamine derivative venlafaxine (‘baby ecstasy’) inhibits the reuptake of serotonin, noradrenalin and dopamine, particularly at the prefrontal cortex level (Francesconi et al., Reference Francesconi, Orsolini, Corkery, Papanti and Schifano2015). If suddenly discontinued, a withdrawal syndrome characterised by nausea, depression, suicidal thoughts, disorientation, stomach cramps, panic attacks, sexual dysfunction, headache and occasional psychotic symptoms may develop (Table 1).
Antipsychotics
Quetiapine (FDA, 2010) recently emerged on the drug scenario as being used for recreational purposes (Klein et al., Reference Klein, Bangh and Cole2017), which may have contributed to increased poisonings and related fatalities (Lee et al., Reference Lee, Pilgrim, Gerostamoulos, Robinson and Wong2018). Crushed quetiapine tablets can be self-administered through nasal insufflation, ingested or injected (Chiappini and Schifano, Reference Chiappini and Schifano2018). The intentional abuse of quetiapine is associated with sedation and euphoria (Lee et al., Reference Lee, Pilgrim, Gerostamoulos, Robinson and Wong2018). Quetiapine is also abused concomitantly with other illicit substances, such as cocaine (‘Q ball’; Lee et al., Reference Lee, Pilgrim, Gerostamoulos, Robinson and Wong2018). At high/supratherapeutic dosages, a quetiapine agonist activity on the DA system has been hypothesised (Chiappini and Schifano, Reference Chiappini and Schifano2018). Vulnerable subjects include inmates and those with a previous substance abuse history (Lee et al., Reference Lee, Pilgrim, Gerostamoulos, Robinson and Wong2018) (Table 1).
Olanzapine, at a dosage of up to 50 mg/day, has been anecdotally advised online as the ‘ideal trip terminator’ after a psychedelic drug binge. Moreover, it may be used to treat unwanted ‘comedown’ symptoms (depression, dysphoria, anxiety and insomnia) from drug/alcohol intake (Klein et al., Reference Klein, Bangh and Cole2017; Chiappini and Schifano, Reference Chiappini and Schifano2018) (Table 1).
Gabapentinoids
A rise in pregabalin and gabapentin prescription rates has been registered worldwide, with an anecdotally growing black market (Parsons, Reference Parsons2018). Both gabapentinoids bind to the calcium channel, reducing the release of excitatory molecules. At therapeutic dosages, they are thought to possess GABA-mimetic properties, which may be behind the ‘liking’ (euphoric/relaxing high), but causing only limited rewarding (‘wanting’), dopaminergic-related, properties (Berridge and Robinson, Reference Berridge and Robinson2016; Bonnet and Scherbaum, Reference Bonnet and Scherbaum2017; Bonnet et al., Reference Bonnet, Richter, Isbruch and Scherbaum2018). A range of experiences may be associated with gabapentinoid high-dosage abuse, including euphoria, improved sociability, opiate-like sedation, entactogenic feelings/dissociation and psychedelic effects (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015). Gabapentinoids may be ingested to cope with opiate/opioid withdrawal symptoms (Schifano et al., Reference Schifano, Chiappini, Corkery and Guirguis2018). Unconventional routes of administration have been reported, e.g. intravenous; rectal – ‘plugging’; smoking and ‘parachuting’, e.g. emptying the content of the capsule into a pouch (Chiappini and Schifano, Reference Chiappini and Schifano2016; Al-Husseini et al., Reference Al-Husseini, Van Hout and Wazaify2018). A proper withdrawal syndrome, including insomnia; headache; nausea; anxiety and convulsions, can be associated with gabapentinoids' abrupt discontinuation (Baumeister et al., Reference Baumeister, Tojo and Tracy2015; WHO, 2017) (Table 1).
Z-drugs and designer benzodiazepines
The Z-drugs' (zolpidem, zopiclone and zaleplon) addictive potential has already been highlighted (Kapil et al., Reference Kapil, Green, Le Lait, Wood and Dargan2014; Schifano et al., Reference Schifano, Chiappini, Corkery and Guirguis2019). Zolpidem and zopiclone seem to be the most involved in the diversion and abuse phenomena (ACMD, 2013), and it is likely that the misusing phenomenon is currently underestimated (Hajak et al., Reference Hajak, Müller, Wittchen, Pittrow and Kirch2003). A 20 mg to 300–400 mg/day zolpidem dosage has been associated with significant stimulating effects, hyperactivity and euphoria (Victorri-Vigneau et al., Reference Victorri-Vigneau, Dailly, Veyrac and Jolliet2007) (Table 1). Polydrug consumption and history of drug misuse are frequently reported issues; both snorting and injection practices have been described. A withdrawal syndrome may develop after the abrupt cessation of Z-drugs' long-term, high-dosage, intake and symptoms may include insomnia, anxiety, irritability, tremor, abdominal pain, hypertension, tonic–clonic seizures and confusion.
Designer benzodiazepines recently emerged on the illegal drug scene (EMCDDA, 2017; Graddy et al., Reference Graddy, Buresh and Rastegar2018; Vårdal et al., Reference Vårdal, Wong, Øiestad, Pedersen-Bjergaard, Gjelstad and Øiestad2019). Most of them are not approved for therapeutic use in any country (Baumeister et al., Reference Baumeister, Tojo and Tracy2015; Moosmann et al., Reference Moosmann, King and Auwarter2015) and may be easily acquired online (Vårdal et al., Reference Vårdal, Wong, Øiestad, Pedersen-Bjergaard, Gjelstad and Øiestad2019). Whilst sharing clinical effects with ‘traditional’ molecules (Baumeister et al., Reference Baumeister, Tojo and Tracy2015), some designer benzodiazepines (e.g. pyrazolam; phenazepam/‘Zinnie’) may be several times more potent than diazepam (Moosmann et al., Reference Moosmann, King and Auwarter2015; Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015; Tracy et al., Reference Tracy, Wood and Baumeister2017). Designer benzodiazepines' side-effects include amnesia, long-lasting (60 h) confusion and disorientation, dizziness, loss of coordination, drowsiness, blurred vision, slurred speech and ataxia (Baumeister et al., Reference Baumeister, Tojo and Tracy2015). Due to their high potency, molecules such as clonazolam or flubromazolam can cause strong sedation and amnesia at oral doses as low as 0.5 mg, hence they may be unintentionally overdosed (Moosmann et al., Reference Moosmann, King and Auwarter2015). Etizolam, phenazepam, clonazolam, diclazepam, phenazolam and flubromazolam have all been involved in fatalities (UNODC, 2018a; 2018b) (Table 1).
OTC drugs
Over the last decade, clinicians have raised concerns relating to a range of OTCs being misused recreationally, with ‘pharming’ (e.g. shopping from a range of pharmacy shops) being an internationally recognised issue (Schifano and Chiappini, Reference Schifano and Chiappini2018b). OTC misuse may have developed due to their increased availability, affordability and users' perceptions of their safety (Cooper, Reference Cooper2013; Sansgiry et al., Reference Sansgiry, Bhansali, Bapat and Xu2016). Commonly abused medications include ephedrine and pseudoephedrine; codeine-containing antitussives and dextromethorphan (Cooper, Reference Cooper2013). Codeine diversion has been reported to be associated with sedating effects, whilst its combination with promethazine is known as ‘purple drank’ (Cooper, Reference Cooper2013) (Table 1).
Dextromethorphan (DXM) is a cough suppressant opioid derivative, considered safe at recommended dosages, e.g. 120 mg in four divided doses per day (Linn et al., Reference Linn, Long and Pagel2014). The psychotropic effects and addictive potential are associated with the intake of large dosages, typically administered through snorting or injecting practices. Psychotropic effects include trance-like euphoria/stupor, hyper excitability, depersonalisation, dyskinesia, delayed response times, disordered speech and vivid auditory/visual hallucinations (Romanelli and Smith, Reference Romanelli and Smith2009). Due to the action of DXM's primary metabolite dextrorphan on the NMDA receptor, the compound may produce a ketamine-like dissociative state, known as ‘robo-ing’, ‘robo-copping’ or ‘robo-tripping’, after the DXM-containing cough syrup commercial name (Wilson et al., Reference Wilson, Ferguson, Mazer and Litovitz2011). Moreover, DXM chronic abuse has been associated with psychosis (Linn et al., Reference Linn, Long and Pagel2014). In addition to NMDA receptor antagonist activity, DXM and its metabolite dextrorphan are specific serotonin reuptake inhibitors. As a result, the acute DXM intoxication has been linked to serotonin syndrome, especially if used together with remaining serotonergic agents (Linn et al., Reference Linn, Long and Pagel2014) (Table 1).
Recently, the anti-diarrhoeal opiatergic compound loperamide has been reported for its euphoric effects (Lee et al., Reference Lee, Vera, Alexander, Ruck, Nelson, Wax, Campleman, Brent and Calello2019). At therapeutic dosages (2–16 mg/day), due to both rapid metabolism and poor blood–brain barrier penetration, it is considered safe. However, when self-administered at high dosages (e.g. >50 mg), its μ-opioid receptors' agonist activities explain why ‘lope’, being anecdotally described as ‘better than oxycodone’, has been associated with euphoria, central nervous system depression and fatal cardiotoxicity. Cytochrome inhibitors, such as cimetidine, omeprazole and grapefruit juice, as well as P-glycoprotein inhibitors, such as quinidine-quinine and pepper, may be concomitantly used to raise the drug blood levels (Baker, Reference Baker2007; Schifano and Chiappini, Reference Schifano and Chiappini2018b) (Table 1).
Discussion
The present paper has provided an updated review of both the large number of NPS and their associated psychopathological consequences. In recent years, the large access to the web has led to a gradual, although partial, shift from a ‘street’ to a ‘web’ market (Corkery et al., Reference Corkery, Orsolini, Papanti and Schifano2017). Both the ‘open’ but also the ‘deep web’ and the ‘dark net’ (Orsolini et al., Reference Orsolini, Papanti, Francesconi and Schifano2015), with their fora, blogs, social networks and chat rooms, are in continuous development. These represent large-scale, international, shared platforms that facilitate the occurrence of confidential exchange of drug-related information, but which also directly/indirectly promote the acquisition of a range of new, emerging and untested psychoactive substances (Schifano et al., Reference Schifano, Orsolini, Papanti and Corkery2015). This has facilitated the growth of a completely uncontrolled and ‘quasi-legal’ market for many psychoactive substances. The use of NPS is mostly self-experimental in nature, ad one could argue that the ‘e-psychonauts’ (Orsolini et al., Reference Orsolini, Papanti, Francesconi and Schifano2015) are those who properly shape and influence current and possibly future drug scenarios. Indeed, the e-psychonauts seem to test, and at times synthesise, a range of drugs to achieve the state of consciousness they find most pleasurable (Orsolini et al., Reference Orsolini, Papanti, Francesconi and Schifano2015). It is intriguing that, whilst navigating the online psychonauts' fora with NPS.Finder® (2019), a few thousand NPS were here identified, a number which is about 4-fold higher than what identified by both the EMCDDA (EMCDDA, 2018) and the UNODC (UNODC, 2018a; 2018b). Hence, it is here suggested that carrying out systematic web crawling activities may help in designing and developing a range of NPS-related early recognition and monitoring programmes. Further studies from our group will hopefully better identify: (a) which of the e-psychonauts' molecules will enter the future markets; and (b) which is the time gap, for an index NPS, between the start of the e-psychonauts' interest and the actual identification on the international drug scenarios.
The ever-increasing changes in terms of recreational psychoactives' availability represent a relatively new challenge for psychiatry. These molecules' intake may be risky, and the pharmacodynamics and pharmacokinetics of many NPS are still poorly understood (Schifano et al., Reference Schifano, Papanti, Orsolini and Corkery2016). Overall, the intake of these substances is typically associated with an imbalance of a range of neurotransmitter pathways/receptors, and consequently with the risk of psychopathological disturbances. The occurrence of psychopathological disturbances has been related here to the significant imbalance of a range of neurotransmitters/pathways: (a) increased central dopamine levels, mostly associated with psychedelic phenethylamines and synthetic cathinones; (b) agonist/super agonist cannabinoid CB1 receptor activation, achieved with synthetic cannabimimetics; (c) 5-HT2A receptor activation, reported with latest tryptamine derivatives, DXM and hallucinogenic plants; (d) antagonist activity at NMDA receptors, described with phencyclidine-like dissociatives and (e) k-opioid receptor activation, typically associated with Salvia divinorum intake. As NPS are presumably more often used in hedonistic and sporadic occasions, the acute physical and psychiatric complications are perhaps of special importance compared to the risk of addiction development observed with the traditional illicit psychoactive substances, which are more often used on a daily basis over an extended period of time.
It is difficult for mental health professionals to keep up to date with the growing number of NPS being made available. Clinicians are not always aware of the psychopathological risks relating to NPS intake, and, at the same time, they are not typically able to identify a potential NPS user (Simonato et al., Reference Simonato, Corazza, Santonastaso, Corkery, Deluca, Davey, Blaszko and Schifano2013). This may be a reason for concern, especially for emergency mental health clinicians confronting with acute, and at times dramatic, clinical situations which are suspected of being drug-related but in which the standard urine specimen turns out to be negative. In fact, standard toxicity tests can identify just a few misused molecules and only expensive, lengthy, tests carried out in specialised settings are able to identify the vast range of NPS available (Smith et al., Reference Smith, Sutcliffe and Banks2015). Hence, clinicians should be informed about the range of NPS; their intake modalities; their psychoactive sought-after effects; the idiosyncratic psychotropics' combinations and finally, their psychopathological risks (Orsolini et al., Reference Orsolini, Papanti, Francesconi and Schifano2015). Thus, further research studies should focus on drafting specific guidelines to better help clinicians in treating and managing the acute and long-term psychopathological consequences of NPS intake.




