Introduction
Cognitive theories of obsessive-compulsive disorder (OCD) posit that intrusive thoughts are experienced by most healthy individuals without significant distress or impairment, and suggest that it is the dysfunctional interpretation of such thoughts that results in obsessive-compulsive (OC) symptoms (Rachman, Reference Rachman1997; Salkovskis, Reference Salkovskis1999). The three most prominent belief domains that have been linked to OC symptoms include: responsibility and threat over-estimation (responsibility/threat), or the belief that one has the ability to cause or prevent negative outcomes that are perceived to be severe and probable; perfectionism and intolerance of uncertainty (perfectionism/certainty), or the belief that perfection is achievable and necessary and that uncertainty is threatening and unsafe; and importance and control of thoughts (importance/control of thoughts), or the belief that mental events are morally, psychologically and behaviourally important and that control of thoughts should be achieved [Obsessive Compulsive Cognitions Working Group (OCCWG), 1997, 2005]. Each belief domain has been found to predict specific OC symptoms, including sexual and religious obsessions, washing, checking, doubting and ordering (among others), although these links have been inconsistently supported (Brakoulias et al., Reference Brakoulias, Starcevic, Berle, Milicevic, Hannan and Martin2014; Cordeiro et al., Reference Cordeiro, Sharma, Thennarasu and Janardhan Reddy2015; Myers et al., Reference Myers, Fisher and Wells2008; Siev et al., Reference Siev, Steketee, Fama and Wilhelm2011; Wheaton et al., Reference Wheaton, Abramowitz, Berman, Riemann and Hale2010). While these belief domains are theorized to influence the interpretations and subsequent emotional consequences of intrusive thoughts (OCCWG, 1997), additional mediating factors are probably involved, given the inconsistency of the relationships (Mantz and Abbott, Reference Mantz and Abbott2017).
One intriguing link between belief domains and OC symptoms may be magical thinking, which refers to beliefs about one’s thoughts and behaviours being ‘linked in a way that cannot be rationally explained by physical laws or culturally acceptable explanations’ (Bocci and Gordon, Reference Bocci and Gordon2007). While magical thinking may include religious or spiritual beliefs, it encapsulates a broad spectrum of beliefs, including beliefs in clairvoyance, luck, evil spirits’ influential power, energy transfer, and other paranormal phenomena (Eckblad and Chapman, Reference Eckblad and Chapman1983). Thus, magical thinking is a broader construct than thought–action fusion, which refers to thoughts influencing the likelihood of events (e.g. thinking about a loved one dying in a plane crash increases the likelihood of it happening) or having a moral equivalence to actions (e.g. thinking about physically harming someone is no different from actually assaulting them; Amir et al., Reference Amir, Freshman, Ramsey, Neary and Brigidi2001; Shafran et al., Reference Shafran, Thordarson and Rachman1996). OC beliefs may lead to higher levels of magical thinking due to magical thinking’s likely function as a coping mechanism for handling uncontrollable situations (Moulding and Kyrios, Reference Moulding and Kyrios2006). Specifically, OC beliefs may spur greater perceptions of uncontrollability surrounding an intrusive thought, which then may be partially coped with using magical thinking. In turn, magical thinking may drive specific OCD-relevant responses (e.g. compulsions; Einstein and Menzies, Reference Einstein and Menzies2004). For instance, belief in spirits may justify responding to threatening thoughts by engaging in neutralizing behaviours such as repeating a mantra believed to recruit the help of a particular spirit. Magical thinking may help explain why individuals with elevated obsessive beliefs have higher levels of OC symptoms across several key belief domains. In terms of responsibility/threat, studies have found a link with superstitious thinking, a closely tied construct to magical thinking (Frost et al., Reference Frost, Krause, McMahon, Peppe, Evans, McPhee and Holden1993; Sica et al., Reference Sica, Novara and Sanavio2002). Similarly, responsibility/threat has been found to relate to paranormal beliefs (Yorulmaz et al., Reference Yorulmaz, Inozu and Gültepe2011). Furthermore, it is plausible that people who over-estimate threats may be especially prone to engage in magical thinking because of its perceived ability to help cope with threats. Based on these ideas, we expected magical thinking to mediate the relationship between responsibility/threat and OC symptoms. For the other belief domains, there is also evidence to suggest that magical thinking may mediate the relationship between perfectionism/certainty and OC symptoms. Perfectionism/certainty has also been linked to paranormal beliefs (Yorulmaz et al., Reference Yorulmaz, Inozu and Gültepe2011). Putting more stock into exerting control via magical thinking may minimize the impact of an uncertain, imperfect world. Thus, it is no surprise that increased magical thinking is linked to a number of uncertainty-filled activities, including gambling (Joukhador et al., Reference Joukhador, Blaszczynski and Maccallum2004), investing (Carlson et al., Reference Carlson, Mowen and Fang2009), and sporting events (Burger and Lynn, Reference Burger and Lynn2005). Lastly, in terms of the importance/control of thoughts belief domain, there seemed to be competing evidence for importance/control of thoughts and magical thinking as mediators of the other’s relation to OC symptoms. For example, if one believes that one can use their thoughts to avoid bad luck (i.e. magical thinking), it may only impact OC symptoms according to their beliefs that thoughts may be responsible for determining the outcome of an event (importance/control of thoughts). However, believing that one’s thoughts are important and must be controlled (importance/control of thoughts) may only result in OC symptoms to the extent that they believe their thoughts can be used to control outcomes (magical thinking). As a result, we made no predictions about that relationship and considered this test exploratory.
Method
Participants and procedure
Participants were undergraduates (n = 284; 62.3% female; mean age = 19.12 years; SD = 1.07; 76.4% White) at a large Midwestern university in the United States who participated for course credit as part of a larger study. All measures were approved by the institutional review board, and were administered in-person on a computer using Qualtrics software (Qualtrics, Provo, UT, USA; see Qualtrics, 2019).
Measures
Obsessional Beliefs Questionnaire-44 (OBQ-44; OCCWG, 2005)
The OBQ-44 measures three obsessive belief domains: responsibility/threat, perfectionism/certainty, and importance/control of thoughts (OCCWG, 2005). Example items include ‘When I see any opportunity to do so, I must act to prevent bad things from happening’ (responsibility/threat), ‘If I’m not absolutely sure of something, I’m bound to make a mistake’ (perfectionism/certainty), and ‘For me, having bad urges is as bad as actually carrying them out’ (importance/control of thoughts). The OBQ-44 has been shown to have strong internal consistency, good criterion-related validity and convergent validity, and less evidence of discriminant validity (OCCWG, 2005). Cronbach’s alpha values in the current study were .95 for the total scale, and for the subscales were .89 (responsibility/threat), .92 (perfectionism/certainty) and .88 (importance/control of thoughts).
Illusory Beliefs Inventory (IBI; Kingdon et al., Reference Kingdon, Egan and Rees2012)
The IBI was used to measure magical thinking (Kingdon et al., Reference Kingdon, Egan and Rees2012). In addition to providing a total score, the IBI consists of three subscales: Magical Beliefs, Spirituality, and Internal State and Thought Action Fusion. When calculating a total, we excluded the ‘Internal State and Thought Action Fusion’ subscale from our analyses to avoid redundancy between magical thinking and the belief domain already captured by the importance/control of thoughts subscale from the OBQ-44. This left the subscales of Magical Beliefs and Spirituality that we used to examine the construct of magical thinking. We found the same pattern of results when including the ‘Internal State and Thought Action Fusion’ subscale. There was an indirect effect of responsibility/threat and importance/control of thoughts on OC symptoms via magical thinking and no indirect effect for perfectionism/certainty. The remaining 19 items were used as a measure of magical thinking. Example items include ‘Most things that happen to us are the result of fate’ (Magical Beliefs) and ‘There is an invisible force guiding us all’ (Spirituality). The IBI has strong test–retest reliability and convergent validity, and acceptable levels of internal consistency (Kingdon et al., Reference Kingdon, Egan and Rees2012; Shihata et al., Reference Shihata, Egan and Rees2014). Cronbach’s alpha for the current study was .84.
Obsessive-Compulsive Inventory-Revised (OCI-R; Foa et al., Reference Foa, Huppert, Leiberg, Langner, Kichic, Hajcak and Salkovskis2002)
The OCI-R is an 18-item measure of six common categories of OC symptoms (Foa et al., Reference Foa, Huppert, Leiberg, Langner, Kichic, Hajcak and Salkovskis2002). Example items include ‘I check things more often than necessary’ and ‘I sometimes have to wash or clean myself simply because I feel contaminated’. The OCI-R has strong internal consistency, good test–retest reliability and convergent validity, and mixed evidence for discriminant validity that depends upon the relevant problem area (Abramowitz and Deacon, Reference Abramowitz and Deacon2006; Foa et al., Reference Foa, Huppert, Leiberg, Langner, Kichic, Hajcak and Salkovskis2002). Cronbach’s alpha for the current study was .89.
Analytic plan
For analyses, we conducted a series of mediation models using Model 4 of Hayes’ PROCESS Macro (Hayes, Reference Hayes2017). To test our hypotheses, we examined the size and significance of the estimated indirect effect of OC beliefs on OC symptoms through magical thinking (i.e. an OC belief domain predicts magical thinking, which in turn predicts OC symptoms). Thus, our primary analysis tested three different mediation models, one for each belief domain. As a check on the directionality of the results, we conducted additional mediation analyses that switched the order of OC beliefs and magical thinking. In other words, these models examined the estimated indirect effect of magical thinking on OC symptoms through OC beliefs (i.e. magical thinking predicts the OC belief domains, which in turn predicts OC symptoms). We ran four models that tested both directions with the OC beliefs entered simultaneously. We ran three models with each obsessive belief domain entered as the independent variable, magical thinking as the mediating variable, OC symptoms as the outcome variable, and the other two beliefs entered as covariates. Finally, we ran a model with all three beliefs entered simultaneously as mediators of the relationship between magical thinking and OC symptoms. Each analysis was run with 10,000 bootstraps and with 95% confidence intervals. All variables were standardized.
Results
Table 1 displays the correlations among OC beliefs, magical thinking, and OC symptoms, as well as the means and standard deviations.
Table 1. Means, standard deviations, and bivariate correlations
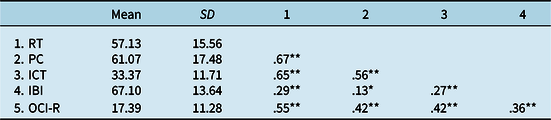
RT, responsibility/over-estimation of threat; PC, perfectionism/intolerance of uncertainty; ICT, importance/control of thoughts; IBI, Illusory Beliefs Inventory; OCI-R, Obsessive-Compulsive Inventory-Revised; *p < .05; **p < .01.
The indirect effects of OC belief domains on OC symptoms via magical thinking
Responsibility and threat over-estimation
We first examined the indirect effect of responsibility/threat on OC symptoms through magical thinking. As seen in Fig. 1, greater responsibility/threat predicted greater magical thinking [β = .20, SE = .06, CI (.09, .32), p < .001], and greater magical thinking predicted greater OC symptoms [β = .18, SE = .05, CI (.08, .28), p < .001]. Critically, as expected, there was a significant indirect effect of responsibility/over-estimation on OC symptoms through magical thinking [indirect effect = .04, CI (.01, .07), P M = .07].
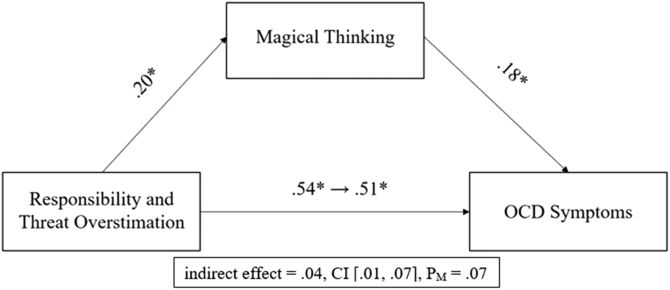
Figure 1. Magical thinking as a mediator of the relationship between responsibility and threat over-estimation and OC symptoms. Values represent standardized beta values. *p < .001.
Perfectionism and intolerance of uncertainty
Unlike responsibility/threat, perfectionism/certainty did not predict magical thinking [β = .06, SE = .06, CI (–.06, .18), p = .30; see Fig. 2]. As before, greater magical thinking predicted greater OC symptoms [β = .26, SE = .05, CI (.16, .36), p < .001]. Contrary to our hypothesis, there was no indirect effect of perfectionism/certainty on OC symptoms through magical thinking [indirect effect = .02, CI (–.02, .06), P M = .04].
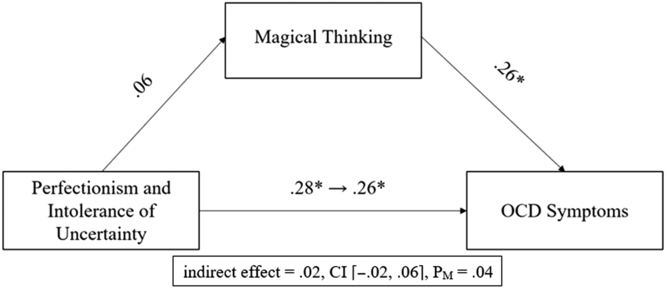
Figure 2. Magical thinking as a mediator of the relationship between perfectionism and intolerance of uncertainty and OC symptoms. Values represent standardized beta values. *p < .001.
Importance and control of thoughts
As seen in Fig. 3, greater importance/control of thoughts predicted greater magical thinking [β = .22, SE = .06, CI (.10, .34), p < .001], and greater magical thinking predicted greater OC symptoms [β = .20, SE = .05, CI (.10, .31), p < .001]. For this domain which did not have a hypothesis, there was an indirect effect of importance/control of thoughts on OC symptoms through magical thinking [indirect effect = .04, CI (.01, .08), P M = .10]. Thus, across the three beliefs domains we found indirect effects of responsibility/threat and importance/control of thoughts through magical thinking, but not perfectionism/certainty.
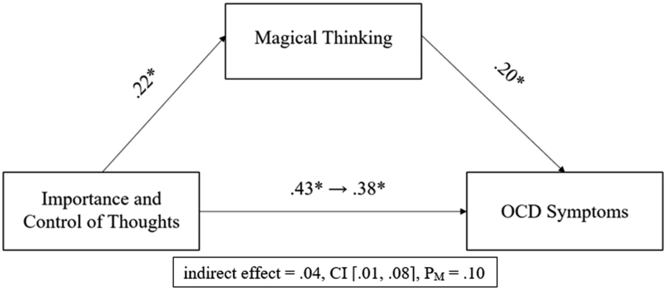
Figure 3. Magical thinking as a mediator of the relationship between importance and control of thoughts and OC symptoms. Values represent standardized beta values. *p < .001.
Finally, as a check on the directionality of the original models, we examined the three reversed models testing the indirect effects of magical thinking on OC symptoms via the three obsessive belief domains. We found significant indirect effects for the models examining responsibility/threat [indirect effect = .10, CI (.04, .16), P M = .36], and importance/control of thoughts [indirect effect = .08, CI (.03, .14), P M = .28], as mediators, but not for perfectionism/certainty [indirect effect = .02, CI (–.03, .08), P M = .09]. Thus, for both of the belief domains that had demonstrated indirect effects with magical thinking as a mediator, the same was true when obsessive beliefs were the mediators. For the four simultaneous models, the results paralleled those listed above with the exception being that there was no indirect effect of importance/control of thoughts in the relationship between magical thinking and OC symptoms.
Discussion
In the present study, we evaluated whether magical thinking indirectly linked obsessive belief domains (responsibility/threat, perfectionism/certainty, and importance/control of thoughts) and OC symptoms, finding partial support for our hypotheses. There were indirect effects flowing through magical thinking for both responsibility/threat and importance/control of thoughts beliefs, supporting the idea that magical thinking may partially explain previous inconsistency in the relationship between OC beliefs and OC symptoms. These findings give credence to proposals that magical thinking may be used by individuals to maintain control (Moulding and Kyrios, Reference Moulding and Kyrios2006), given that individuals with higher responsibility/threat and importance/control of thoughts are prone to feeling less control (Moulding and Kyrios, Reference Moulding and Kyrios2007). Magical thinking did not mediate the relationship between perfectionism/certainty and OC symptoms and in fact was unrelated to perfectionism/certainty, which is somewhat surprising given past links between these constructs (Keinan, Reference Keinan1994; Yorulmaz et al., Reference Yorulmaz, Inozu and Gültepe2011). Nevertheless, this finding is congruent with other work not finding a link between perfectionism and superstition (Sica et al., Reference Sica, Novara and Sanavio2002) in which the authors speculated that the OBQ may not fully capture the pathological side of perfectionism. For example, magical thinking may only be tied to perfectionism when perfectionism revolves around negative outcomes (Terry-Short et al., Reference Terry-Short, Owens, Slade and Dewey1995). In these cases, magical thinking would emerge due to a perceived function of preventing such outcomes. Belief in a higher power or in luck may be deemed advantageous when one feels limited capability to change their environment (Rothbaum et al., Reference Rothbaum, Weisz and Snyder1982). Another possibility is that the link between perfectionism/certainty and magical thinking may not be linear. For example, Keinan (Reference Keinan1994) found that uncertainty interacted with stress to predict even higher levels of magical thinking. Perhaps, environmental stressors play a pivotal role in predicting magical thinking. Future work should examine whether other risk factors explain the relationship between perfectionism/certainty and OC symptoms, and if any of the risk factors work in conjunction with magical thinking to heighten symptoms.
As part of our analyses, we also checked whether OC belief domains mediated the relationship between magical thinking and OC symptoms. While the current study aligned with past research by finding magical thinking to be a significant predictor of OC symptoms (Einstein and Menzies, Reference Einstein and Menzies2004; Kingdon et al., Reference Kingdon, Egan and Rees2012), we found that magical thinking only accounted for a small portion of the association between both responsibility/threat and importance/control of thoughts, and OC symptoms. In contrast, the proportion of the total effect accounted for by responsibility/threat in the reversed model (i.e. 30%) was more substantial. Furthermore, all three of the OC belief domains we tested were robust predictors of OC symptoms, which is consistent with some past research and theory but is not always found (Freeston, Rhéaume, & Ladouceur, Reference Freeston, Rhéaume and Ladouceur1996; OCCWG, 2005; Salkovskis, Reference Salkovskis1985). Although causality cannot be determined due to the cross-sectional design, the direct and indirect effects we found largely support cognitive theories of OCD which emphasize the role of beliefs in leading to OC symptoms. It may be the case that believing that thoughts can subvert harm (i.e. magical thinking) leads to an inflated sense of responsibility, which in turn leads to neutralizing behaviour. In addition to the current mediation analyses, it will be important for future work to elucidate the extent to which OC beliefs are necessary for magical thinking to predict OC symptoms (i.e. do OC beliefs moderate the relationship between magical thinking and OC symptoms?), and to examine how their attenuation impacts the association between magical thinking and OC symptoms. Furthermore, more complicated models that include additional variables (e.g. stress, perceived ability to cope) may increase our understanding of these relationships. For example, those who over-estimate threats may be especially prone to engage in magical thinking due to the elevated distress they may feel when over-estimating threats. Distress is commonly experienced when one’s perceived ability to cope with a threat is diminished (Bandura, Reference Bandura1988; Wiedenfeld et al., Reference Wiedenfeld, O’Leary, Bandura, Brown, Levine and Raska1990) and magical thinking is a typical response to loss of control (Case et al., Reference Case, Fitness, Cairns and Stevenson2004). Past research on Israelis under the threat of missile attacks during the Gulf War (i.e. a stressful and uncertain situation) found that they endorsed higher levels of magical thinking, particularly when their reported ability to tolerate the uncertainty was low (Keinan, Reference Keinan1994). Thus, magical thinking may be more likely used as a coping mechanism under stressful and uncertain situations, when an alternative coping mechanism is not seen as being viable (Rothbaum et al., Reference Rothbaum, Weisz and Snyder1982).
While the cross-sectional design prohibits us from inferring causation for either directional model, it is interesting to consider these relationships for future, temporal tests. A bidirectional relationship may exist, in which increases in responsibility/threat lead to increases in magical thinking, and vice versa, with both magical thinking and responsibility/threat in turn leading to increases in OC symptoms. It also remains possible that OC beliefs, magical thinking and OC symptoms operate in a cyclical pattern. The non-occurrence of a feared outcome after OC symptom behaviours like neutralizing and/or checking may serve to reinforce the importance of controlling one’s thoughts and magical thinking. Thus, future work should examine how these variables influence each other temporally. Additionally, the idiosyncratic nature of OC beliefs and symptomatology may be better captured by intra-individual approaches.
In addition to the cross-sectional design, other limitations deserve mentioning. First, we measured obsessive beliefs using the OBQ-44, which collapses six beliefs into three domains (OCCWG, 2005). As other work has suggested that some of these beliefs should be measured separately (e.g. Moulding et al., Reference Moulding, Anglim, Nedeljkovic, Doron, Kyrios and Ayalon2011), it is possible that our results would have changed if we had tested our hypotheses with each individual belief. Second, we used an undergraduate sample that was fairly homogenous in terms of age and race. Future research should look to enhance the generalizability of these results by examining these variables in more racially and age diverse samples, as well as in different cultures and clinical samples.
Conclusion
The current study examined the relationship between OC belief domains, magical thinking, and OC symptoms. Limitations notwithstanding, this study found that the relationships between some OC belief domains and symptoms partially flow through magical thinking. If magical thinking is indeed as pernicious to the effectiveness of psychosocial interventions as has been suggested, then clarifying the directionality between magical thinking and different OC belief domains will be helpful in informing interventions (Einstein and Menzies, Reference Einstein and Menzies2008; Freeston et al., Reference Freeston, Rhéaume and Ladouceur1996).
Acknowledgements
The authors would like to thank Kate Freeman, Marcia Kantrow, Erin Shelton, Abigail Wenger and Cassandra Woodford for their help with data collection.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The authors have no conflict of interest with respect to this publication.
Ethical statements
The authors have conducted this research in concordance with the Ethical Principles of Psychologists and Code of Conduct (American Psychological Association, 2017)







Comments
No Comments have been published for this article.