Anomalous origin of one pulmonary artery from the ascending aorta is a rare cardiac anomaly in which the pulmonary artery abnormally arises from the ascending aorta. Physiologically, most patients develop signs of cardiac failure due to high flow to lung that is perfused by the abnormal artery. The purpose of this study is to demonstrate, with this rare anomaly, the accurate place of the echocardiography to establish diagnosis especially in the systemic or supra-systemic pulmonary hypertension.Reference Amir, Frenkel and Bruckheimer1
Case report
A 5-month-old baby was discharged from our department for severe respiratory distress with pulmonary hypertension. An already made echocardiography, done 2 weeks ago, did not show cardiac malformation, just a pulmonary hypertension related to respiratory origin.
The infant was delivered normally at term with normal birth weight, and has history of cyanosis related mainly to crying and feeding since few days after birth.
On clinical examination, a soft 2/6 holo-systolic murmur was found, femoral pulse present, with hepatomegaly and polypnoea, oxygen saturation 88% in upper left arm. Lung sounds were within normal limits in all fields, heart rate (160 bpm), respiratory rate (40 breaths/minute), and temperature were within normal.
Chest radiographs revealed cardiomegaly, with an interstitial pulmonary pattern most pronounced in the right lung lobes.
Echocardiography with multiple views shows different futures exposed just below:
A high short axis view showed the origin of the right pulmonary artery to be from the posterior side of the ascending aorta, this anomalous pulmonary branch has normal aspect without stenosis anatomy of the pulmonary trunk and left branch was without anomaly.
A suprasternal view visualised the right side of the aorta, the absence of the ductus arteriosus, collaterals arteries, coarctation or interruption of the aorta.
Subcostal and apical scans showed normal intracardiac anatomy, the absence of shunt or outflow obstruction, right ventricle dilatation, and tricuspid regurgitation with severe pulmonary hypertension.
In the left parasternal short axis view, the pulmonary artery is discontinuous and the right bifurcation of main pulmonary artery is not seen with Doppler and 2D echo.
The parasternal long-axis view of the heart revealed an enlarged left atrium and left ventricle, normal mitral valve anatomy, and pulmonary veins direction.
Therapy with titrated oxygen, diuretic, and captopril was initiated with partial improvement. After, the baby was intubated and ventilated because his condition has worsened. He died later.
Discussion
Anomalous origin of the right pulmonary arteries arising from the ascending aorta, also called hemitruncus, is a very rare CHD. The diagnosis is well far established by two-dimensional echocardiography, under the condition of thinking and taking necessary time.Reference Erdem, Aydemir and Demir2, Reference Hadeed, Ohanessian and Acar3
Unfortunately, this diagnosis should be established at the first time, because, before thinking to the pulmonary hypertension related to respiratory infection, the physician must exclude congenital heart malformation, and the hemitruncus is one such disease. In the same condition, we must rule out the lung over-vascularisation such as Patent duct arteriosus (PDA), major collateral vessel between the systemic and pulmonary circulation, and truncus arteriosus.
The morphology of the anomalous pulmonary artery is constant: it originates from the wall of the ascending aorta, 5–30 mm above the ventriculo-arterial junction juxta-proximal to the right brachio-cephalic trunk.
Anomalous origin of the right pulmonary arteries arising from the ascending aorta should not be confused with aorto-pulmonary window, which demonstrates normal pulmonary artery bifurcation of the main pulmonary artery in the high left parasternal window.Reference King, Huhta, Gutgesell and Ott4
The detailed main pulmonary artery with each branch, and the continuity between ascending aorta and the right pulmonary artery should be done with multiple acoustic windows. Especially the image from the high short axis view, high left parasternal and suprasternal window. The pulmonary artery is discontinuous and the bifurcation of the main pulmonary artery is not seen from any angle, and the right sidedness and the PDA are usually contra-lateral to the anomalous pulmonary artery. The absence of pulmonary artery branch is usually on the opposite side of the aortic arch.Reference King, Huhta, Gutgesell and Ott4, Reference Duncan, Freedom, Olley and Rowe5, Reference Santos and Azevedo6 By the suprasternal view, we must exclude coarctation or interruption of the aorta. In addition, associated lesions should be eliminated such as tetralogy of Fallot, Ventricular septal defect, or Atrial septal defect.Reference Hadeed, Ohanessian and Acar3, Reference Santos and Azevedo6, Reference Lai, Mertens, Cohen, Geva, Wyman, Mertens, Meryl Cohen and Geva7
Echocardiography diagnosis is established by:
Demonstrating two flow separating ventricular outflow tract and semilunar valves.
There is continuity between the main pulmonary arteryand left pulmonary artery, and continuity between the ascending aorta and the right pulmonary artery.
The echogram typically exhibits the evidence of pulmonary hypertension.
It is imperative to be sure that branch pulmonary arteries and their origins are clearly defined in such case echo-free space in its place that gives the appearance of the artery.
The absence of colour flow in this echo-free space (Fig 1).
The presence of the pulmonary branch arises just above the semilunar valve (Fig 2) or distant from this.
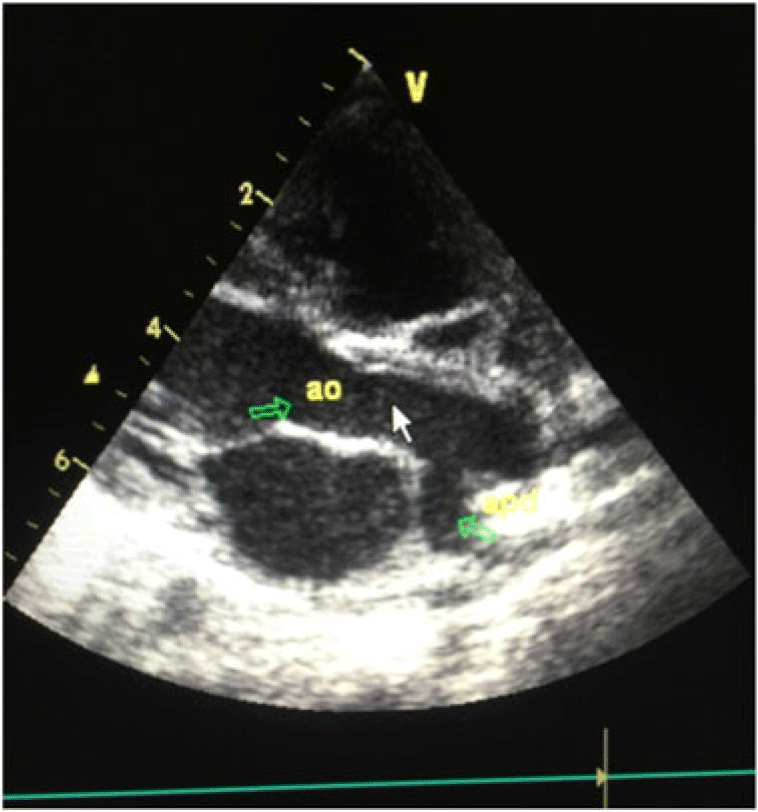
Figure 1. The pulmonary artery is discontinuous, the absence of colour flow in this echo-free space.

Figure 2. The presence of the pulmonary branch arises just above the semilunar valve.
As diagnosis is established, the oxygen should be avoided if possible. Surgery should be performed as soon as possible. The patient should underwent immediate and complete surgical repair, consisting of detachment of the anomalous pulmonary artery from the ascending aorta with direct anastomosis to the main pulmonary artery.
Conclusion
This case shows that one diagnosis which should be excluded before retain respiratory HTAP origin is hemitruncus, performing detailed echocardiography should guarantying good management. This pathology should be diagnosed in case of heart failure with increased blood flow. Unless surgically repaired, this condition is fatal in the most cases.
Acknowledgements
The authors would like to thank Khadija Qadida for the support.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.




