Introduction
Autologous cartilage is widely used in rhinoplasty and possesses several characteristics of an ideal graft. It is easy to shape and can be readily harvested from the patient. Moreover, autologous cartilage usually lacks local tissue reaction and is relatively resistant to resorption.Reference Lovice, Mingrone and Toriumi 1 – Reference Grobbelaar, Matti and Nicolle 3 Autologous cartilage can be harvested from the septum, auricle or rib. Septal cartilage is the most commonly used site, followed by conchal and costal cartilage.Reference Sajjadian, Rubinstein and Naghshineh 2 When septal cartilage is not available or is insufficient, conchal cartilage represents an ideal alternative source for autologous cartilage.Reference Wright, Calhoun, Decherd and Quinn 4 – Reference Mowlavi, Pham, Wilhelmi, Masouem and Guyuron 6
Conchal cartilage can be used in several applications in rhinoplasty, such as a tip graft, dorsal graft, radix graft or columellar strut.Reference Boccieri and Marano 5 , Reference Han, Kim, Son and Park 7 The histological characteristics of its elasticity and inherent curvature make conchal cartilage the ideal graft for tip surgery, including onlay graft, shield graft and lateral crural graft.Reference Jang and Jang 8 It also has been successfully used for correcting nasal valve collapse and for partial dorsal augmentation.Reference Jang and Jang 8
Although conchal cartilage is a favourable graft in rhinoplasty, complications, such as haematoma, keloid formation and ear deformity, can still arise.Reference Sajjadian, Rubinstein and Naghshineh 2 – Reference Wright, Calhoun, Decherd and Quinn 4 , Reference Jang and Jang 8 However, little information regarding the incidence of donor site morbidities has been reported to date.Reference Grobbelaar, Matti and Nicolle 3 , Reference Wright, Calhoun, Decherd and Quinn 4 , Reference Jovanovic and Berghaus 9 This article aimed to investigate the incidence of donor site complications associated with conchal cartilage harvesting in rhinoplasty.
Materials and methods
Patients
This was a retrospective medical records review of 372 patients who underwent conchal cartilage harvesting for rhinoplasty at Asan Medical Centre between March 2002 and December 2013. The study was approved by our Institutional Review Board and informed consent was obtained from all patients. The post-operative follow-up period ranged from 2 to 66 months (mean, 12.7 months). Data regarding patient demographics, types of nasal deformities and complications were collected.
Surgical techniques
All rhinoplasties were performed by the senior author (YJJ). All patients were operated under general anaesthesia, except four patients who underwent surgery under local anaesthesia. Most patients underwent an open rhinoplasty technique. Only seven patients underwent an endonasal approach. Most patients received the posterior approach for the conchal cartilage harvesting, while some received the anterior approach.
Statistical analyses
Numerical data are presented as means ± standard deviations, and categorical variables are shown as percentages. The Mann–Whitney U test was used to compare non-parametric variables. The chi-square test or Fisher's exact test were used for categorical variables. Statistical analyses were performed using SPSS® version 12.0 software. We used p < 0.05 as a threshold for identifying statistically significant differences.
Results
A total of 372 patients underwent conchal cartilage harvesting for rhinoplasty; there were 247 (66.4 per cent) male and 125 (33.6 per cent) female patients. Demographic data for the patients are summarised in Table I. The patients’ average age was 33.98±11.73 years (range, 17–74 years). The average age of the male patients was 33.81±11.64 years (range, 18–72 years) and the average age of the female patients was 34.32±11.93 years (range, 17–74 years). This difference in age was not statistically significant (p > 0.05). Among all 372 patients, 66 (32 males and 34 females) were revision rhinoplasty cases. The most frequent external nasal deformity was a deviated nose (n = 253), followed by hump nose (n = 82) and low profile nose (n = 78) (Table I).
Table I Demographic and clinical characteristics of study cohort

SD = standard deviation
There were nine patients (2.4 per cent) with donor site morbidities that were observed during the follow-up period, including four patients (1.1 per cent) with keloids (Figure 1) and five patients (1.3 per cent) with haematomas (Figure 2 and Table II). Interestingly, all patients with keloids were young males who underwent the posterior approach. However, there were no statistically significant differences in sex, age or approach method between the patients with and without keloids (Table II).
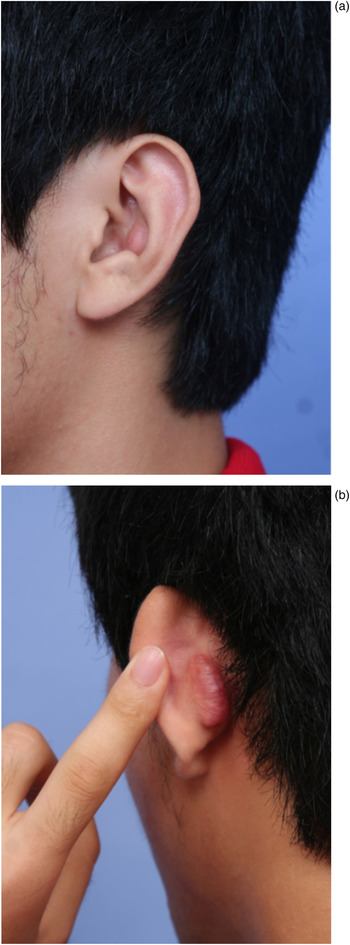
Fig. 1 (a) Anterior and (b) posterior views of the auricle keloid of a patient who underwent conchal cartilage harvesting in rhinoplasty.

Fig. 2 (a) Anterior and (b) posterior views of the auricle haematoma of a patient who underwent conchal cartilage harvesting in rhinoplasty (red arrow indicates haematoma location).
Table II Complications associated with graft use

We treated three of these patients with keloids by surgical excision followed by steroid injection. One patient with a small keloid refused surgical excision and was treated with steroid injection alone. There was residual keloid in two patients, who both required additional treatment. Among five patients with auricle haematoma, including three males and two females, four were treated with incision and drainage, while one was treated with compression alone. There were no cases of post-operative donor site infection.
Discussion
The conchal cartilage is the most favourable tissue for autologous cartilage harvesting for some Asian patients or for revision rhinoplasty patients who have an insufficient amount of septal cartilage for nasal reconstruction.Reference Wright, Calhoun, Decherd and Quinn 4 – Reference Jang and Jang 8 It is an option for nasal tip grafting. Its elastic characteristic provides a high degree of flexibility, but without the warping tendency usually apparent in costal cartilage.Reference Boccieri 10
The superior cymba and inferior cavum, which are divided by the conchal extension of the helical crus, represent the two components of the conchal bowl.Reference Mowlavi, Pham, Wilhelmi, Masouem and Guyuron 6 The cavum and the cymba, the widest but thinnest cartilage region, are both excellent options for a tip or alar rim graft.Reference Mowlavi, Pham, Wilhelmi, Masouem and Guyuron 6 A thicker graft, such as a spreader or columellar strut graft, can be harvested from the extension of the helical crus.Reference Mowlavi, Pham, Wilhelmi, Masouem and Guyuron 6 In the current study, the conchal cartilage was most frequently used in tip grafting, followed by dorsal grafting, septal reinforcement and the correction of nostril asymmetry. For 50 cases, we used conchal cartilages in more than 1 site for nasal reconstruction.
Only a few papers to date have described the incidence of donor site morbidity resulting from conchal cartilage harvesting (Table III).Reference Grobbelaar, Matti and Nicolle 3 , Reference Wright, Calhoun, Decherd and Quinn 4 , Reference Han, Kim, Son and Park 7 , Reference Jovanovic and Berghaus 9 Complications include hypertrophic scarring, keloids, haematomas, delayed wound healing, infection and asymmetry of the ears.Reference Grobbelaar, Matti and Nicolle 3 , Reference Wright, Calhoun, Decherd and Quinn 4 Grobbelaar et al. reported four complications (9.09 per cent) in their case series: one patient had a hypertrophic scar, two patients had delayed wound healing and one patient had flattening of the ear after surgery.Reference Grobbelaar, Matti and Nicolle 3 Jovanovic and Berghaus reported two complications (6.2 per cent) in their series: one patient had seroma formation and one had a small perforating auricular defect.Reference Jovanovic and Berghaus 9 In the studies by Wright et al.Reference Wright, Calhoun, Decherd and Quinn 4 and Han et al.,Reference Han, Kim, Son and Park 7 no complications were reported for conchal cartilage harvesting in rhinoplasty. In the current study, among 372 patients, there were 9 patients (2.4 per cent) for whom donor site morbidities were observed, including 4 patients (1.1 per cent) with keloids and 5 patients (1.3 per cent) with haematomas. No infections were recorded in our series. To the best of our knowledge, our study reports on the largest series of cases to date to assess donor site morbidities associated with conchal cartilage harvesting in rhinoplasty.
Table III Summary of donor site morbidities in different studies

Leaving the helical buttress intact in the conchal area to support the remaining cartilage can prevent ear deformities after harvesting conchal cartilage.Reference Grobbelaar, Matti and Nicolle 3 , Reference Mowlavi, Pham, Wilhelmi, Masouem and Guyuron 6 – Reference Jang and Jang 8 Adams suggested that at least 2 mm of the superior outer rim of the concha, 3 mm of the cartilage rim connecting the tragus to the antitragus, and 3 mm distal to the rim of the external auditory meatus should be left intact to prevent a noticeable change in the conchal cavity of the donor ear.Reference Adams 11 Falces and Gorney recommended that the anti-helical ridge must remain unviolated even if the entire concha is removed.Reference Falces and Gorney 12 In the current study, there were no ear deformities, because we preserved the antihelix, antitragus, inferior crus of antihelix, crus of helix, and the junction of the cavum and external auditory meatus during the surgery.
However, there were still five cases of haematoma in our study. Meticulous haemostasis and a carefully contoured compressive dressing are the two precautionary key steps to prevent post-operative haematoma formation. When such a situation is encountered, the haematoma should be evacuated immediately and then pressure should be reapplied.Reference Grobbelaar, Matti and Nicolle 3 , Reference Mowlavi, Pham, Wilhelmi, Masouem and Guyuron 6 , Reference Jang and Jang 8 However, too much pressure on the bolster dressing over the conchal skin may cause ischaemic injury of the epidermis, which results in discoloration of the conchal skin as was noted in three cases in our study.
We identified four patients with keloids in our present series. A keloid is a type of scar that is thought to be caused by a stimulus that results in the uncontrolled upregulation of collagen and extracellular matrix expression.Reference Song 13 In our analyses, although there was no statistical difference in the sex of patients with or without keloids, a trend for male predominance was observed. Park et al. also found that males with keloids outnumbered females with keloids among their patients who underwent conchal cartilage harvesting.Reference Park, Park, Kim, Seo, Rah and Chang 14 They concluded that male gender was a possible risk factor for keloid formation after conchal cartilage harvesting.
Erol stated that there were no hypertrophic scars or keloid formations in a series of 250 patients who received secondary rhinoplasties after conchal cartilage harvesting using the anterior approach.Reference Erol 15 They proposed that the main advantage of the anterior approach is the preservation of neurovascular structures on the posterior side of the auricle.Reference Erol 15 Keloid formation rates have been reported to range from 0.7 per cent to 11 per cent using the posterior approach for otoplasty.Reference Furnas 16 Erol proposed that the absence of subcutaneous fat tissue on the anterior side of auricle skin might be the reason for the reduced incidence of keloid formation on that side compared to the posterior side of the auricle skin.Reference Erol 15 In the current study, we preferred to use a posterior approach in the majority of cases because noticeable scar formations over the anterior surface of auricles were observed in some patients who underwent conchal cartilage harvesting via an anterior approach. Interestingly, patients treated by an anterior approach did not have post-operative keloids in our present series.
-
• Conchal cartilage harvesting is a safe technique for rhinoplasty
-
• It is associated with a low incidence of complications such as keloids and haematomas
The cosmetic deformity caused by the keloid usually results in a significant burden for the patient. However, the treatment of keloids remains challenging, even for an experienced surgeon.Reference Song 13 The recurrence rate of keloids after surgical excision alone has been reported to be up to 80–100 per cent.Reference Cosman and Wolff 17 Many adjuvant treatments after surgical excision of a keloid have been proposed, including intralesional steroid injection, radiation treatment, laser treatment, pressure therapy and cryotherapy.Reference Naylor and Brissett 18 In the study of Park et al., auricular keloids were successfully treated in 93.3 per cent of patients who underwent surgical excision followed by adjuvant pressure therapy using a pair of magnets; in that series, 6.7 per cent of patients had recurrences.Reference Park, Park, Kim, Seo, Rah and Chang 14 In the current investigation, three patients were initially treated with surgical excision followed by steroid injection, and one patient with a small keloid who refused surgical excision was treated with steroid injection alone. However, residual keloids were observed in two patients who received additional treatments.
Conclusion
Based on our experience with conchal cartilage harvesting in rhinoplasty, we contend that it is a safe and straightforward technique, with a low complication rate. However, patients should still be informed, prior to surgery, about the possibility of donor site morbidities, such as keloids and haematomas, which are associated with this procedure.







