Introduction
The incidence of thyroid carcinoma has been increasing worldwide, with more than 62 000 new cases diagnosed in the USA in 2015.Reference Cabanillas, McFadden and Durante1 Differentiated thyroid carcinoma is the most common type of thyroid carcinoma, and papillary thyroid carcinoma is the most common subtype.Reference Cabanillas, McFadden and Durante1 Surgery is the primary treatment, although its extent remains controversial. In particular, because of the delicate structures contained within the neck, and risks of recurrent laryngeal nerve injury and hypoparathyroidism, prophylactic neck dissection of the central compartment remains a difficult procedure.Reference Haugen, Alexander, Bible, Doherty, Mandel and Nikiforov2–Reference Feng, Pan, Wang, Ye, Jiang and Qu4
Adequate removal of central neck lymph nodes has been successfully described by Orloff and Kuppersmith,Reference Orloff and Kuppersmith5 who aimed to remove all lymph nodes at major risk of metastasising. In the context of central neck dissection terminology and classification for thyroid cancer, the central neck compartment can be divided into the following four anatomical areas: A, the Delphian and prethyroidal lymph nodes contained in the region of the neck, commonly defined as the muscular linea alba, superficial to the thyroid capsule and cartilage; B/D, deep lymph nodes contained in the adipose tissue on the right (B) and left side (D) of the trachea, where the recurrent nerve emerges from the deep layers and runs medially toward the cricoid cartilage until its entrance into the cricothyroid membrane; and C, deep pretracheal nodes present in the adipose tissues, bound superficially by the strap muscles, deeply by the pretracheal fascia, cranially by the thyroid isthmus and caudally by the thymus horn.Reference Orloff and Kuppersmith5
Previous reports have already described the surgical technique for central neck dissection, but the fine details have not been provided and are still the prerogative of the expert surgeon. The current work aimed to provide a high-quality, pictorial, step-by-step description of dissection of the central neck compartment, to increase understanding of this region's anatomy and its delicate contents, for both resident surgeons and those unfamiliar with these anatomical specifications.
Materials and methods
A detailed description of the surgical technique for central neck dissection was supported by highly representative iconographic materials from a tertiary department.
All patients provided informed consent to allow use of their data (including iconographic materials) for scientific purposes, and the work was carried out in accordance with the Declaration of Helsinki.
Surgical technique
Step one
The patient's head is overextended with the assistance of a soft pillow placed underneath the shoulders at the level of an imaginary line passing between the two scapular crests. The cervical incision is performed at the level of a natural skin crease, about 1 cm below the inferior border of the cricoid cartilage. The platysma flap is raised superiorly and inferiorly until the superficial cervical fascia is exposed (Figure 1).

Fig. 1. (a) Cervical incision performed about 1 cm below the inferior border of the cricoid cartilage. (b) The platismatic flap is raised superiorly and inferiorly to expose the superficial cervical fascia.
Step two
The cervical fascia is incised medially, and the linea alba and medial border of the sternohyoid muscles are identified. The dissection proceeds along the medial border of the strap muscles bilaterally until it reaches the thyroid capsule, thus removing area A (the Delphian and prethyroidal lymph nodes contained in the neck region, superficial to the thyroid capsule and cartilage), including the Delphian and prelaryngeal lymph nodes anterior to the cricothyroid membrane (Figures 2 and 3).
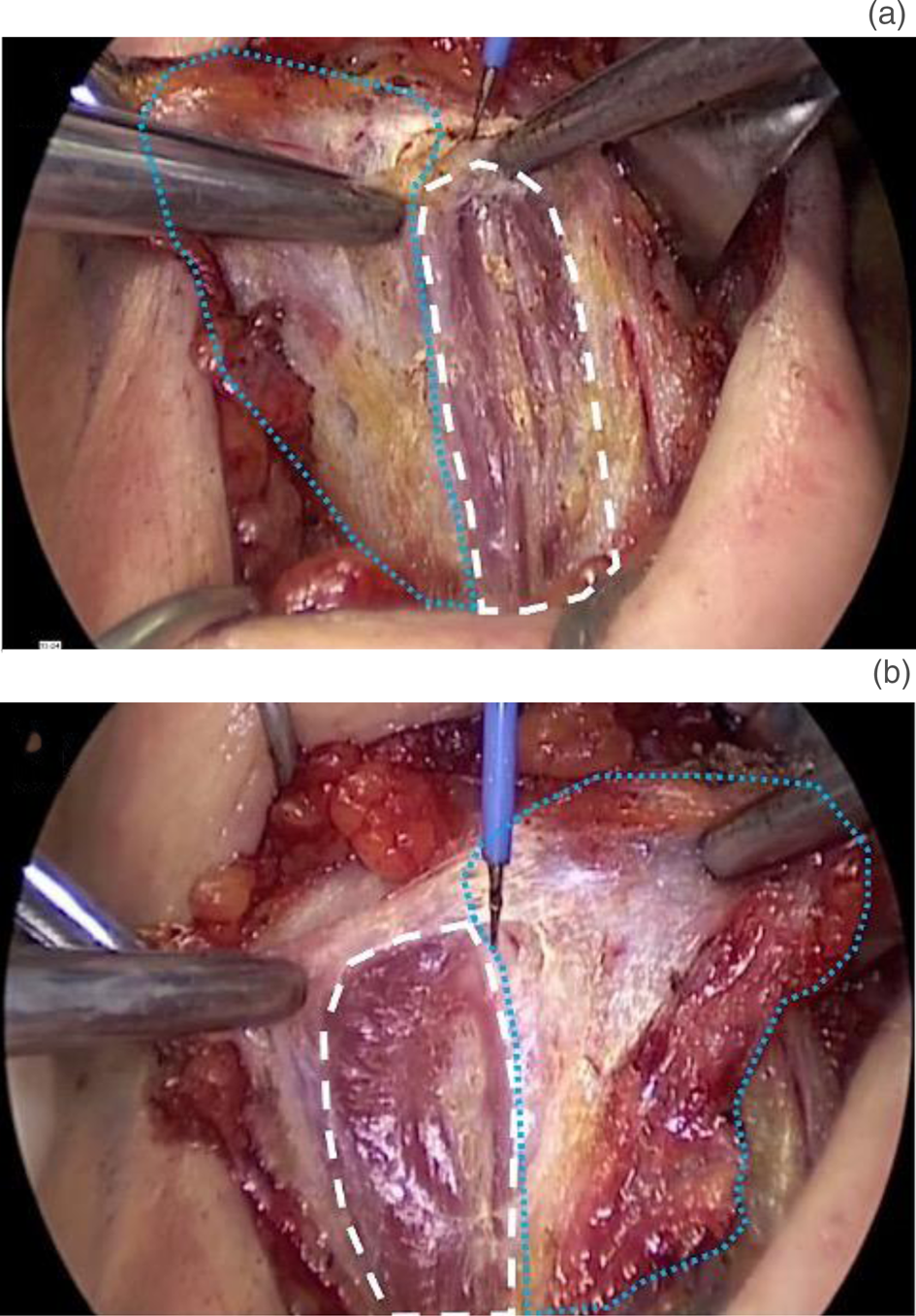
Fig. 2. (a) After incision of the superficial cervical fascia, the left sternohyoid muscle (white dashed line) is gently pulled laterally, allowing incision and removal of area A (blue dashed line). (b) Area A (blue dashed line) is pulled contralaterally, allowing dissection along the medial border of the right sternohyoid muscle (white dashed line).
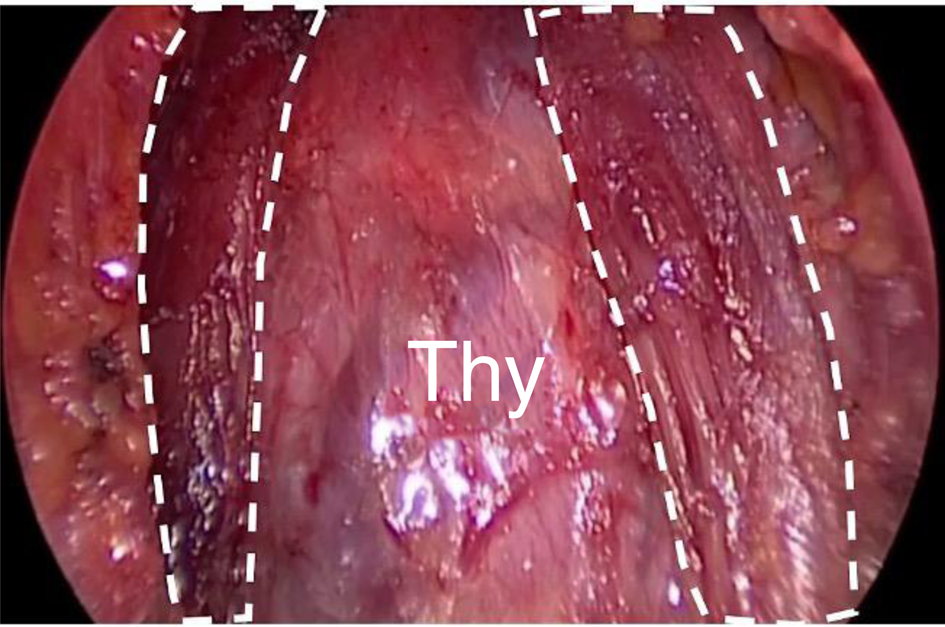
Fig. 3. Dissection of area A proceeds until the thyroid is fully exposed (Thy), with the strap muscles used as lateral landmarks (white dashed line).
Step three
The sternohyoid muscle is retracted laterally to expose the medial border of the sternothyroid muscle. The thyroid lobe is freed by laterally retracting the sternothyroid muscle and ligating all the median veins coming from the thyroid itself, until the common carotid artery is exposed (Figure 4).
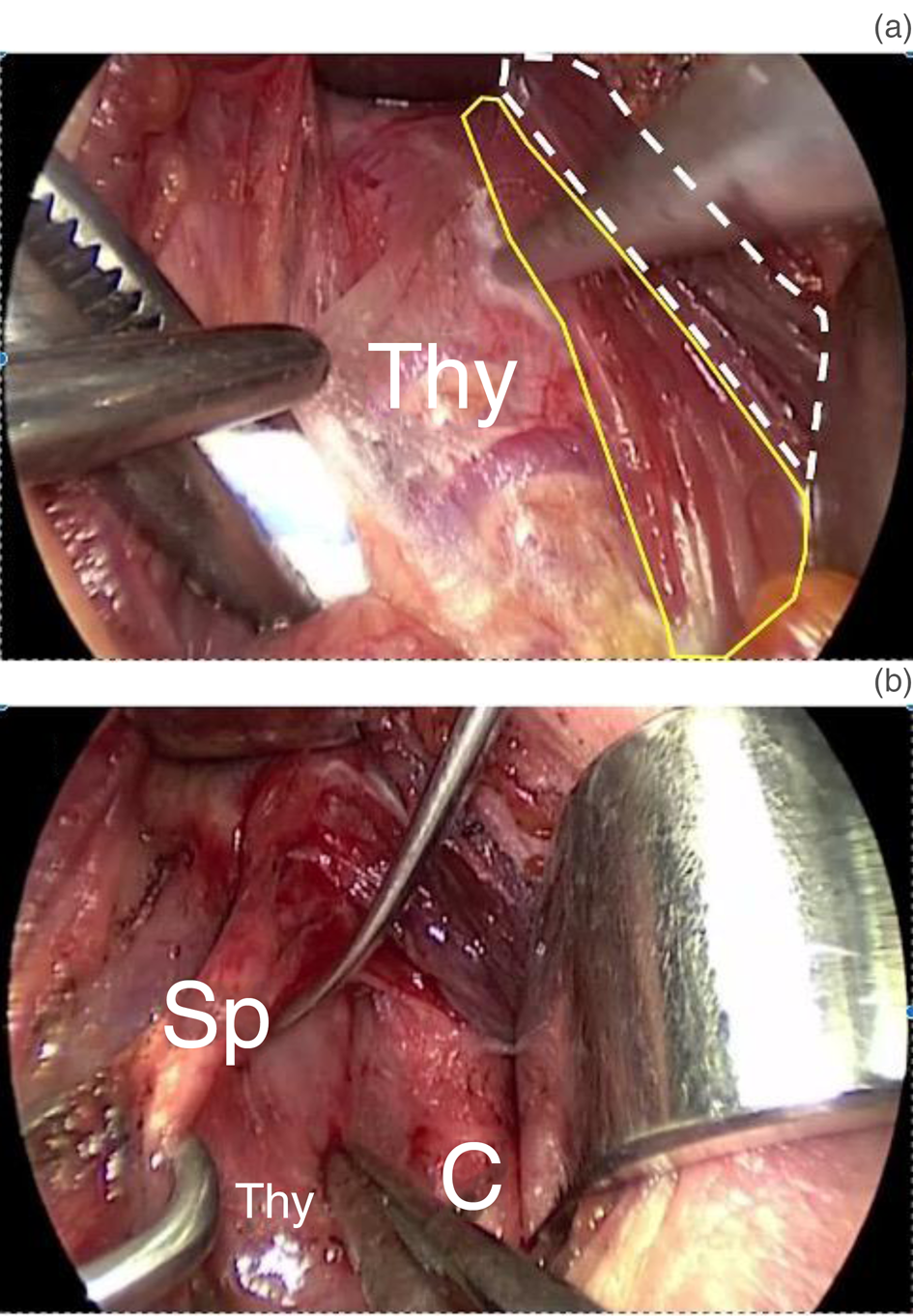
Fig. 4. (a) Thyroid gland (Thy) is freed by retracting the sternohyoid muscle (white dashed line), thus exposing the medial border of the sternothyroid muscle (yellow line). (b) All veins emerging from the thyroid (Thy) are carefully ligated and cut, and the sternothyroid muscle is retracted laterally, permitting identification of the common carotid artery (C); the superior thyroid pedicle (Sp) is exposed by gently pulling the thyroid lobe downward.
The superior thyroid pedicle is identified and ligated, vessel by vessel. The purpose is to: preserve the superior laryngeal nerve; exclude the presence of a non-recurrent laryngeal nerve (on the right side); and identify and preserve the superior parathyroid gland, together with its pedicle coming from the terminal branches of the inferior thyroid artery (Figure 5).

Fig. 5. (a) Ligation of the superior thyroid pedicle. The surgeon should pay attention to the ligate and cut vessel by vessel, thus avoiding damage to the superior laryngeal nerve and the superior parathyroid gland. (b) Identification of the superior parathyroid gland (P) with its pedicle after tying the superior thyroid pedicle.
Step four
After the thyroid lobe is gently rotated medially, the deep lymph nodes contained in the adipose tissue on the right (B) and left side (D) of the trachea (where the recurrent nerve emerges from the deep layers and runs medially toward the cricoid cartilage until its entrance into the cricothyroid membrane) are exposed. These are delimited laterally by the carotid artery, medially by the trachea, posteriorly by the oesophagus, anteriorly by the border of the thyroid lobe, cranially by the entrance point of the recurrent laryngeal nerve into the larynx, and inferiorly by the brachiocephalic (innominate) trunk (Figure 6).
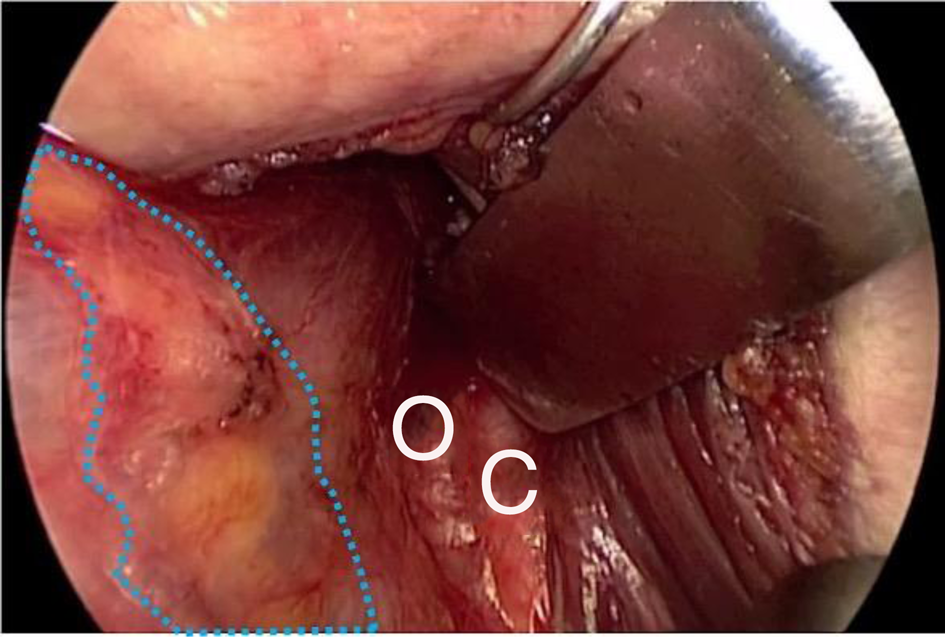
Fig. 6. The left thyroid lobe is rotated medially so that area D is finally exposed (blue dashed line), with the carotid artery (C) laterally, the trachea medially and the oesophagus (O) posteriorly.
Step five
There are several methods to help the surgeon find the recurrent nerve. In our experience, the inferior thyroid artery allows for the identification of the recurrent laryngeal nerve with its medial and lateral branches, always bearing in mind that the nerve may follow a different path, running above, below, or even in between the arterial branches.
Once identified, the inferior artery is gently pulled laterally to expose the recurrent nerve with its branches (Figure 7). The surgeon should always keep in mind that, on the left side, the recurrent nerve usually shows a more vertical run compared with the right side, being longer because it loops under the aortic arch at the ligamentum arteriosum. Both nerves follow the inferior thyroid artery, running anterior to, posterior to, or in between the terminal branches of the inferior thyroid artery.
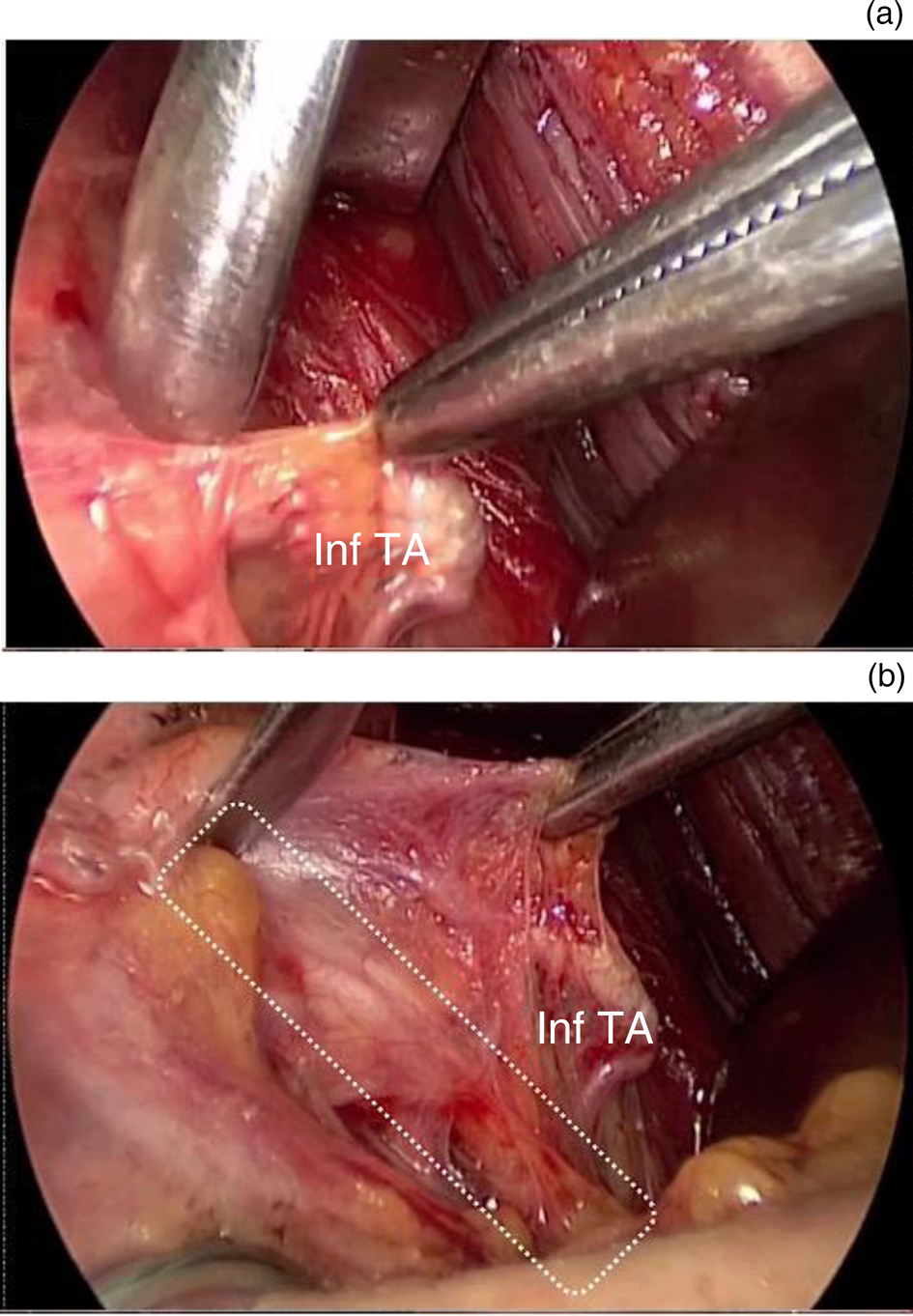
Fig. 7. (a) Identification of the inferior thyroid artery (inf TA). (b) The inferior thyroid artery (inf TA) is pulled laterally, but not ligated or cut until the surgeon exposes the recurrent nerve with its branches (white dashed line), thus verifying the highly variable course of the nerve itself.
The dissection proceeds parallel to the nerve from the brachiocephalic trunk inferiorly to its entrance into the cricothyroid cartilage superiorly. Finally, B/D (the deep lymph nodes in the adipose tissue on the right and left side of the trachea, respectively) are detached from the thyroid lobe (Figure 8).

Fig. 8. (a & b) Dissection of area D (blue dashed line) proceeds along the recurrent nerve (the white dashed lines indicate the recurrent nerve with its branches), as it becomes progressively superficial right before it enters (Ent) into the larynx at the cricothyroid membrane. T = trachea; C = common carotid artery; Inf TA = inferior thyroid artery
Step six
The loose fat tissue anterior to the trachea is gently retracted upward, with attention paid to isolate and ligate all of the inferior thyroid veins and the ima artery coming from the innominate trunk. The dissection proceeds laterally until the contralateral sternothyroid muscles and tracheal border are reached and finally detached from the thymus (Figures 9 and 10).
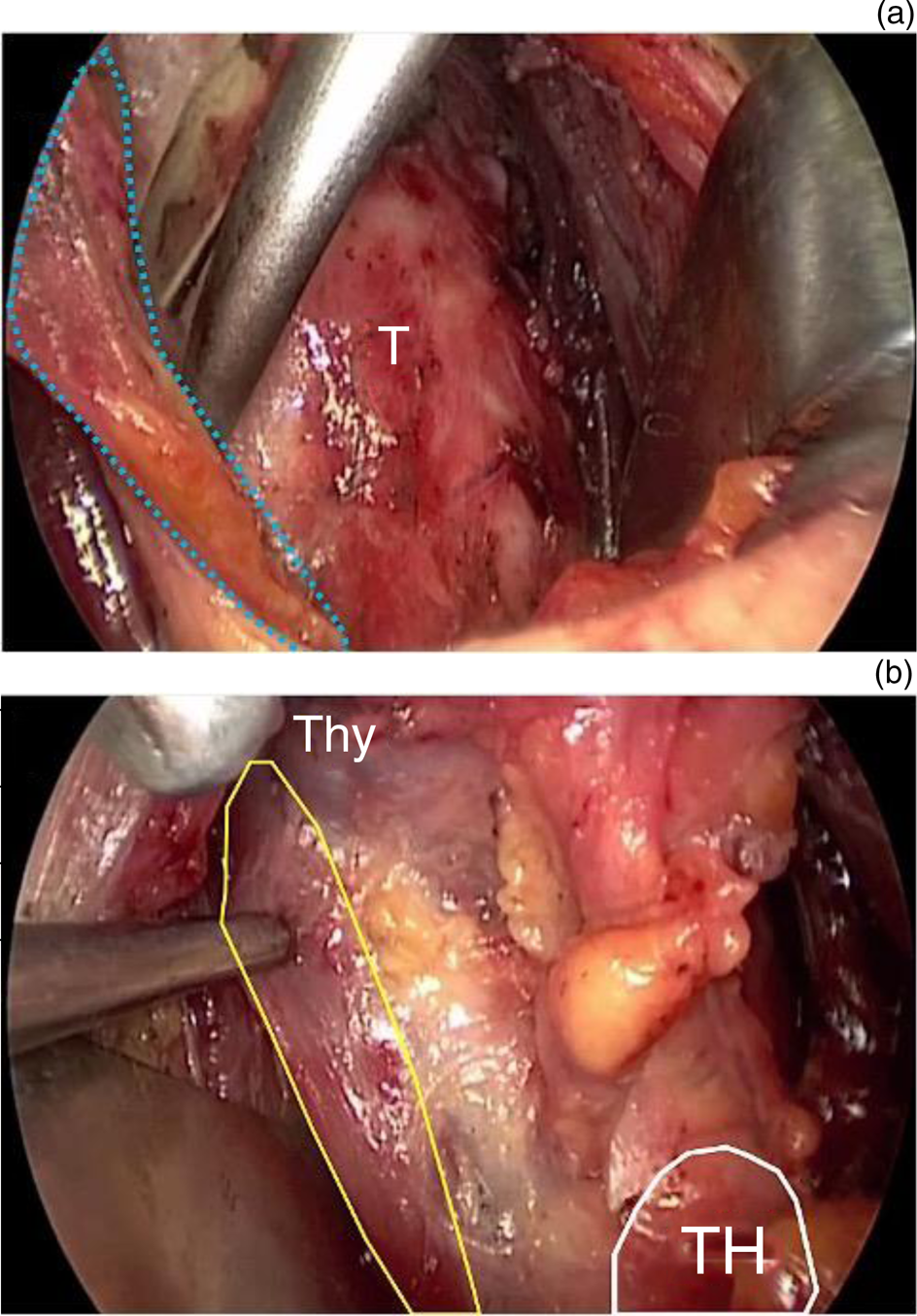
Fig. 9. (a) Dissection of area C (blue dashed line). The loose fat tissue is detached from the trachea (T), paying attention to the inferior thyroid veins and ima artery. (b) The loose fat tissue is detached from the medial border of the contralateral sternothyroid muscle (yellow line), from the thyroid isthmus superiorly (Thy) and from the thymus horn inferiorly (TH).

Fig. 10. The thyroid gland together with the recurrent lymph nodes in the four areas.
Discussion
Lymph node metastasis occurs in up to 80 per cent of patients affected by thyroid cancer, with the central neck compartment (level VI–VII) being involved in 40–60 per cent of cases.Reference Robinson, Thomas, Dinan, Roman, Sosa and Hyslop6–Reference Patel, Yip, Lubitz, Grubbs, Miller and Shen8
Nodal dissection of the central neck compartment can be performed both therapeutically (i.e. for clinically or radiographically evident lymph node metastasis) or prophylactically, based on the risk of subclinical nodal metastasis.Reference Cabanillas, McFadden and Durante1,Reference Patel, Yip, Lubitz, Grubbs, Miller and Shen8
Nevertheless, the scientific community has voiced concern about the role of routine prophylactic central lymph node dissection, as it might result in severe hypoparathyroidism and/or recurrent laryngeal nerve injuries. Recently, the UK National Multidisciplinary Guidelines indicated that prophylactic central neck dissection is associated with a high incidence of long-term, permanent hypoparathyroidism and recurrent laryngeal nerve damage, and therefore it should not be recommended in patients with low-risk and small papillary carcinomas.Reference Mitchell, Gandhi, Scott-Coombes and Perros9
The international guidelines continue to be updated, and several papers are published annually in major scientific journals on the extreme effort to delineate the best risk–benefit ratio of such a delicate procedure. Thus, it must still be emphasised that the experience of the surgeon and a thorough knowledge of the central neck compartment anatomy are essential to achieve complete removal of all metastatic lymph nodes. Adequate central neck compartment dissection should always be conducted as a systematic and standardised procedure, based on the careful identification of the inferior thyroid artery, parathyroid gland and recurrent nerves.
Anatomical knowledge and standardisation are the milestones of any surgical procedure. This holds true for all surgeons, but particularly for new surgeons, such as residents, who cannot rely simply on experience. In this regard, step-by-step descriptions of clinical techniques are priceless, especially nowadays, as high-quality pictures and videos can complement plain text.
The central neck compartment is a very delicate region that contains several vulnerable structures; damage to these structures would affect patients’ lives, possibly permanently. Although the technique used to dissect this area was codified years back,Reference Orloff and Kuppersmith5 to the best of our knowledge, an illustrated step-by-step depiction is currently lacking. This might be because of its controversial indications and, therefore, its limited use by thyroid surgeons, as discussed previously. Nonetheless, when required, it must be performed cautiously.
Dissection of area A (the Delphian and prethyroidal lymph nodes contained in the neck region, superficial to the thyroid capsule and cartilage) is straightforward, yet neglected in most thyroid surgical procedures. It requires the simple removal of fibrous tissue in front of the thyroid isthmus, which encompasses the Delphian node.
Dissection of area C (deep pretracheal nodes present in the adipose tissues, bound superficially by the strap muscles, deeply by the pretracheal fascia, cranially by the thyroid isthmus and caudally by the thymus horn) may be tricky. The upper pole of the thymus can go undetected, so that the dissection can be extended too inferiorly, endangering the mediastinal vessels. Unless frankly pathological nodes are identified, dissection of this area should not proceed further than the jugular notch. Of note, the thymus appears white-yellow when compared with the bright yellow of pretracheal fat.Reference Roman, Randolph and Kamani10
Dissection of areas B and D (the deep lymph nodes contained in the adipose tissue on the right and left side of the trachea, respectively), which is the true recurrent region, is definitely the most technically demanding. As pointed out earlier, this space is enclosed by the trachea medially, the common carotid artery laterally and the brachiocephalic trunk inferiorly. Because of the high variability of the anatomical relationship between the inferior thyroid artery and the recurrent nerve, we strongly recommend against ligating and sectioning the inferior thyroid artery before clearly identifying the nerve, thus avoiding trauma to the latter. This is especially true on the right side, where the possibility of a non-recurrent nerve must always be considered. Once identified based on its pulse and termination in the thyroid gland, the artery may be pinched delicately and pulled sideways to detect and finally expose the nerve.
Because it is likely that the inferior parathyroid gland is removed together with the loose areolar tissue of the recurrent region, we recommend that the superior gland be searched and preserved, including its nourishing vessels, especially in the case of total thyroidectomy plus removal of the whole central neck compartment.
We suggest that when emptying the recurrent area, clips or threads be used to secure vessels at the inferior limit of the dissection, instead of simple cauterisation. This is to avoid any possible bleeding of these vessels originating from or draining into arteries and veins at the cervicothoracic junction. Such bleeding would be extremely difficult to control and would transform a relatively easy procedure into a nightmare.
Of course, attention should also be paid to the lymphatic vessels, especially on the left side (area D), where the thoracic duct courses. Because these structures are very fragile, excessive traction of the surrounding tissue is best avoided. If identified, the thoracic duct should be handled carefully, touched as little as possible, and clipped.
Conclusion
Despite being a well-codified procedure, the central neck dissection procedure has not been detailed to date. This stepwise description of the surgical technique, along with high-quality pictures and specific tips and tricks, is meant to fill the gap in knowledge and to provide learning material for new surgeons.
Acknowledgement
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and ‘5 × 1000′ funds.
Competing interests
None declared












