Borderline personality disorder (BPD) is a debilitating mental illness with a lifetime prevalence of 2 to 6% in the general population (Grant et al., Reference Grant, Chou, Goldstein, Huang, Stinson, Saha, Smith, Dawson, Pulay and Pickering2008; Tomko et al., Reference Tomko, Trull, Wood and Sher2014) and about 15 to 27% in clinical populations (Korzekwa et al., Reference Korzekwa, Dell, Links, Thabane and Webb2008). BPD is characterized by emotional intensity and instability, identity disturbance, impulsive and self-destructive behaviors, and chaotic interpersonal relationships (American Psychiatric Association, 2013). BPD is a major public health concern as it is associated with high distress, functional impairments, and utilization of mental health resources both cross-sectionally (Bender et al., Reference Bender, Dolan, Skodol, Sanislow, Dyck, McGlashan, Shea, Zanarini, Oldham and Gunderson2001) and longitudinally (Zanarini et al., Reference Zanarini, Frankenburg, Hennen and Silk2004; Bagge et al., Reference Bagge, Stepp and Trull2005; Winograd et al., Reference Winograd, Cohen and Chen2008). As such, there is a clear need to understand the factors contributing to the etiology and maintenance of this disorder (Brune, Reference Brune2016).
The influences of parental psychopathology, parent–child interactions, and family environment have been prominent in both theoretical frameworks of BPD (Kernberg, Reference Kernberg and Magnavita2004; Fonagy and Luyten, Reference Fonagy and Luyten2009) and in empirical research (Paris, Reference Paris2000; Zanarini, Reference Zanarini2000; Gratz et al., Reference Gratz, Latzman, Tull, Reynolds and Lejuez2011; Belsky et al., Reference Belsky, Caspi, Arseneault, Bleidorn, Fonagy, Goodman, Houts and Moffitt2012). Several family studies document the aggregation of depression, antisocial personality disorder, and substance-use disorders – as well as BPD proper – in family members of BPD probands (Soloff and Millward, Reference Soloff and Millward1983; Zanarini et al., Reference Zanarini, Frankenburg, Dubo, Sickel, Trikha, Levin and Reynolds1998; White et al., Reference White, Gunderson, Zanarini and Hudson2003; Zanarini et al., Reference Zanarini, Barison, Frankenburg, Reich and Hudson2009). One of the most influential theories to date, Linehan's biopsychosocial theory of BPD, makes a strong emphasis on the role of family environment and environmental adversity in the development of BPD (Linehan, Reference Linehan1987, Reference Linehan1993). Several retrospective and prospective studies document the role of family factors such as parenting styles, divorce, and marital discord (Frank and Paris, Reference Frank and Paris1981; Zweig and Paris, Reference Zweig and Paris1991; Bandelow et al., Reference Bandelow, Krause, Wedekind, Broocks, Hajak and Rüther2005; Winsper et al., Reference Winsper, Zanarini and Wolke2012). For instance, individuals with BPD recall lower parental bonding as well as higher parental control (Zweig and Paris, Reference Zweig and Paris1991). Parent-reported childhood neglect predicted increased BPD severity 10 years later during adolescence and early adulthood (Johnson et al., Reference Johnson, Smailes, Cohen, Brown and Bernstein2000). Furthermore, parents with BPD seem to engage in negative parenting strategies that in turn are associated with an increased likelihood of BPD in their offspring (Newman et al., Reference Newman, Stevenson, Bergman and Boyce2007; Stepp et al., Reference Stepp, Whalen, Pilkonis, Hipwell and Levine2012; Zalewski et al., Reference Zalewski, Stepp, Scott, Whalen, Beeney and Hipwell2014).
Interpretation of these studies, however, is far from straightforward. A series of recent studies document moderate (≈ 40%) genetic contributions to BPD traits and symptoms (Distel et al., Reference Distel, Trull, Derom, Thiery, Grimmer, Martin, Willemsen and Boomsma2008; Reichborn-Kjennerud et al., Reference Reichborn-Kjennerud, Ystrom, Neale, Aggen, Mazzeo, Knudsen, Tambs, Czajkowski and Kendler2013; Amad et al., Reference Amad, Ramoz, Thomas, Jardri and Gorwood2014; Reichborn-Kjennerud et al., Reference Reichborn-Kjennerud, Czajkowski, Ystrom, Orstavik, Aggen, Tambs, Torgersen, Neale, Roysamb, Krueger, Knudsen and Kendler2015). ‘Environmental’ factors such as marital relationship (Spotts et al., Reference Spotts, Neiderhiser, Towers, Hansson, Lichtenstein, Cederblad, Pederson and Reiss2004), divorce (Jocklin et al., Reference Jocklin, McGue and Lykken1996), and parenting styles (Kendler et al., Reference Kendler, Myers and Reichborn-Kjennerud2011) are also heritable (see Kendler and Baker, Reference Kendler and Baker2007 for a review). It is possible that patterns of influence in BPD generally attributed to the familial environment are, in fact, at least partly genetically mediated. Putative environmental factors may be indirectly related to offspring BPD traits through the mechanism of passive gene–environment correlation (r GE; Plomin et al., Reference Plomin, DeFries and Loehlin1977, Scarr and McCartney, Reference Scarr and McCartney1983). Passive r GE occurs when parents create an environment that correlates with their genotype, while also passing down their genotype to their offspring. Therefore, the association between environmental factors and child outcomes is spurious and could be a function of shared genetics. In the current context, heritable factors may increase the likelihood of parental psychopathology, marital conflict and maladaptive parenting among the parents, and BPD features in the offspring.
Unfortunately, data solely from families reared together cannot help to accurately partition genetic and environmental influences in the presence of gene–environment correlation or direct effects, as in this context, parents provide both the genetic risk and the social environment for their offspring. Classical twin studies also cannot account for the effects of passive r GE and can incorrectly model them as shared environmental effects (Carpenter et al., Reference Carpenter, Tomko, Trull and Boomsma2013). An effective method of disentangling direct environmental from passive r GE effects is comparing the patterns of association in biological and adopted children. Because adoptive children do not inherit their genotype and environment from the same source, the effect of passive r GE is eliminated. If familial risk factors are associated with BPD traits in biological and adopted offspring equally, it would imply a direct environmental influence. On the contrary, if the risk factors are only related to BPD traits in biological children, it would imply genetic transmission. To our knowledge, the effect of putative environmental risk factors and parental psychopathology on the development of offspring BPD features has not been examined through an adoptive design.
The current study aimed to examine the vertical transmission of parent psychopathology, parenting practices, and family discord on offspring BPD traits, while accounting for the relative contribution of passive r GE. Using a large sample of biological and adoptive families recruited from the community, we aimed to estimate the relative contribution of genetic and direct environmental effects. Among the familial risk factors, we included parent psychopathology, parenting practices, and marital discord. Maternal and paternal psychopathology included BPD traits, adult antisocial behavior, history of conduct disorder, nicotine, alcohol and illicit substance dependence, and major depressive disorder. Notably, although parental psychopathology is not strictly a measure of ‘environment’, the adoptive design still allowed us to broadly examine genetic and environmental effects. In addition to maladaptive parental practices, we examined the effects of marital discord on offspring BPD traits.
Hypotheses
Rather than having a single directional hypothesis, we had the following competing expectations for each familial risk factor. If only environmental transmission is present, then parental risk factors should predict offspring BPD traits equally in adoptive and biological offspring. If only genetic transmission is present, one would expect an effect in biological offspring, a zero or negligible effect in adoptive offspring (as well as a significant interaction between parental risk factors and offspring adoptive status if both family types are modeled together). Finally, if both environmental and genetic transmissions are operating, then there should be effects in both biological and adoptive offspring, with the effect being larger in biological offspring (i.e. a significant interaction between parental risk factors and adoptive status).
Method
Sample
The current analyses used data from two large studies. The Siblings Interaction and Behavior Study (SIBS) (McGue, Keyes et al., Reference McGue, Keyes, Sharma, Elkins, Legrand, Johnson and Iacono2007) at the University of Minnesota consisted of 409 adoptive and 208 biological families [M age offspring = 14.93 (s.d. = 1.93); 55% female; 56% Caucasian, 39% Asian, and 5% other], recruited between 1998 and 2005. Families were eligible if they had two offspring between the ages of 11 to 21 who did not have a physical or mental impairment that could hinder the assessment. Adoptive families were ascertained from infant placements made by the three largest, private adoption agencies in Minnesota. Non-adoptive families were ascertained through Minnesota state birth records and selected to have a pair of siblings of comparable age and gender to the adoptive sibling pairs. For both adoptive and non-adoptive families, the siblings had to be no more than 5 years apart in age. For adoptive families, the adopted offspring had to have been placed prior to age 2 years. Mean age of permanent placement in the sample was 4 months. Families who had one adopted and one biological child were also eligible. Of the adoptive families, there were 124 ‘mixed’ family structures, with one adopted child, and one child biologically related to at least one parent. Participation rate was high for adoptive (63.2%) and non-adoptive (57.3%) families. Previous work (McGue et al., Reference McGue, Keyes, Sharma, Elkins, Legrand, Johnson and Iacono2007) documented few differences between participating and recruited but non-participating families, or between the study families and the general community.
The Minnesota Twin Family Study (MTFS) consisted of 580 families consisting of parents and twin pairs [M age offspring = 14.90 (s.d. = 0.60); 93.1% Caucasian]. Only female twins were included, because personality data was not available for male twins at age 14. MTFS is an ongoing population-based, longitudinal study of twins and their families (Iacono et al., Reference Iacono, Carlson, Taylor, Elkins and McGue1999; Keyes et al., Reference Keyes, Malone, Elkins, Legrand, McGue and Iacono2009). Birth records and public databases were used to locate more than 90% of families that included a twin birth in the state of Minnesota from 1975 to 1984 and from 1988 to 1994. Eligible twins and their families (a) were living within a 1-day drive of Minneapolis with at least one biological parent, and (b) had no mental or physical handicap precluding participation. Parental psychopathology was assessed at intake (when twins were aged ≈11) and again 6 years later, allowing us to obtain a lifetime index of parental psychopathology. BPD traits were first assessed at age 14 among female twins; parenting and marital satisfaction were measured concurrently. We used the age-14 assessment for the current analyses and included all families where at least one offspring had BPD trait data. Previous work (Johnson et al., Reference Johnson, Krueger, Bouchard and McGue2002) reported few differences in personality between twins and singletons in the community.
Measures
Psychopathology
The Structured Clinical Interview for DSM-III-R (Spitzer et al., Reference Spitzer, Williams and Gibbon1987), updated to include the DSM-IV criteria, was administered to both parents to assess symptoms of adult antisocial behavior, history of conduct disorder, and major depressive disorder. Higher scores reflect a higher number of symptoms endorsed. Parental symptom counts of nicotine, alcohol and illicit substance dependence (cannabis; opiates; amphetamine; sedatives; hallucinogens; cocaine; phencyclidine; inhalants) were measured using the substance use supplement of the Composite International Diagnostic Interview (Robins et al., Reference Robins, Baber and Cottler1987). The inter-rater reliability for all diagnostic procedures was higher than κ = 0.89 (Iacono et al., Reference Iacono, Carlson, Taylor, Elkins and McGue1999; McGue et al., Reference McGue, Keyes, Sharma, Elkins, Legrand, Johnson and Iacono2007). For parents and offspring aged 16 and older, BPD traits were assessed using the Minnesota Borderline Personality Scale (Bornovalova et al., Reference Bornovalova, Hicks, Patrick, Iacono and McGue2011), a 19-item, Likert-type, four-point self-report instrument derived from the Multidimensional Personality Questionnaire (Tellegen, Reference Tellegen1982, Reference Tellegen2003). For offspring younger than 16, BPD traits were assessed using the Personality Booklet Youth-Abbreviated (PBYA, developed specifically for the MTFS; e.g. Matteson et al., Reference Matteson, McGue and Iacono2013). The PBYA contains 17 of the 19 items on the MBPD. To make the MBPD and PBYA compatible, the PBYA score was prorated to a score compatible with MBPD (range 19–76) by using the proportion of maximum possible scaling method (POMP; Cohen et al., Reference Cohen, Cohen, Aiken and West1999). Higher scores are indicative of higher borderline personality pathology. The MBPD has excellent psychometric properties and has been validated on both adult and mid- to older adolescent samples (Rojas et al., Reference Rojas, Cummings, Bornovalova, Hopwood, Racine, Keel, Sisk, Neale, Boker and Burt2014; Rojas et al., Reference Rojas, Hicks, Stark, Hopwood and Bornovalova2015)Footnote †Footnote 1. In the current sample, the MBPD the PBYA showed good internal consistency (MBPD, α = 0.82; PBYA, α = 0.84). Notably, the correlations between the mother's and father's psychopathology were low (all rs < 0.30 between parents), and as such, parental psychopathology variables were kept separate in all analyses.
Family environment
The Parental Environment Questionnaire (Elkins et al., Reference Elkins, McGue and Iacono1997) is a 50-item self-report instrument that measures parent–child interactions. Each parent responded to the PEQ for each offspring, using a four-point scale to yield subscales of conflict, lack of involvement, and lack of regard (αs ranged from 0.78 to 0.87). Additionally, each parent's opinions on favoring punishment were also assessed using nine items on a child rearing questionnaire (αs ranged from 0.75 to 0.81). Higher scores on the PEQ and attitudes towards punishment reflected higher maladaptive parenting. As above, the correlations between the parents' styles were low (all rs ⩽ 0.30), except for conflict and punishment, which were higher (both rs = 0.43).
Marital discord was measured using a 34-item modified version of the Dyadic Adjustment Scale (Spanier, Reference Spanier1976), with two additional items concerning parents' attitudes towards child rearing. The DAS taps into marital satisfaction, and cohesion and marital consensus, and higher scores reflect high marital discord (α = 0.93). Each parent rated the relationship separately and their scores were averaged together to form a single estimate for each couple (rs > 0.60 between parent reports), where higher scores reflected higher discord. Finally, mothers also reported separation/divorce status. In our sample, 87.8% of the mothers were currently married and 12.2% were divorced/separated from the biological father; the remaining either never married or widowedFootnote 2.
Data analyses
As shown in Table 1, there were significant differences between biological and adoptive parents. Adoptive parents were older, were more likely to finish college and/or post-graduate school, had higher income, and were more likely to be Caucasian than biological parents. Subsequently, we adjusted for parental age, family socioeconomic status, and parental race in all analyses, and all psychological measures were standardized. We also adjusted for offspring age, sex, and ethnicity, as sex and ethnicity showed substantial differences across adoptive v. biological groups, and previous work indicates sex as well as age and ethnicity effects on BPD traits (Shea et al., Reference Shea, Edelen, Pinto, Yen, Gunderson, Skodol, Markowitz, Sanislow, Grilo and Ansell2009; Silberschmidt et al., Reference Silberschmidt, Lee, Zanarini and Schulz2015).
Table 1. Demographic characteristics in adoptive and biological families

For categorical differences, both d (Cohen's d) and diff. % (difference in percentage) were calculated. Negative d or diff. % values indicate higher means for adoptive offspring. Among parents, data were available on at least one parental variable for 2356 moms and 2129 dads.
Given dependence among data for siblings from the same family, we conducted our analyses using multilevel models with the lme4 (version 1.1-21; Bates et al., Reference Bates, Mächler, Bolker and Walker2015), optimx (version 2018-7.10; Nash and Varadhan, Reference Nash and Varadhan2011), and simr (version 1.0.5; Green and MacLeod, Reference Green and MacLeod2016) packages in R (version 3.5.2; R Core Team, 2018). All analyses were estimated as two-level random-intercept models with intercepts allowed to vary across families and residual variances allowed to differ across adoptive, biological sibling/DZ, and MZ groups. Each parental risk factor was examined separately. Across models, offspring-level covariates and predictors [age, sex, ethnicity, adoptive status, parenting practices (conflict, lack of regard, lack of involvement)] were included at level-1. Parent- and family-level covariates and predictors [parent age and ethnicity, socioeconomic status, parent psychopathology, parenting practices (attitude toward punishment), marital discord, divorce] were included at level-2.
We fit a series of two-level random-intercept models to test three key questions: (1) Is there a practically significant effect of familial variables on offspring BPD traits within adoptive families? (2) Is there a practically significant effect within biological families? and (3) Is the effect within biological families practically significantly greater than the effect within adoptive families? Evidence for environmental transmission is implied by the presence of both (1) and (2), whereas evidence for genetic transmission is implied by (2) and (3). Note that a combination of genetic and environmental transmission is inferred when (1), (2), and (3) are all present. Questions (1) and (2) were examined by estimating models separately in the adoptive and biological offspring samples. Each model included the covariates (parent age and ethnicity, family socioeconomic status, offspring gender, age, and ethnicity) and a familial risk factor (parental psychopathology or family environment) as predictors, with offspring BPD traits as the outcome. Question (3) was tested using the combined full sample with moderated regression analyses as a formal test of slope differences across biological and adoptive samples. Each model included the above covariates and a familial risk factor as predictors. Question 3 also included adoptive status and the interaction between adoptive status and the familial risk factor. A significant (i.e. one with a non-negligible effect size where the confidence interval does not include zero) moderation effect by adoptive status indicates the potential impact of the familial risk factor for BPD traits differs across biological and adoptive offspring, thereby supporting an interpretation of genetic transmission. Notably, instead of solely focusing on statistical significance, we interpret the broad pattern of effects and the magnitudes of effect sizes. To this end, all effect sizes were standardized and can be interpreted using empirical effect size benchmarks identified by Gignac and Szodorai (Reference Gignac and Szodorai2016) (Cohen's d: 0.2, 0.5, 0.8; Pearson's r: 0.1, 0.2, 0.3 for small, medium, and large, respectively corresponding to the quartiles for effect sizes observed in empirical individual differences research). Standardized regression coefficients (β) were interpreted in the r metric.
Results
Differences between families in parent and offspring psychopathology are displayed in Table 2. Adoptive offspring reported slightly higher BPD traits. Biological and adoptive families showed small but significant differences on most other factors, including higher levels of maternal and paternal externalizing psychopathology and BPD traits. Adoptive parents reported a significantly higher parent–child conflict, but were less likely to favor punishment. Biological and adoptive families did not differ on the level of marital discord, but the former were more likely to be divorced.
Table 2. Summary statistics of parent and offspring psychopathology
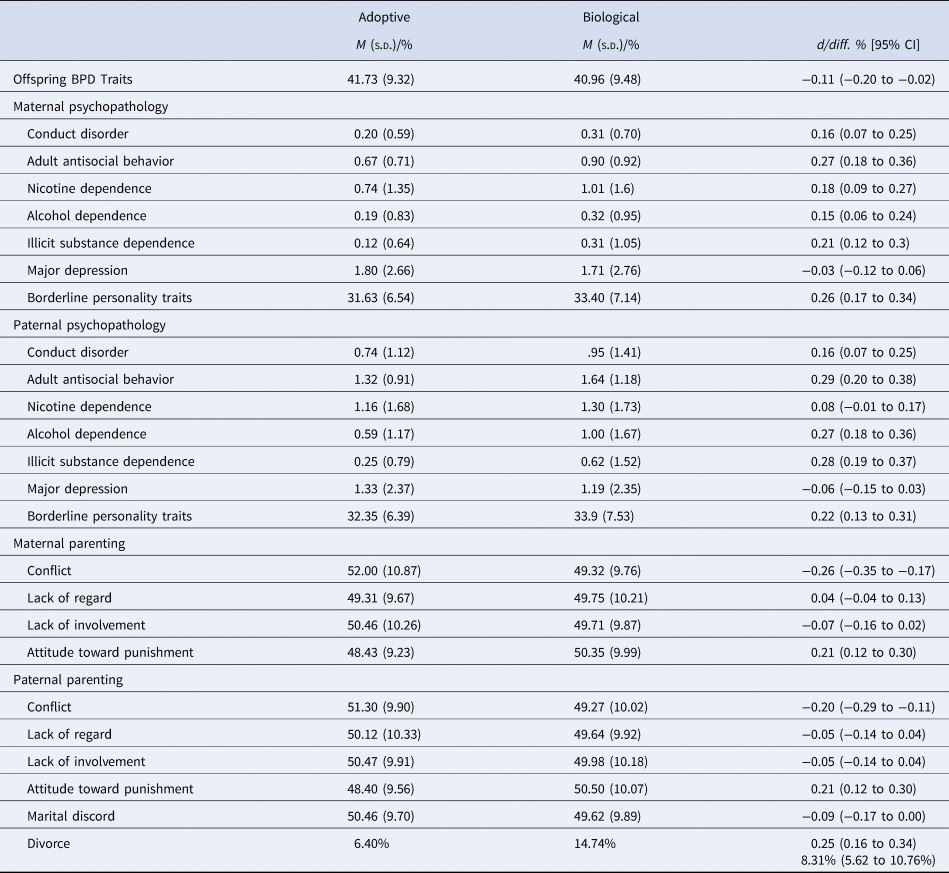
For categorical differences, both d (Cohen's d) and diff. % (difference in percentage) were calculated. Negative d or diff. % values indicate higher means for adoptive offspring. Symptom counts were used to index parental psychopathology, and the MBPD score (range 19–76) was used to index parental BPD traits. Parenting variables and marital discord were converted to T scores.
Table 3 summarizes the association between familial risk factors and offspring BPD traits in adoptive and biological offspring separately, as well as for interaction effects that test for slope differences across family typesFootnote 3. Evidence of a genetic effect required a practically significant relationship (β ⩾ .10) between offspring BPD traits and the familial risk factor for biological families and a practically significant interaction effect. This pattern was observed for both parents' psychopathology for conduct disorder, adult antisocial behavior, and nicotine, alcohol, and illicit substance dependence, with small to moderate positive effects in biological families and similar sized interaction effects (β ado ranged −0.08 to +0.03, β bio ranged 0.07 to 0.16, β int ranged 0.12 to 0.25; see Fig. 1 for visual representationsFootnote 4). The confidence interval for paternal illicit substance dependence included zero but the pattern and magnitude of effects were consistent with other externalizing psychopathology (β ado = 0.01, β bio = 0.11, β int = 0.12) and coefficients were not significantly different from coefficients for maternal illicit substance dependence. For major depression, maternal and paternal effects were weak and similar, with limited to little support evident for the transmission of either environmental or genetic risk (for maternal and paternal effects, respectively: β ado = 0.08, 0.01, β bio = 0.10, 0.07, β int = 0.03, 0.04). Paternal BPD traits displayed the genetic effect pattern (β ado = 0.04, β bio = 0.19, β int = 0.15), but maternal BPD traits showed the environmental effect pattern, with consistent small relationships with offspring BPD across family types (β ado = 0.15, β bio = 0.15, β int = −0.01).
Table 3. Familial risk factors and offspring BPD

All columns present results from separate models with psychological measures standardized. Values are standardized regression coefficients (β) with 95% confidence intervals. All models controlled for offspring age, sex and ethnicity, parent ethnicity and age, and socioeconomic status (composite of income and both parents' education). Models with full sample also controlled for adoptive status. The variables divorce and marital discord each had a single value per family. Positive interaction coefficients indicate greater effect in the biological than adoptive offspring.

Fig. 1. Effects of familial risk factors on offspring BPD by adoptive status. Axis labels represent symptom counts for parental DSM-IV psychopathology and possible range (19–76) for parental BPD traits.
Evidence of an environmental effect required a practically significant relationship (β ⩾ .10) between offspring BPD traits and the familial risk factor for both adoptive and biological families. As noted above, this pattern was observed for maternal BPD traits. It was also observed for both maternal parenting practices (conflict, lack of regard, lack of involvement; β ado ranged 0.16 to 0.28, β bio ranged 0.19 to 0.24, β int ranged −0.01 to 0.00), and paternal parenting practices (conflict, lack of regard, lack of involvement; β ado ranged 0.11 to 0.18, β bio ranged 0.09 to 0.21, β int ranged −0.03 to +0.02). Parental attitudes toward punishment and marital discord had limited support evident for either environmental or genetic transmisssion (for maternal punishment, paternal punishment, and marital discord respectively: β ado = 0.09, 0.08, −0.01; β bio = 0.07, 0.10, 0.10; β int = 0.01, 0.05, 0.10).
Evidence for both a genetic and an environmental effect required practically significant effects for both adoptive and biological families, with a larger effect in biological families (i.e. a significant interaction). No such pattern was observed.
In summary, the small to medium effects of parental externalizing disorders (maternal and paternal conduct, antisocial, and substance use disorders, paternal BPD) appeared to reflect primarily genetic effects, whereas the small to medium effects of maternal BPD and maternal and paternal parenting practices appeared to reflect primarily environmental effects.Footnote 5
Discussion
The goal of the current investigation was to determine if the vertical transmission of parent psychopathology on offspring BPD traits is explained by genetic factors, direct environmental influence of parenting and home environment, or both. To our knowledge, this is the first study to test the association between familial risk factors and offspring BPD traits via the adoptive family design. Our results suggest that the route of transmission may vary based on the specific risk factors. Genetic transmission was found for externalizing psychopathology. Each parent's conduct disorder, adult antisocial behavior, and nicotine, alcohol, and illicit substance dependence, as well as paternal BPD traits substantially predicted offspring BPD traits in biological offspring only, and the difference in slopes between adoptive and biological offspring was substantial. The nicotine finding is also notable, as this is the first study to document the association between parental nicotine use and offspring BPD features and to specify a mechanism for this relationship. Findings are congruent with previous studies showing that BPD features have a strong genetic overlap with substance use frequency and dependence, and with antisocial behavior, both cross-sectionally (Kendler et al., Reference Kendler, Aggen, Czajkowski, Røysamb, Tambs, Torgersen, Neale and Reichborn-Kjennerud2008; Hunt et al., Reference Hunt, Bornovalova and Patrick2015) and longitudinally (Bornovalova et al., Reference Bornovalova, Hicks, Iacono and McGue2013; Bornovalova et al., Reference Bornovalova, Verhulst, Webber, McGue, Iacono and Hicks2018; Rosenstrom et al., Reference Rosenstrom, Torvik, Ystrom, Czajkowski, Gillespie, Aggen, Krueger, Kendler and Reichborn-Kjennerud2018). Indeed, family studies suggest there is high familial co-aggregation with disorders marked by behavioral disinhibition (White et al., Reference White, Gunderson, Zanarini and Hudson2003). For instance, in the families of BPD probands, the risk for ASPD is 7–16% whereas the risks of alcohol and substance dependence are between 20% and 25% – rates much higher than in the general population (ASPD: 3.5%; alcohol dependence: 14%; drug dependence: 7.7%; Grant et al., Reference Grant, Chou, Goldstein, Huang, Stinson, Saha, Smith, Dawson, Pulay and Pickering2008). It is plausible that a common factor is inherited which acts as a general liability for related psychopathology. In the current context, a candidate common vulnerability factor in the transmission of parental externalizing variables to offspring BPD traits is behavioral disinhibition (Trull et al., Reference Trull, Sher, Minks-Brown, Durbin and Burr2000), which is strongly heritable (Hicks et al., Reference Hicks, Foster, Iacono and McGue2013). Thus, it is likely that the genetically transmitted disposition toward behavioral disinhibition explains the association between parent externalizing and BPD traits in biological offspring.
Support for environmental transmission was found for maternal BPD and both maternal and paternal maladaptive parenting, including conflict, lack of involvement, and lack of regard. These variables predicted BPD traits with similar magnitudes in both biological and adopted offspring. This pattern of results is consistent with previous studies (Zweig and Paris, Reference Zweig and Paris1991; Golomb et al., Reference Golomb, Ludolph, Westen, Block, Maurer and Wiss1994). Previous studies document that mothers with BPD engage in negative parenting strategies (Stepp et al., Reference Stepp, Whalen, Pilkonis, Hipwell and Levine2012), leading to subsequent poor psychosocial outcomes in offspring (Newman et al., Reference Newman, Stevenson, Bergman and Boyce2007). It is also consistent with several major etiological theories of BPD that highlight the role of familial environment (Weaver and Clum, Reference Weaver and Clum1993; Carr and Francis, Reference Carr and Francis2009) and mother–offspring conflict (Crowell, Baucom et al., Reference Crowell, Baucom, McCauley, Potapova, Fitelson, Barth, Smith and Beauchaine2013).
The current findings should be interpreted in the context of five limitations. First, although we controlled for measured differences in socioeconomic status between families, parents in adoptive families tended to be older and more educated and likely differed on other unmeasured variables as well. Second, we used a self-reported, dimensional/trait-based measure of BPD traits rather than a clinical interview-based diagnosis. While interviews are often assumed to be superior to questionnaire measures, there is limited evidence for the superiority or incremental validity of one method over the other, though each approach has unique strengths and weaknesses (Hopwood et al., Reference Hopwood, Morey, Edelen, Shea, Grilo, Sanislow, McGlasha, Daversa, Gunderson, Zanarini, Markowitz and Skodol2008). Additionally, we showed here that the MBPD has construct validity in participants as young as 11. Likewise, although the test-retest reliability of BPD in adolescents has been questioned (Biskin, Reference Biskin2015), this appears to be mainly a function of unreliability of dichotomized diagnoses. Indeed, several studies document that the test-retest reliability of BPD traits is high when measured via dimensional and/or trait-based indices (Chanen et al., Reference Chanen, Jackson, McGorry, Allot, Clarkson and Yuen2004). Yet ideally, the current study should be replicated using a multi-method approach (i.e. trait- and interview-based measures). Third, future studies should examine if the relationship between parental risk factors and offspring BPD traits varies by sex. Fourth, the data analyses were cross-sectional, and causal or directional statements require further assumptions (Rohrer, 2018). It is possible and indeed likely that offspring BPD traits evoke maternal–child conflict and lack of involvement, or that the influence is bidirectional (Stepp et al., Reference Stepp, Whalen, Scott, Zalewski, Loeber and Hipwell2014). Fifth, the current study was able to arbitrate between environmental transmission v. passive r GE. However, it was not able to detect or rule out evocative r GE or G × E. Evocative r GE occurs when offspring characteristics evoke a response from the environment (e.g. offspring BPD traits lead parents to adopt harsher punishment practices); G × E occurs when offspring have a genetic susceptibility to environmental influences. These processes are plausible in the relationship between parenting and BPD traits from both a theoretical (e.g. Linehan, Reference Linehan1993) and empirical (Belsky et al., Reference Belsky, Caspi, Arseneault, Bleidorn, Fonagy, Goodman, Houts and Moffitt2012; Reinelt et al., Reference Reinelt, Stopsack, Aldinger, Ulrich, Grabe and Barnow2014; Stepp et al., Reference Stepp, Whalen, Scott, Zalewski, Loeber and Hipwell2014) standpoint. Follow-up studies can disentangle these processes by moderating the genetic architecture of BPD traits by self- and parent-reports of parenting (Purcell, Reference Purcell2002).
Despite these potential limitations, several strengths of the study should be acknowledged. To our knowledge, this is the first paper that compared the transmission of BPD traits across biological and adoptive families and thus took the role of passive r GE into account. Additionally, we used a large sample to test the hypotheses. Formal power analyses indicated we generally had sufficient power to detect even small effect sizes. Generally, BPD research involves retrospective self-reports on family environment and parenting practices. In this study, we measured current familial risk factors from parents themselves. Hence, we eliminated the influence of offspring's acute psychopathology and retrospective bias on reports of parent practices and home environment.
Findings of the current study contribute to the understanding of the etiology of BPD, which has implications for developing effective prevention and intervention strategies. Essentially, this study highlights the partial genetic nature of BPD while at the same time elucidating the role of parenting practices that are associated with BPD traits in both biological and adoptive offspring. Therefore, interventions targeting parenting practices could help prevent the expression of BPD traits in offspring.
Financial support
Data for this project were collected at the University of Minnesota. This work was supported by National Institute on Drug Abuse Grant DA 05147, National Institute on Alcohol Abuse and Alcoholism Grants AA09367 and AA015621, and the National Institute on Mental Health MH066140-10.






