Introduction
The generally accepted definition of a biofilm is a structured community of bacterial cells enclosed in a self-produced polymer matrix that is attached to an abiotic or biotic surface (Costerton et al., Reference Costerton, Stewart and Greenberg1999; Hall-Stoodley and Stoodley, Reference Hall-Stoodley and Stoodley2009). Virtually all bacteria can grow as a biofilm and biofilms can be found in every ecosystem including natural, engineered and pathogenic settings. Growth as a biofilm is considered to be a protective mode that allows for survival in hostile environments. Additionally, bacteria grown in biofilms can form intricate and complex structures such as channels that allow nutrients to circulate. The structure of a biofilm has an impact on gene expression. Cells located in different areas of the biofilm will exhibit different patterns of gene expression (Costerton et al., Reference Costerton, Stewart and Greenberg1999). Although the biofilm is composed of sessile individuals, biofilm communities can give rise to non-sessile (or planktonic) individuals that can rapidly multiply, disperse and start a new biofilm.
The clinical significance of biofilm etiology was first established in device-related infections (Donlan and Costerton, Reference Donlan and Costerton2002; Hall-Stoodley et al., Reference Hall-Stoodley, Costerton and Stoodley2004). Electron microscopy of medical device surfaces, which had been foci of device-related infections in humans, showed the presence of large numbers of slime (matrix)-enclosed bacteria (Costerton et al., Reference Costerton, Stewart and Greenberg1999). Furthermore, biofilms have also been isolated in the absence of medical devices. For example, tissues isolated from chronic infections also showed the presence of bacteria surrounded by an exopolysaccharide (EPS) matrix (Donlan and Costerton, Reference Donlan and Costerton2002). The visual characteristics of biofilms growing in diverse environments are strikingly similar, indicating that there are important convergent survival strategies that are conferred in part by structural specialization (Hall-Stoodley et al., Reference Hall-Stoodley, Costerton and Stoodley2004). Bacterial biofilms share several common features: (i) cells are held together by an extracellular matrix composed mainly of EPS, proteins and nucleic acids; (ii) biofilm development occurs in response to extracellular signals, both environmental and self-produced; (iii) biofilms protect bacteria from a diverse and wide array of environmental stresses such as antibiotics, predators and the immune system (Lemon et al., Reference Lemon, Earl, Vlamakis, Aguilar and Kolter2008).
Interestingly, biofilm aggregates have also been observed within epithelial cells. Uropathogenic Escherichia coli (UPEC) undergo cycles of invasion of the bladder epithelium, intracellular proliferation in polysaccharide-containing biofilm-like masses called intracellular bacterial communities (IBC), and then dispersal into the bladder lumen to initiate further rounds of epithelial colonization and invasion (Anderson et al., Reference Anderson, Palermo, Schilling, Roth, Heuser and Hultgren2003).
The ability to form biofilms is now seen as a universal attribute of micro-organisms (Lemon et al., Reference Lemon, Earl, Vlamakis, Aguilar and Kolter2008). Approximately 80% of the world's microbial biomass resides as biofilm populations. The National Institutes of Health estimates that up to 75% of human infections are caused by the formation and persistence of biofilms (Richards and Melander, Reference Richards and Melander2009). Although a PubMed search (15 July 2010) gave more than 13,500 hits for ‘biofilm’, relatively few studies concerning veterinary bacterial pathogens have been perfomed. Considering the extensive involvment of biofilms in infections and diseases in human, biofilms are likely responsible for a wide variety of infections in veterinary medicine (Clutterbuck et al., Reference Clutterbuck, Woods, Knottenbelt, Clegg, Cochrane and Percival2007). Here, we review the current knowledge on bacterial biofilms, which was mostly gained from environmental, industrial and human clinical samples. This review is intended to cover biofilm formation in animal pathogens and to increase awareness about the potential impact of biofilms on the treatment options for animals and disinfection protocols used in both farming and food industries.
Model for biofilm formation
The currently accepted model for biofilm formation is based on observations obtained using various bacterial species (Costerton et al., Reference Costerton, Stewart and Greenberg1999; Hall-Stoodley et al., Reference Hall-Stoodley, Costerton and Stoodley2004; Hall-Stoodley and Stoodley, Reference Hall-Stoodley and Stoodley2009). Multiple steps are involved in the formation of biofilm by bacteria (Fig. 1A). The bacteria must first attach to a surface. Specific components found at the bacterial surface are required for adhesion. Once the bacteria have attached to a surface, they will autoaggregate into microcolonies. In addition to adhesion factors, other bacterial surface components are required for autoaggregation to occur. Following microcolony formation, the biofilm starts to take form by the maturation of the attached bacteria. During maturation, the bacterial community produces EPS, which surrounds and binds the bacterial community. Bacteria in a biofilm coordinate their behavior resulting in the formation of complex three-dimensional structures. Despite the coordinate effort in the biofilm, the bacterial biofilm community displays functional heterogeneity. The overall three-dimensional structure of the biofilm can be flat or mushroom shaped; biofilm shape is influenced by nutrient sources and the presence or absence of shear force. It is well established that bacteria can adapt to environmental changes by sensing cell density (quorum sensing (QS)) or other environmental cues. These environmental signals and conditions influence several biological functions, including biofilm formation. Some environmental signals have been identified; however, other signals are yet to be studied (Karatan and Watnick, Reference Karatan and Watnick2009). Environmental signals can be divided into three categories: mechanical (e.g. surface sensing), nutritional and metabolic (e.g. concentration of glucose, iron and phosphate) and secondary messenger and signalling networks (e.g. c-di-GMP, two-component systems). The final step in biofilm formation is detachment and dispersal of bacteria from the biofilm. The released bacteria can then colonize new surfaces.

Fig. 1. (A) Growth and development of biofilms. In the center is seen the microcolony formation observed in biofilms. The lower right demonstrates polymicrobial biofilms formed through specific cell–cell signaling and attraction. The upper right demonstrates the mechanism of biofilm spread where cells become motile, swim away as a planktonic population and following to the left go through a cycle of reversible adherence, tight adherence and microcolony formation again under regulation of specific cell–cell communication. (B) Multifactorial mechanisms that contribute to antibiotic tolerance developed within a biofilm (from Ceri et al., Reference Ceri, Olson and Turner2010; reproduced with permission). Ceri et al., Expert Opinion in Pharmacotherapy, 11/8, copyright © 2010, Informa Healthcare. Reproduced with permission of Informa Healthcare.
As with the previous steps, dispersion is greatly influenced by environmental cues (e.g. nutrients, oxygen depletion, c-di-GMP and QS) (Karatan and Watnick, Reference Karatan and Watnick2009). Detachment can be initiated by several factors including mechanical perturbations (e.g. changes in shear forces or abrasion), enzymatic degradation of the biofilm matrix (e.g. dispersin B and alginate lyase), enzymatic degradation of the biofilm substrate (e.g. hyaluronidase), induction of motility, production of surfactants (e.g. rhamnolipids), release of EPS and surface-binding proteins or cell death and cell lysis (Hall-Stoodley et al., Reference Hall-Stoodley, Costerton and Stoodley2004; Karatan and Watnick, Reference Karatan and Watnick2009; Kaplan, Reference Kaplan2010). Recently, new factors controlling biofilm dispersion have been identified. Kolodkin-Gal et al. (Reference Kolodkin-Gal, Romero, Cao, Clardy, Kolter and Losick2010) discovered that D-amino acids (D-leucine, D-methionine, D-tyrosine and D-tryptophan) prevented biofilm formation by Bacillus subtilis, Staphylococcus aureus and Pseudomonas aeruginosa. D-amino acids did not have any effect when D-alanine was present. This suggests that D-amino acids prevent biofilm formation by replacing D-alanine in the peptide side chain of peptidoglycan. D-amino acids are produced by many bacteria and, thus, D-amino acids may act as biofilm dispersal signals in several bacterial species. The detachment of bacteria from an existing biofilm plays an important role in the transmission of bacteria from environmental reservoirs to human or animal hosts, in horizontal and vertical transmission between hosts, and in the exacerbation and spread of infection within a host (Kaplan, Reference Kaplan2010).
The biofilm matrix
The biofilm matrix is believed to be highly hydrated (up to 97%) (Karatan and Watnick, Reference Karatan and Watnick2009). Several components such as polysaccharides, proteins, DNA, surfactants, lipids, glycolipids, membrane vesicles and ions (Ca2+) have been identified in the matrices of biofilm. The composition of the biofilm matrices varies according to bacterial species and growth conditions (Karatan and Watnick, Reference Karatan and Watnick2009). One of the most common and most extensively studied matrix EPS is a polymer of β-1,6-N-acetyl-D-glucosamine called poly-glucosamine (PGA), poly-N-acetyl-glucosamine (PNAG) or polysaccharide intercellular adhesin (PIA). Several bacterial species such as E. coli, S. aureus, Staphylococcus epidermidis, Yersinia pestis, Actinobacillus spp., Aggregatibacter actinomycetemcomitans and Bordetella spp. produce PGA in their biofilm matrices (Fig. 2). Another EPS that is commonly found in biofilm matrices is cellulose, a linear polymer of β-1-4-linked glucose. Cellulose is found in some strains of E. coli, Salmonella, Citrobacter, Enterobacter and Pseudomonas. Alginate, a polymer of β-1-4-linked mannuronic acid and guluronic acid, is found in P. aeruginosa.
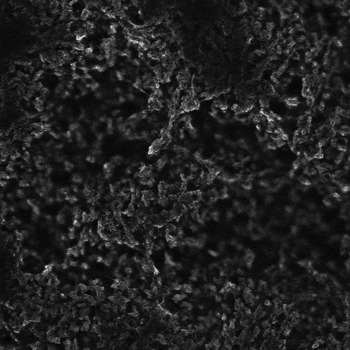
Fig. 2. Confocal scanning laser microscopic image of Actinobacillus pleuropneumoniae serotype 5b strain L20 biofilm stained with wheat germ agglutinin (WGA)-Oregon Green 488. WGA binds to PGA of the biofilm matrix.
Biofilms are resistant to various agents
Biofilms found in natural and industrial environments are resistant to bacteriophages, amoebae and biocides used in industrial processes (Costerton et al., Reference Costerton, Stewart and Greenberg1999). Furthermore, biofilms formed by medically important bacteria can withstand host immune responses and there is good evidence that bacteria in a biofilm are less susceptible to antibiotics and biocides than their planktonic counterparts (Costerton et al., Reference Costerton, Stewart and Greenberg1999; Russell, Reference Russell2002; Hall-Stoodley et al., Reference Hall-Stoodley, Costerton and Stoodley2004; Anderson and O'Toole, Reference Anderson and O'Toole2008; Hall-Stoodley and Stoodley, Reference Hall-Stoodley and Stoodley2009). In fact, infections associated with biofilms are 10 to 1000 times more resistant to the effects of antimicrobial agents (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002; Ceri et al., Reference Ceri, Olson and Turner2010).
Several mechanisms and factors are likely employed by biofilms to resist antimicrobial agents (Costerton et al., Reference Costerton, Stewart and Greenberg1999; Hall-Stoodley et al., Reference Hall-Stoodley, Costerton and Stoodley2004; Anderson and O'Toole, Reference Anderson and O'Toole2008; Ceri et al., Reference Ceri, Olson and Turner2010) (Fig. 1B). The barrier created by the biofilm matrix is considered one of the major factors that increase the resistance of bacteria to antimicrobial agents. This is particularly relevant for reactive (bleach or superoxides), charged (metals) or large (immunoglobulins) antimicrobial agents that are neutralized or bound by the matrix. Another proposed mechanism of antimicrobial resistance is related to the different metabolic states of bacteria found within the biofilm. In a biofilm, nutrients are limited and as a result, bacteria can exist in low metabolic states or in a starved/dormant state. This might result in the formation of persister cells which represent a small subpopulation of bacteria (spore-like cells) that spontaneously enter a dormant, non-dividing state. Persister cells have a greatly reduced susceptibility to antibiotics, and therefore, can also contribute to increased resistance of the biofilm to antimicrobial agents. Additionally, multispecies biofilms exhibit a decrease in antimicrobial susceptibility when compared to their single species counterparts. For example, a bacterial species can be protected against the action of an antibiotic by another species or strain that produces a β-lactamase (Hall-Stoodley and Stoodley, Reference Hall-Stoodley and Stoodley2009).
Antibiotics can degrade fairly quickly in the environment; however, antibiotic resistance genes have now been identified in water and sediment surrounding animal feedlots (Zhang et al., Reference Zhang, Sturm, Knapp and Graham2009). A recent study has demonstrated the accumulation of tetracycline (tet) resistance genes in aquatic biofilms due to periodic loadings from swine lagoons (Zhang et al., Reference Zhang, Sturm, Knapp and Graham2009). Similar trends and patterns were seen with extended-spectrum β-lactamase (bla) and macrolide (erm) resistance genes (Knapp et al., Reference Knapp, Zhang, Sturm and Graham2010). Antibiotic resistance genes can spread rapidly to biofilms and these genes will persist longer in the biofilm when compared to adjacent waters. This suggests that biofilms likely act as reservoirs for antibiotic resistance genes.
The minimal inhibitory concentration (MIC) has been used as a gold standard for the determination of antimicrobial sensitivity of planktonic populations of animal and human pathogens (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). The inherent problem with the MIC of planktonic bacteria is that it does not correlate with the concentration required to eradicate biofilms. Therefore, the misuse of antibiotics to treat biofilm-associated bacterial infections likely contributed to the development and spread of antibiotic resistance in bacteria (Ceri et al., Reference Ceri, Olson and Turner2010). It is now possible to determine the minimal antibiotic concentration to eradicate a biofilm and this is referred to as the minimal biofilm eradication concentration (MBEC) (Ceri et al., Reference Ceri, Olson, Stremick, Read, Morck and Buret1999). Determination of the MBEC might permit the selection of the appropriate antibiotic for the treatment of a specific bacterial infection (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). Optimal antibiotic treatment could decrease the spread of antibiotic resistance and reduce complications related to chronic infections. The need for updated standard guidelines for testing the susceptibility of biofilms is not limited to antibiotics and also applies to biocides (Toté et al., Reference Toté, Horemans, Vanden Berghe, Maes and Cos2010).
In vitro systems to study biofilms
Several systems are widely used to study biofilm formation (Lemon et al., Reference Lemon, Earl, Vlamakis, Aguilar and Kolter2008). Flow cells are small chambers that allow a submerged biofilm to form in the presence of shear force and with a continuous supply of fresh nutrients; this system is amenable to observation through confocal scanning laser microscopy (CSLM). One of the advantages of the flow cell system is that it mimics conditions that are naturally encountered by bacterial biofilm. Submerged biofilm can also be studied as batch cultures in microtiter plates (Fig. 3A); the main advantage of this commonly used system is its effectiveness for high-throughput screens. Until recently, the absence of shear force was one of the major limiting factors of the batch culture. Benoit et al. (Reference Benoit, Conant, Ionescu-Zanetti, Schwartz and Matin2010) developed a flow-cell system that utilizes a 96-well plate, and is compatible with CSLM and plate readers. Overall, this new method combines the advantages of the batch format (i.e. high-throughput screen) with those of the flow cell (i.e. natural biofilm). The floating pellicles that form at the liquid–air interface of standing cultures represent another form of biofilm (Fig. 3B). In addition, colonies growing on the surface of agar that demonstrate macroscopically complex architecture (e.g. Bacillus) are now recognized as a type of biofilm (Lemon et al., Reference Lemon, Earl, Vlamakis, Aguilar and Kolter2008). A method to grow biofilms under low shear conditions at the air–liquid interface was recently described (Goeres et al., Reference Goeres, Hamilton, Beck, Buckingham-Meyer, Hilyard, Loetterle, Lorenz, Walker and Stewart2009). This method is called the drip flow reactor and this reactor allows fresh culture medium to drop onto diverse surfaces such as a glass microscope slide or a catheter. This system can model environments such as the lungs and oral cavity.

Fig. 3. Biofilm assays. (A) Biofilms of Actinobacillus pleuropneumoniae isolates formed in a microtiter plate and stained with crystal violet. (B) Biofilm of A. pleuropneumoniae serotype 5b strain L20 formed in a glass tube and stained with crystal violet.
Ceri et al. (Reference Ceri, Olson, Stremick, Read, Morck and Buret1999) described a technology, originally called the Calgary Biofilm Device, for the rapid and reproducible screening of the antibiotic or biocide susceptibility of a biofilm. The device is now called the MBEC Assay System. The device consists of a two-part reactive vessel. The top component forms a lid with 96 pegs that are designed to sit in the channels at the bottom component and fit into the wells of a standard 96-well plate. The bottom of the vessel serves to channel the flow of medium across the pegs to create consistent shear force across all pegs. This results in the formation of 96 equivalent biofilms. The MBEC Assay System is used to determine the MBEC of bacterial pathogens of medical and veterinary importance.
Biofilm formation by animal pathogens
In their seminal work, Olson et al. (Reference Olson, Ceri, Morck, Buret and Read2002) used the Calgary Biofilm Device to test the biofilm-forming ability of several Gram-negative and Gram-positive pathogens of veterinary importance, isolated from cattle, sheep, pigs, chicken and turkeys. In addition, they determined the MIC and MBEC of various antibiotics. This study clearly demonstrated the diversity of organisms that can form biofilms. It also showed that biofilms formed by veterinary pathogens were resistant to commonly used antibiotics in veterinary medicine. In the next sections, we review the literature regarding biofilm formation of pathogenic bacteria of veterinary importance (Table 1).
Table 1. Studies on biofilm formation of bacterial pathogens of veterinary importance

Actinobacillus pleuropneumoniae
Actinobacillus pleuropneumoniae is an important swine pathogen and member of the Pasteurellaceae family. A. pleuropneumoniae has the ability to form biofilms under specific growth conditions, when cultured under static (Kaplan and Mulks, Reference Kaplan and Mulks2005; Labrie et al., Reference Labrie, Pelletier-Jacques, Deslandes, Ramjeet, Auger, Nash and Jacques2010) and low shear conditions at the air–liquid interface (Y.D.N. Tremblay and M. Jacques, unpublished data). In A. pleuropneumoniae, the formation of biofilm on polystyrene microtiter plates is dependent on the production of PGA (Kaplan et al., Reference Kaplan, Velliyagounder, Ragunath, Rohde, Mack, Knobloch and Ramasubbu2004; Izano et al., Reference Izano, Sadovskaya, Vinogradov, Mulks, Velliyagounder, Ragunath, Kher, Ramasubbu, Jabbouri, Perry and Kaplan2007). PGA biosynthesis is dependent on the proteins encoded within the pgaABCD operon (Kaplan et al., Reference Kaplan, Velliyagounder, Ragunath, Rohde, Mack, Knobloch and Ramasubbu2004). PGA is the substrate for dispersin B (DspB) which is a glycosyl hydrolase produced by Aggregatibacter (Actinobacillus) actinomycetemcomitans and A. pleuropneumoniae (Kaplan et al., Reference Kaplan, Velliyagounder, Ragunath, Rohde, Mack, Knobloch and Ramasubbu2004; Kerrigan et al., Reference Kerrigan, Ragunath, Kandra, Gyémant, Liptak, Janossy, Kaplan and Ramasubbu2008). Dispersin B releases biofilms formed by A. pleuropneumoniae, A. actinomycetemcomitans and other PGA-producing bacterial pathogens. In A. pleuropneumoniae, mutants lacking pgaC cannot form biofilm on polystyrene surfaces (Izano et al., Reference Izano, Sadovskaya, Vinogradov, Mulks, Velliyagounder, Ragunath, Kher, Ramasubbu, Jabbouri, Perry and Kaplan2007; Liu et al., Reference Liu, Tan, Li, Chen, Xu, He, Bei and Chen2008). Furthermore, overexpression of the pga operon was associated with enhanced biofilm formation in an rseA mutant, which is deficient in the anti-sigma factor for σE, and an H-NS mutant (Dalai et al., Reference Dalai, Zhou, Wan, Kang, Li, Li, Zhang and Chen2009; Bossé et al., Reference Bossé, Sinha, Li, O'Dwyer, Nash, Rycroft, Kroll and Langford2010). It was recently demonstrated that σE and H-NS independently regulate the expression of the pga operon (Bossé et al., Reference Bossé, Sinha, Li, O'Dwyer, Nash, Rycroft, Kroll and Langford2010). Positive regulation by σE indicates that biofilm formation in A. pleuropneumoniae is part of the extracytoplasmic stress response. The association between the extracytoplasmic stress response and biofilm formation has also been observed in other Gram-negative bacteria such as E. coli (Dorel et al., Reference Dorel, Lejeune and Rodrigue2006; Yang et al., Reference Yang, Ma and Wood2008) and Burkholderia pseudomallei (Korbsrisate et al., Reference Korbsrisate, Vanaporn, Kerdsuk, Kespichayawattana, Vattanaviboon, Kiatpapan and Lertmemongkolchai2005). Interestingly, both pgaB and pgaC were upregulated in A. pleuropneumoniae attached to St. Jude Porcine Lung (SJPL) cells (Auger et al., Reference Auger, Deslandes, Ramjeet, Contreras, Nash, Harel, Gottschalk, Olivier and Jacques2009a). This upregulation suggests that PGA produced by A. pleuropneumoniae might play a role during infection and may participate in biofilm formation in vivo.
PGA appears to play a significant role in the properties of the A. pleurepneumoniae biofilm. The presence of PGA in the matrix impedes fluid convection and transport of cetylpyridinium chloride (CPC) through A. pleuropneumoniae biofilms ( Ganeshnarayan et al., Reference Ganeshnarayan, Shah, Libera, Santostefano and Kaplan2009). CPC binds reversibly to the biofilm matrix suggesting that PGA sequesters CPC. Therefore, PGA prevents contact between CPC and the bacteria located within the biofilm. Additionally, treatment of a biofilm from field isolates (serotype 5) with dispersin B increased the sensitivity of A. pleuropneumoniae to ampicillin. This indicates that A. pleuropneumoniae cultured as a biofilm exhibits a higher resistance to antibiotics than by its planktonic counterpart (Izano et al., Reference Izano, Sadovskaya, Vinogradov, Mulks, Velliyagounder, Ragunath, Kher, Ramasubbu, Jabbouri, Perry and Kaplan2007). Our group observed that zinc could completely inhibit biofilm formation by A. pleuropneumoniae and A. actinomycetemcomitans (Labrie et al., Reference Labrie, Pelletier-Jacques, Deslandes, Ramjeet, Auger, Nash and Jacques2010). It is well established that PGA functions as a matrix polysaccharide in phylogenetically diverse bacteria. Therefore, it would be worth investigating if zinc interferes with PGA biosynthesis in other bacteria.
In addition to the pga operon, σE and H-NS, other genes have been associated with biofilm formation in A. pleuropneumoniae. Enhanced biofilm formation was observed in a QS (luxS) mutant (Li et al., Reference Li, Zhou, Li, Kang, Wan, Xu and Chen2008), whereas deficient biofilm formation was observed for a mutant (arcA) in the ArcAB two-component system facilitating metabolic adaptation to anaerobicity (Buettner et al., Reference Buettner, Maas and Gerlach2008) and an autotransporter serine protease (aasP) mutant (Tegetmeyer et al., Reference Tegetmeyer, Fricke and Baltes2009).
Aeromonas hydrophila
Aeromonads are ubiquitous water-borne bacteria that are significant pathogens of amphibians, fish and reptiles. Aeromonad infections are also associated with gastroenteritis cases in humans (Gavìn et al., Reference Gavìn, Rabaan, Merino, Tomàs, Gryllos and Shaw2002). Aeromonas hydrophila readily attaches to surfaces to produce a thin biofilm with a complex 3D structure. Lynch et al. (Reference Lynch, Swift, Kirke, Keevil, Dodd and Williams2002) were the first to demonstrate a role for N-acylhomoserine lactone (AHL)- or autoinducer-1 (AI-1)-dependent QS in the development of biofilm by A. hydrophila. Kozlova et al. (Reference Kozlova, Popov, Sha, Foltz, Erova, Agar, Horneman and Chopra2008) have shown that mutation in the luxS gene, involved in autoinducer-2 (AI-2) QS, also affects biofilm formation by A. hydrophila. Furthermore, lateral flagella are essential for adherence and biofilm formation on epithelial cells by A. hydrophila (Gavìn et al., Reference Gavìn, Rabaan, Merino, Tomàs, Gryllos and Shaw2002).
Arcanobacterium pyogenes
Arcanobacterium (Actinomyces) pyogenes is a commensal bacterium and also an opportunistic pathogen of economically important livestock such as dairy and beef cattle, and swine. A. pyogenes causes a wide array of diseases including mastitis, liver abscesses and pneumonia (Jost and Billington, Reference Jost and Billington2005). A. pyogenes can readily form biofilms (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002); this appears to be controlled by the two-component regulatory system PloSR (Jost and Billington, Reference Jost and Billington2005). This two-component regulatory system is considered a global regulator of A. pyogenes virulence. The implication of the PloSR system in biofilm formation suggests that biofilm formation may also be a virulence factor in A. pyogenes. Furthermore, when A. pyogenes was grown as a biofilm it was highly resistant to antibiotics (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002).
Bacillus cereus group
The Bacillus cereus group includes three genetically related species: B. cereus sensu stricto, Bacillus anthracis and Bacillus thuringensis (Auger et al., Reference Auger, Ramarao, Faille, Fouet, Aymerich and Gohar2009b). B. cereus biofilm formation is highly dependent on the strain, the assay and environmental conditions (Wijman et al., Reference Wijman, de Leeuw, Moezelaar, Zwietering and Abee2007). Furthermore, the ability of B. cereus to form biofilms in polyvinylchloride (PVC) microtiter plates at 30°C is strongly dependent on the origin of the strain; strains isolated from soil or from digestive tract infections were efficient biofilm-formers, whereas strains isolated from other locations were poor biofilm-formers (Auger et al., Reference Auger, Ramarao, Faille, Fouet, Aymerich and Gohar2009b). This organism appears to form biofilms preferentially at the air–liquid interface (Wijman et al., Reference Wijman, de Leeuw, Moezelaar, Zwietering and Abee2007) and motility promotes biofilm formation in this condition (Houry et al., Reference Houry, Briandet, Aymerich and Gohar2010). The addition of exogenous AI-2 inhibits biofilm formation by B. cereus; furthermore, the addition of exogenous AI-2 also promotes the dispersion of cells from preformed biofilms (Auger et al., Reference Auger, Krin, Aymerich and Gohar2006). B. cereus biofilms can be a site for spore formation and release. Biofilm formation represents a problem for the food industry, because B. cereus biofilms are more resistant to cleaning procedures than their planktonic counterparts (Wijman et al., Reference Wijman, de Leeuw, Moezelaar, Zwietering and Abee2007). For example, hot-alkali resistant spores from B. cereus isolated from dairy silo tanks were able to germinate and form biofilms in whole milk (Shaheen et al., Reference Shaheen, Svensson, Andersson, Christiansson and Salkinoja-Salonen2010).
B. anthracis is an endospore-forming bacterium and is the etiological agent of pulmonary, gastrointestinal and cutaneous anthrax. Anthrax infections are part of the natural lifecycle of many ruminants in North America, including cattle and bison, and in other parts of the world (Lee et al., Reference Lee, Costerton, Ravel, Auerbach, Wagner, Keim and Leid2007). B. anthracis readily forms biofilms under static and shear conditions and these biofilms are inherently resistant to commonly used antibiotics (Lee et al., Reference Lee, Costerton, Ravel, Auerbach, Wagner, Keim and Leid2007). In B. anthracis, sporulation is regulated during biofilm growth which is likely the result of nutrient limitation and other stresses. Inactivation of the genes encoding enzymes involved in the biosynthesis of polyphosphate in B. cereus resulted in motility and biofilm-formation defects (Shi et al., Reference Shi, Rao and Kornberg2004). Homologous enzymes have been identified in B. anthracis and they may represent attractive targets for the treatment of anthrax. Recently, Schuch and Fischetti (Reference Schuch and Fischetti2009) demonstrated that lysogeny can block or promote sporulation. The effects of lysogeny are dependent on the type of bacteriophage present. Lysogeny can also induce EPS expression and biofilm formation in B. anthracis. The complete role of biofilm in the ecology of this pathogen is yet to be understood.
Bartonella henselae
Bartonella henselae is a fastidious bacterial pathogen of cats and humans. Pilin expression is associated with autoagglutination in liquid cultures. Pilins are also required for the agar-pitting phenotype and for biofilm formation; however, components other than pilins are also required for the mentioned phenotype (Kyme et al., Reference Kyme, Dillon and Iredell2003).
Bordetella bronchiseptica and Bordetella parapertussis
Bordetellae colonize the respiratory tracts of humans and animals and cause a wide array of respiratory diseases. These bacteria are capable of living as sessile communities on a number of abiotic surfaces (Parise et al., Reference Parise, Mishra, Itoh, Romeo and Deora2007). B. bronchiseptica is associated with a variety of respiratory diseases in animals, whereas B. parapertussis is associated with non-progressive pneumonia in sheep. Various Bordetella species, including B. bronchiseptica and B. parapertussis, produce PGA (Parise et al., Reference Parise, Mishra, Itoh, Romeo and Deora2007). Biofilm formation under static hydrodynamic conditions does not require PGA in the initial stages, but PGA contributes to the stability and the maintenance of the complex architecture of Bordetella biofilms. In addition to PGA, a xylose polymer was also detected in the biofilm matrix of B. bronchiseptica (Irie et al., Reference Irie, Preston and Yuk2006). The BvgAS signal transduction system regulates biofilm development in Bordetella (Irie et al., Reference Irie, Mattoo and Yuk2004; Mishra et al., Reference Mishra, Parise, Jackson, Wozniak and Deora2005). Biofilm also appears to develop during Bordetella infection. For example, when nasal tissues of mice infected with B. bronchiseptica were examined by immunofluorescence and scanning electron microscopy (Sloan et al., Reference Sloan, Love, Sukumar, Mishra and Deora2007), B. bronchiseptica was able to form robust biofilms attached to nasal epithelium. The biofilm formed in vivo displayed the same architectural characteristics observed in biofilms formed in vitro on inert surfaces.
Bordetella biofilms are highly tolerant to a number of antimicrobial agents, which include antibiotics recommended for the treatment of veterinary and human infections caused by these bacteria (Mishra et al., Reference Mishra, Parise, Jackson, Wozniak and Deora2005). Interestingly, it was shown that rhamnolipids, a biosurfactant secreted by P. aeruginosa, dispersed B. bronchiseptica biofilms (Irie et al., Reference Irie, O'Toole and Yuk2005).
Brucella melitensis
Brucella spp. are intracellular pathogens and the etiological agents of brucellosis, a worldwide zoonosis affecting a broad range of mammals (Uzureau et al., Reference Uzureau, Godefroid, Deschamps, Lemaire, De Bolle and Letesson2007). Mutations of the QS-dependent regulator VjbR lead to drastic surface modifications in B. melitensis including overproduction of a matrix-forming EPS (Uzureau et al., Reference Uzureau, Godefroid, Deschamps, Lemaire, De Bolle and Letesson2007). This study was the first to suggest that B. melitensis can form a biofilm.
Burkholderia pseudomallei
B. pseudomallei is the etiological agent of melioidosis. The ability of B. pseudomallei to produce biofilm varies in each isolate and the source of the isolate is not indicative of its ability to form biofilm (Taweechaisupapong et al., Reference Taweechaisupapong, Kaewpa, Arunyanart, Kanla, Homchampa, Sirisinha, Proungvitaya and Wongratanacheewin2005). Inactivation of the rpoE operon found in B. pseudomallei resulted in a reduced ability to form biofilms (Korbsrisate et al., Reference Korbsrisate, Vanaporn, Kerdsuk, Kespichayawattana, Vattanaviboon, Kiatpapan and Lertmemongkolchai2005). Biofilm formation on PVC is independent of pilA, which encodes the type IVA pilin (Boddey et al., Reference Boddey, Flegg, Day, Beacham and Peak2006). Mutations in the flagellin genes resulted in markedly reduced biofilm formation, whereas mutations in genes encoding the capsule and O-side chains of lipopolysaccharide (LPS) had no effect on biofilm formation (Sawasdidoln et al., Reference Sawasdidoln, Taweechaisupapong, Sermswan, Tattawasart, Tungpradabkul and Wongratanacheewin2010). A polyphosphate kinase mutant, which is deficient in swimming and swarming motility, forms a biofilm that is less dense than that of the wild-type strain (Tunpiboonsak et al., Reference Tunpiboonsak, Mongkolrob, Kitudomsub, Thanwatanaying, Kiettipirodom, Tungboontina and Tungpradabkul2010). Finally, a c-di-GMP phosphodiesterase (cdpA) mutant had higher intracellular levels of c-di-GMP, produced more EPS, autoaggregated more, lacked flagella and swimming motility and had enhanced biofilm formation (Lee et al., Reference Lee, Gu, Ching, Lam and Chua2010).
When isolates of B. pseudomallei were cultured as biofilms, their resistance to all antimicrobial agents increased despite uneven amounts of biofilm production among isolates (Sawasdidoln et al., Reference Sawasdidoln, Taweechaisupapong, Sermswan, Tattawasart, Tungpradabkul and Wongratanacheewin2010). In contrast, virtually all isolates cultured as planktonic cells were susceptible to the antimicrobial agents studied, which included doxycycline, ceftazidime, imipenem and trimethoprim/sulfamethoxazole.
Campylobacter coli and Campylobacter jejuni
Several members of the Campylobacter genus are pathogenic and are responsible for causing a range of diseases in humans and domesticated animals. Thermophilic campylobacters, especially C. jejuni and C. coli, are the major etiological agents of foodborne gastrointestinal infections in the developed world (Murphy et al., Reference Murphy, Carroll and Jordan2006; Peyrat et al., Reference Peyrat, Soumet, Maris and Sanders2008; Gunther and Chen, Reference Gunther and Chen2009; Sulaeman et al., Reference Sulaeman, Le Bihan, Rossero, Federighi, Dé and Tresse2010). Post-infection complications include reactive arthritis and Guillain–Barré syndrome, an immune-mediated disorder affecting the peripheral nervous system (Sulaeman et al., Reference Sulaeman, Le Bihan, Rossero, Federighi, Dé and Tresse2010).
The most important source of Campylobacter is poultry, pig and bovine meat. Campylobacter has a high occurrence throughout the meat production and processing chain (Sulaeman et al., Reference Sulaeman, Le Bihan, Rossero, Federighi, Dé and Tresse2010). A recent study by Peyrat et al. (Reference Peyrat, Soumet, Maris and Sanders2008) indicates that C. jejuni is able to survive on the surface of meat processing equipment despite robust cleaning and disinfection. The surviving C. jejuni may subsequently contaminate carcasses during the slaughter process.
In general, Campylobacter are fastidious and very sensitive to atmospheric oxygen levels (Gunther and Chen, Reference Gunther and Chen2009). They encounter many stresses in the host intestinal tract, on processed meat and in the environment. However, they have developed survival mechanisms to overcome these stresses (reviewed by Murphy et al., Reference Murphy, Carroll and Jordan2006). Biofilm formation has been suggested as a possible means of persistence for Campylobacter (Murphy et al., Reference Murphy, Carroll and Jordan2006; Gunther and Chen, Reference Gunther and Chen2009). For example, C. jejuni starts to develop into a biofilm in response to aerobic stress or other stressful conditions. The formation of biofilms allows for survival during detrimental conditions, and the biofilm can act as a reservoir of planktonic cells (Reuter et al., Reference Reuter, Mallett, Pearson and van Vliet2010). The ability to form biofilm on different surfaces (glass, stainless steel and polystyrene plastic) by representative strains of 14 Campylobacter species was investigated (Gunther and Chen, Reference Gunther and Chen2009). The results obtained suggest that the anaerobic Campylobacter species are able to form biofilm more readily than the microaerophilic species; however, further investigation is required to determine if those trends apply to a wider range of isolates.
Campylobacter can form monospecies biofilms as wells as join pre-established multispecies biofilms (Sulaeman et al., Reference Sulaeman, Le Bihan, Rossero, Federighi, Dé and Tresse2010). For example, it was shown that biofilms isolated from chicken houses enhance the survival of C. jejuni (Trachoo et al., Reference Trachoo, Frank and Stern2002). The number of viable C. jejuni determined by direct viable count was greater than by standard enumeration method. This suggests that C. jejuni can adopt a viable but non-culturable state within biofilms. Recently, it was determined that C. jejuni attachment is facilitated by pre-established biofilms found in poultry environments (Hanning et al., Reference Hanning, Jarquin and Slavik2008). Additionally the survival of culturable C. jejuni was extended in certain pre-established biofilms (Hanning et al., Reference Hanning, Jarquin and Slavik2008). Further investigation showed no evidence of interspecies signaling indicating that the attachment of C. jejuni to pre-established biofilm was mediated by bacterial surface components. The above-mentioned examples clearly indicate that the control of any type of biofilms is critical because pre-established biofilm communities can trap C. jejuni and may therefore be important in the transmission and prevalence of C. jejuni. The presence of biofilm microbiota also decreased the effectiveness of many sanitizers used to control C. jejuni; however, chlorine completely inactivated C. jejuni enclosed in a biofilm (Trachoo and Frank, Reference Trachoo and Frank2002).
C. jejuni has the ability to form biofilms in the water supplies and plumbing systems of animal husbandry facilities and animal-processing plants. These biofilms may provide a continual inoculum for domesticated animals (Reeser et al., Reference Reeser, Medler, Billington, Jost and Joens2007). C. jejuni can form biofilms on a variety of abiotic surfaces commonly used in water systems, such as acrylonitrile butadiene styrene and PVC plastics. Biofilm formation by C. jejuni is inhibited in the presence of nutrient-rich media or high osmolarity, and is enhanced under thermophilic and microaerophilic conditions. Therefore, nutritional and environmental conditions affect biofilm formation in C. jejuni. Recently, it was determined that biofilm formation in C. jejuni increased under aerobic conditions when compared to microaerobic conditions, but the final biofilm levels were comparable after 3 days (Reuter et al., Reference Reuter, Mallett, Pearson and van Vliet2010). The aerobic conditions utilized were similar to those found during meat production and processing.
Adhesion to an inert surface (the first step of biofilm formation) by C. jejuni and C. coli strains was compared using the BioFilm Ring Test® (Sulaeman et al., Reference Sulaeman, Le Bihan, Rossero, Federighi, Dé and Tresse2010). The adherence ability of the strains tested ranged from no adhesion to strong adhesion; no strains of C. coli were strongly adherent to the surface. Interestingly, strains isolated from animals or carcasses were less adherent than those isolated from food-processing equipment and clinical cases suggesting that certain environments such as food-processing equipment and the human body can select for strains with greater adhesion. A recent study postulated that agar-grown C. jejuni do not colonize young chickens as well as planktonic cells, suggesting that ‘biofilm cells’ may have poor colonizing abilities (Hanning et al., Reference Hanning, Donoghue, Jarquin, Kumar, Aguiar, Metcalf, Reyes-Herrera and Slavik2009).
Both flagella (flaAB) and QS (luxS) appear to be required for optimum biofilm formation in C. jejuni (Reeser et al., Reference Reeser, Medler, Billington, Jost and Joens2007). Furthermore, a flagellated but non-motile (motA) mutant did not form biofilm to the level exhibited by the wild-type strain. This suggests that motility as well as flagella is required for biofilm formation (Moe et al., Reference Moe, Mimura, Ohnishi, Wake, Yamazaki, Nakai and Misawa2010). At an early stage, flagella are likely to play an important role in biofilm formation, because motility is necessary for cells to gather and form microcolonies. Thereafter, the flagella appear to act as bridges for the formation of net-like connections between the organisms. Although the flagella appear to be important for biofilm formation, aflagellated strains were able to form more biofilm under aerobic conditions. This suggests that biofilm formation can occur in a flagella-dependent and flagella-independent manner in C. jejuni (Reuter et al., Reference Reuter, Mallett, Pearson and van Vliet2010). Interestingly, mutants (waaF and lgtF) lacking the lipooligosaccharide (LOS) outer core exhibited enhanced biofilm formation, implicating the cell envelope in biofilm formation by C. jejuni and highlighting the dynamic nature of the cell envelope (Naito et al., Reference Naito, Frirdich, Fields, Pryjma, Li, Cameron, Gilbert, Thompson and Gaynor2010). A number of regulatory proteins have been shown to have a role in biofilm formation by C. jejuni. Deletion of a gene encoding a histidine kinase sensor (cprS) enhanced biofilm formation (Svensson et al., Reference Svensson, Davis, MacKichan, Allan, Pajaniappan, Thompson and Gaynor2009), whereas the absence of the global regulator CsrA reduced biofilm formation (Fields and Thompson, Reference Fields and Thompson2008). Finally, a spoT mutant, defective for the stringent response, reacted more to calcofluor white and formed more biofilm than the wild-type strain (McLennan et al., Reference McLennan, Ringoir, Frirdich, Svensson, Wells, Jarrell, Szymanski and Gaynor2008). Calcofluor binds to β1-3 and β1-4 carbohydrate linkages.
Clostridium perfringens
Clostridium perfringens is an anaerobic pathogen that causes a variety of infections in animals and humans, including gas gangrene and intestinal diseases. Varga et al. (Reference Varga, Therit and Melville2008) were the first to study biofilm formation by C. perfringens. Biofilms were formed under static conditions with an anaerobic atmosphere for a period of up to 5 days. Under these conditions C. perfringens formed a flat biofilm that was 30–40 μm thick. Type IV pilus-dependent gliding motility and the catabolite control protein (CcpA), a key regulator of the response to carbohydrate limitation, were needed for maximal biofilm formation. Finally, biofilm cells had a 5- to 15-fold-increase in resistance to penicilin G when compared to planktonic cells.
Corynebacterium pseudotuberculosis and Corynebacterium renale
To form biofilms, a lymphadenitis isolate of Corynebacterium pseudotuberculosis and a pyelonephritis isolate of Corynebacterium renale required the addition of fetal bovine serum and incubation under 10% CO2 for 24 h (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). When cultured as biofilms, isolates of C. renale and C. pseudotuberculosis were highly resistant to the antimicrobial agents tested, but were sensitive to the same antimicrobial agents when cultured as planktonic cells. Infections caused by these bacteria require prolonged antimicrobial therapy and are often unresponsive to treatment (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). This suggests that C. renale and C. pseudotuberculosis form biofilms during infection.
Enterococcus
Enterococci are recognized as opportunistic pathogens. They are natural inhabitants of the oral cavity, the intestinal tract and the female genital tract of humans and animals (Mohamed and Huang, Reference Mohamed and Huang2007). Enterococci are common human nosocomial agents and vancomycin-resistant strains are of particular interest. The two most common enterococci species are Enterococcus faecalis and Enterococcus faecium, and both are capable of forming biofilms (Mohamed and Huang, Reference Mohamed and Huang2007). Many environmental and genetic factors are or have been proposed to be associated with the production of biofilm (reviewed by Mohamed and Huang, Reference Mohamed and Huang2007). A gene cluster involved in polysaccharide biosynthesis (epa, enterococcal polysaccharide antigen) was shown to be uniformly present in E. faecalis strains (Teng et al., Reference Teng, Singh, Bourgogne, Zeng and Murray2009). Disruption of the genes in this cluster resulted in mutants with deficient biofilm formation. The E. faecalis biofilm matrix contains DNA and it was shown by Guiton et al. (Reference Guiton, Hung, Kline, Roth, Kau, Hayes, Heuser, Dodson, Caparon and Hultgren2009) that sortase A (SrtA) and autolysin (Atn) have a role in the release of DNA during biofilm development. Recently, a comprehensive analysis of genetic determinants of biofilm formation in the core genome of E. faecalis was carried out (Ballering et al., Reference Ballering, Kristich, Grindle, Oromendia, Beattie and Dunny2009). Sixty-eight genetic loci predicted to be involved in biofilm formation were identified by RIVET (recombinase in vivo expression technology). Most of these genes had not been studied previously and many are highly conserved in Gram-positive pathogens and may thus constitute a pool of uncharacterized genes that may be targeted for drug discovery.
Biofilm formation was observed in 50–60% of commensal enterococci isolated from the intestine of broilers (Oliveira et al., Reference Oliveira, Santos, Fernandes, Bernardo and Vilela2010) and of E. faecalis strains isolated from chicken arthritis (Ciftci et al., Reference Ciftci, Findik, Iça, Bas, Onuk and Güngördü2009). Fsr-regulated gelatinase-positive E. faecalis that formed biofilm were relatively common in the agricultural environment such as swine and cattle feces. The agricultural environment may therefore represent a source/reservoir of clinically relevant strains (Macovei et al., Reference Macovei, Ghosh, Thomas, Hancock, Mahmood and Zurek2009). As observed with other bacteria, enterococci cultured as biofilms are more resistant to antibiotics than their planktonic counterparts (Mohamed and Huang, Reference Mohamed and Huang2007). Biofilm production in enterococci isolated from broilers also correlated with an increase in antibiotic resistance (Oliveira et al., Reference Oliveira, Santos, Fernandes, Bernardo and Vilela2010). Additionally, slime-producing E. faecalis strains isolated from chickens suffering from arthritis were found to be more resistant to antibiotics (Ciftci et al., Reference Ciftci, Findik, Iça, Bas, Onuk and Güngördü2009).
Erysipelothrix rhusiopathiae
Erysipelothrix rhusiopathiae causes erysipelas in animals and erysipeloid in humans. Two surface proteins (RspA and RspB) of E. rhusiopathiae bind to fibronectin, and type I and type IV collagens. These two surface proteins also participate in the initiation of biofilm formation by binding to abiotic and biotic surfaces (Shimoji et al., Reference Shimoji, Ogawa, Osaki, Kabeya, Maruyama, Mikami and Sekizaki2003).
Escherichia coli
With thousands of serotypes, E. coli is a very diverse species that is a part of the normal intestinal microbiota, and can be an important intestinal pathogen or invade the blood stream and cause meningitis (Beloin et al., Reference Beloin, Roux and Ghigo2008). Biofilm formation by several E. coli strains has been studied extensively. Furthermore, E. coli strains will compete among themselves to establish colonies within a host or a niche. For example, it was established that the probiotic E. coli strain Nissle 1917 (serotype O6:K5:H1) was a good biofilm former and can out-compete pathogenic strains of E. coli (Hancock et al., Reference Hancock, Dahl and Klemm2010). The biofilm matrix of E. coli is composed of several EPS, but LPS and capsular polysaccharides do not usually accumulate in the matrix; however, LPS and capsule play an important role during biofilm formation. Cellulose (Zogaj et al., Reference Zogaj, Nimtz, Rhode, Bokranz and Römling2001), PGA (Agladze et al., Reference Agladze, Wang and Romeo2005) and colanic acid (Prigent-Combaret et al. Reference Prigent-Combaret, Prensier, Le Thi, Vidal, Lejeune and Dorel2000) have been detected in the biofilm matrix of E. coli. All three EPS are important for biofilm formation (Beloin et al., Reference Beloin, Roux and Ghigo2008). Several key factors (e.g. various fimbriae) are implicated in E. coli surface colonization. To ensure proper biofilm formation, the expression and activity of these factors are finely regulated at specific times and at various locations in the biofilms (Beloin et al., Reference Beloin, Roux and Ghigo2008; Wood, Reference Wood2009). Microarray analysis has elucidated several aspects of biofilm formation in E. coli. The analysis resulted in the discovery of the role of stresses, intra- and inter-species cell signaling (e.g. AHLs and AI-2), toxin/antitoxin genes (e.g. Hha/TomB and MqsR/B3021) and small RNAs (e.g. CsrB) on biofilm formation and dispersal (reviewed by Wood, Reference Wood2009). One common trend among different biofilm transcriptome studies was that stress genes were induced during biofilm formation.
Olson et al. (Reference Olson, Ceri, Morck, Buret and Read2002) found that E. coli strains isolated from cases of bovine or turkey enteritis were able to form biofilms. Olson et al. (Reference Olson, Ceri, Morck, Buret and Read2002) also noted that enrofloxacin and gentamicin were effective antibiotics against the biofilms of these enteritis E. coli isolates. The data collected by Olson et al. (Reference Olson, Ceri, Morck, Buret and Read2002) suggest that established E. coli biofilms may be difficult to treat with some antibiotics and this is supported by observations made in clinical cases involving pig, cattle and poultry.
Some strains of enterohemorrhagic E. coli O157:H7, a worldwide foodborne pathogen, are able to form biofilms. Recently, a genome-wide transposon mutagenesis of E. coli O157:H7 strain EDL933 revealed that virulence plasmid pO157 plays an essential role during biofilm formation. Specifically espP, an autotransporter serine protease, and ehxD, the enterohemolysin translocator, were identified as mediators of biofilm formation (Puttamreddy et al., Reference Puttamreddy, Cornick and Minion2010). Strain EDL933 was cured of plasmid pO157 and the resulting strain failed to establish a biofilm. This confirmed the essential role of pO157 during biofilm formation. Other studies indicate that the biofilm negative strains of E. coli O157:H7 can associate with pre-established biofilms generated by commensal E. coli strains (Uhlich et al., Reference Uhlich, Rogers and Mosier2010). Furthermore, E. coli O157:H7 strain 0475s enclosed in a multi-species biofilm survived a H2O2 challenge better than its planktonic counterpart.
Francisella tularensis
Francisella tularensis is associated with water and waterways and infects many species of animals, insects and protists (Durham-Colleran et al., Reference Durham-Colleran, Verhoeven and van Hoek2010). Tularemia is commonly spread by arthropod vectors such as mosquitoes, biting flies and ticks. The mechanisms utilized by Francisella to survive in its natural environment are yet to be elucidated; however, biofilm formation plays a critical role in the survival of another arthropod-borne bacterium, Y. pestis (see below). Durham-Colleran et al. (Reference Durham-Colleran, Verhoeven and van Hoek2010) recently demonstrated for the first time that F. tularensis subsp. novicida (or F. novicida) forms a biofilm in vitro. Biofilm formation is regulated by the orphan response regulator, QseB. F. novicida is less virulent than F. tularensis, and is widely used as a model organism for the F. tularensis species. The data collected by Durham-Colleran et al. (Reference Durham-Colleran, Verhoeven and van Hoek2010) suggest that biofilm formation may be important for the lifecycle of F. tularensis. It was recently shown that biofilm formation by F. tularensis promotes persistence on chitin surfaces which can act as a carbon source (Margolis et al., Reference Margolis, El-Etr, Joubert, Moore, Robison, Rasley, Spormann and Monack2010).
Haemophilus parasuis
Haemophilus parasuis is the etiological agent of Glässer's disease in pigs. The ability to form biofilms by field isolates and reference strains was tested in glass tubes and polystyrene microtiter plates (Jin et al., Reference Jin, Zhou, Kang, Luo, Cai and Chen2006). In general, non-virulent serovars formed more biofilms than virulent serovars. In pigs experimentally infected with biofilm-positive strains, bacteria recovered from the nasal cavities remained biofilm positive, whereas bacteria recovered from the lung and brain became biofilm negative. These observations indicate that most serovars of H. parasuis can form biofilms in vitro and the ability to form biofilms is associated with the recovery site of the strains. The ability to form biofilms is maintained during in vitro passages and after infection in the upper respiratory tract. Recently, selective capture of transcribed sequences (SCOTS) was used to identify H. parasuis genes upregulated in necrotic lungs 7 days after the challenge (Jin et al., Reference Jin, Wan, Zhou, Li, Luo, Zhang, Hu, Langford and Chen2008). The data collected by Jin et al. (Reference Jin, Wan, Zhou, Li, Luo, Zhang, Hu, Langford and Chen2008) support the role of biofilm formation by H. parasuis during colonization and/or persistence. Our group has recently made a similar observation. In an in vitro assay, non-virulent strains isolated from the nasal cavities of pigs tend to form more biofilms than did virulent strains isolated from systemic lesions (V. Deslandes, M. Jacques and V. Aragon, unpublished results).
Histophilus somni
Histophilus somni (Haemophilus somnus) is an obligate inhabitant of mucosal surfaces in cattle and sheep. H. somni is an opportunistic pathogen associated with a variety of conditions such as respiratory disease, meningoencephalitis, myocarditis, arthritis and other systemic infections (Sandal et al., Reference Sandal, Hong, Swords and Inzana2007; Corbeil, Reference Corbeil2008). H. somni is also one of the primary agents responsible for bovine respiratory disease complex (Corbeil, Reference Corbeil2008). All H. somni strains examined were able to form biofilms on PVC wells. The majority of isolates from systemic sites produced more biofilm than commensal strains isolated from prepuces (Sandal et al., Reference Sandal, Hong, Swords and Inzana2007). H. somni also formed biofilms in flow cells and the biofilm development went through the stages of attachment, growth, maturation and detachment. Furthermore, H. somni formed biofilms in cardiopulmonary tissue following experimental respiratory infection in the bovine host (Sandal et al., Reference Sandal, Shao, Annadata, Apicella, Boye, Jensen, Saunders and Inzana2009). Biofilms were evident and most prominent in the myocardium, and were associated with a large amount of amorphous extracellular material. After transposon mutagenesis of H. somni strain 2336, mutants that formed enhanced biofilm or did not form biofilm were selected and identified (Sandal et al., Reference Sandal, Shao, Annadata, Apicella, Boye, Jensen, Saunders and Inzana2009). Several mutants deficient in biofilm formation had an insertion in the gene encoding for a homologue of filamentous hemagglutinin (FHA), which is predicted to be involved in attachment. The formation of biofilm may therefore be crucial to H. somni persistence in vivo and the formation of a robust biofilm may provide a selective advantage for pathogenic strains that cause systemic disease. Surprisingly, both planktonic and biofilm cells of H. somni (a bovine pneumonia isolate) were equally sensitive to antimicrobial agents (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002).
Leptospira spp
Leptospira spp. belong to the bacterial phylum Spirochaetes. Leptospires exist as aquatic saprophytic organisms or as pathogens. Leptospirosis is a widespread zoonosis and humans are usually infected through cut or abraded skin that comes into contact with water contaminated with the urine of mammals. Both saprophytic (e.g. Leptospira biflexa) and pathogenic (e.g. Leptospira interrogans, Leptospira borgpetersenii and Leptospira kirschneri) species formed biofilms on glass and polystyrene surfaces (Ristow et al., Reference Ristow, Bourhy, Kerneis, Schmitt, Prevost, Lilenbaum and Picardeau2008). Electron microscopy images showed cells embedded in an extracellular matrix. The formation of such a biofilm is consistent with the aquatic life style of saprophytic strains and may help pathogenic strains to survive in their environmental habitats and to colonize their host.
Listeria monocytogenes
The food-borne pathogen Listeria monocytogenes is the causative agent of listeriosis, a severe disease with high hospitalization and fatality rates in humans (Gandhi and Chikindas, Reference Gandhi and Chikindas2007). L. monocytogenes is also an important pathogen of several animal species, including ruminants. L. monocytogenes can survive and grow in a wide range of environmental conditions such as refrigeration temperatures, low pH and high salt concentration. It can be isolated from a variety of raw and processed foods (e.g. milk and dairy products, various meats and meat products, seafood and fish products). L. monocytogenes is frequently isolated in food-processing plants, especially those involved in the meat and dairy industries. Biofilms on milking equipment on a dairy farm has been implicated as a potential source of bulk tank milk contamination with L. monocytogenes (Latorre et al., Reference Latorre, Van Kessel, Karns, Zurakowski, Pradhan, Boor, Jayarao, Houser, Daugherty and Schukken2010). Biofilms of L. monocytogenes are of particular concern, because biofilm cells are more resistant to disinfectants and sanitizing agents than are planktonic cells. Many disinfectants, including quaternary ammonium compounds and hypochloride, do not effectively kill L. monocytogenes in the presence of soil or organic matter, or at low temperatures (Amalaradjou et al., Reference Amalaradjou, Norris and Venkitanarayanan2009). However, octenidine hydrochloride, a positively charged bispyridinamine, has been shown to effectively kill planktonic cells and biofilm cells of L. monocytogenes at various temperatures (from 4 to 37°C) and in the presence of organic matter (Amalaradjou et al., Reference Amalaradjou, Norris and Venkitanarayanan2009).
Several studies have shown that strains of L. monocytogenes differ in their ability to adhere to surfaces and form biofilms (reviewed by Gandhi and Chikindas, Reference Gandhi and Chikindas2007). Cellular hydrophobicity, however, appears to be an important factor during the initial adherence to PVC (Takahashi et al., Reference Takahashi, Suda, Tanaka and Kimura2010). L. monocytogenes can form monospecies or multispecies biofilms. To study multispecies biofilms, different types of Lactococcus lactis biofilms that exhibited different architectures, porosities, types of matrices and individual cell surface properties were used to investigate factors governing the initial attachment of L. monocytogenes to biofilms (Habimana et al., Reference Habimana, Meyrand, Meylheuc, Kulakauskas and Briandet2009). It was observed that the adhesion of planktonic L. monocytogenes to L. lactis biofilm was lower than to an abiotic surface. Adhesion of L. monocytogenes was almost prevented by the presence of the EPS produced by L. lactis. The presence of biofilms that can prevent the contamination of surfaces by L. monocytogenes can perhaps constitute a novel approach for controlling L. monocytogenes. However, a porous L. lactis biofilm can also enhance L. monocytogenes attachment.
Biofilm development in L. monocytogenes involves flagellar motility; when motility is blocked, the initial attachment is decreased but it later results in the formation of a high-density biofilm (Todhanakasem and Young, Reference Todhanakasem and Young2008). The L. monocytogenes Agr peptide-sensing system, which encodes for a putative QS peptide (Riedel et al., Reference Riedel, Monk, Casey, Waidmann, Gahan and Hill2009) has also been studied for its role in biofilm formation by creating a deletion mutant in agrD. The agrD mutant had reduced ability to form biofilm and to invade Caco-2 intestinal epithelial cells. The virulence of the argD mutant was also attenuated in a mouse model. It has been recently demonstrated that extracellular DNA may be the central component of the matrix of the L. monocytogenes biofilm because DNase I treatment dispersed the biofilm and exogenous DNA could not restore biofilm formation (Harmsen et al., Reference Harmsen, Lappann, Knochel and Molin2010a).
Mannheimia haemolytica
A bovine pneumonia isolate of Mannheimia haemolytica formed a biofilm when cultured in the presence of fetal bovine serum and incubated under 10% CO2 for 24 h (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). Surprisingly, planktonic and biofilm M. haemolytica had similar levels of sensitivity to antimicrobial agents with the exception of trimethroprim/sulfadoxine.
Mycobacterium
Mycobacterium avium subsp. avium causes tuberculosis in domestic and wild birds, while M. avium subsp. hominissuis is an opportunistic pathogen of humans and swine, and occasionally of other mammals (Johansen et al., Reference Johansen, Agdestein, Olsen, Nilsen, Holstad and Djonne2009). An optimized method to screen human, swine and avian isolates of M. avium was established recently (Johansen et al., Reference Johansen, Agdestein, Olsen, Nilsen, Holstad and Djonne2009). After an incubation of 2–3 weeks, nine swine isolates produced biofilm, but none of the human or avian isolates formed biofilms. However, some human M. avium strains were previously shown to form biofilm and the use of a green-fluorescent protein promoter library and transposon mutagenesis allowed the identification of genes associated with biofilm formation (Yamazaki et al., Reference Yamazaki, Danelishvili, Wu, MacNab and Bermudez2006b). Most of the genes identified by Yamazaki et al. (Reference Yamazaki, Danelishvili, Wu, MacNab and Bermudez2006b) were involved in glycopeptidolipids (GPL) biosynthesis. Interestingly, biofilm-negative mutants were also impaired in the invasion of the bronchial epithelial cell line BEAS-2B (Yamazaki et al., Reference Yamazaki, Danelishvili, Wu, Hidaka, Katsuyama, Stang, Petrofsky, Bildfell and Bermudez2006a).
M. avium subsp. paratuberculosis (Map) is the causative agent of Johne's disease, a chronic enteric infection affecting ruminants (Cook et al., Reference Cook, Britt and Bolster2010). Map is transmitted through the fecal–oral route including indirect transmission via ingestion of contaminated materials in the farm environment. The ability of Map to persist in a multispecies biofilm on materials commonly used to construct livestock watering troughs (concrete, plastic, galvanized or stainless steel) was evaluated (Cook et al., Reference Cook, Britt and Bolster2010). It was found that Map encased in mixed biofilms survived for an extended period of time on livestock watering trough materials. To avoid the exposure of susceptible farm animals to Map, management practices for Johne's disease should be aimed at maintaining trough surfaces free of biofilm. It is known that biofilm formation is linked to GPLs, a major component of the mycobacterial cell wall (Wu et al., Reference Wu, Schmoller, Bannantine, Eckstein, Inamine, Livesey, Albrecht and Talaat2009). Recently, a new cell wall lipopeptide was shown to be important for biofilm formation and the pathogenicity of Map (Wu et al., Reference Wu, Schmoller, Bannantine, Eckstein, Inamine, Livesey, Albrecht and Talaat2009).
Biofilm formation has also been observed in Mycobacterium bovis strain BCG and Mycobacterium tuberculosis (Ojha et al., Reference Ojha, Baughn, Sambandan, Hsu, Trivelli, Guerardel, Alahari, Kremer, Jacobs and Hatfull2008). In M. tuberculosis, the extracellular matrix is rich in free mycolic acids and harbors an important drug-tolerant sub-population. This sub-population persisted despite exposure to high levels of isoniazid or rifampicin. Finally, it was also noted that subinhibitory concentrations of clarithromycin, but not moxifloxacin, inhibits biofilm formation by human isolates of M. avium; however, clarithromycin has no activity against pre-established biofilms (Carter et al., Reference Carter, Young and Bermudez2004).
Mycoplasma
Despite their small genome size, mycoplasmas cause a wide range of disease in both humans and animals (McAuliffe et al., Reference McAuliffe, Ellis, Miles, Ayling and Nicholas2006). For example, Mycoplasma spp., typically Mycoplasma bovis, are important bovine pathogens that cause mastitis, metritis, pneumonia and arthritis (Justice-Allen et al., Reference Justice-Allen, Trujillo, Corbett, Harding, Goodell and Wilson2010). McAuliffe et al. (Reference McAuliffe, Ellis, Miles, Ayling and Nicholas2006) examined a variety of mycoplasma species and found considerable variation in their ability to form biofilms in an air–liquid interface model. For example, Mycoplasma agalactiae and M. bovis produced thick and dense biofilms. On the other hand, the highly virulent causative agent of contagious bovine pleuropneumonia, Mycoplasma mycoides subsp. mycoides SC, was unable to form biofilm. Compared to their planktonic counterpart, biofilm cells were more resistant to stresses, including heat and desiccation. Furthermore, a correlation between the ability to form biofilms and specific molecular genotypes was established for M. bovis (McAuliffe et al., Reference McAuliffe, Ellis, Miles, Ayling and Nicholas2006). However, when a simple model (growth on a membrane placed on an agar plate) lacking an air–liquid interface is used, M. mycoides subsp. mycoides SC can form biofilms (McAuliffe et al., Reference McAuliffe, Ayling, Ellis and Nicholas2008). As with the air–liquid interface model, the biofilms formed on a membrane were more resistant to many stresses, including heat, osmotic shock and oxidative stress. Additionally, mycoplasmas cultured on a membrane showed remarkable persistence and were viable for up to 20 weeks.
The murine respiratory pathogen Mycoplasma pulmonis can form biofilms on the epithelium of explanted trachea (Simmons and Dybvig, Reference Simmons and Dybvig2009). M. pulmonis was also able to form biofilms in experimentally infected mice and these biofilms exhibited similar structure and biological characteristics when compared to their in vitro counterparts. Transposon mutants of M. pulmonis that failed to produce the glucose–galactose containing EPS-I had enhanced biofilm-formation ability on glass surfaces. The increased biofilm-formation ability likely resulted from the overproduction of a second EPS (EPS-II) containing N-acetylglucosamine (Daubenspeck et al., Reference Daubenspeck, Bolland, Luo, Simmons and Dybvig2009). When encased within a biofilm, cells of M. pulmonis producing a short form of the Vsa (variable surface antigen) were more resistant to complement killing and gramicidin than were dispersed mycoplamas (Simmons and Dybvig, Reference Simmons and Dybvig2007). The resistance appeared to be localized within cells found within the tower structures of biofilms.
The association between the occurrence of Mycoplasma spp. in recycled bedding sand and mycoplasma mastitis in cows has also been investigated (Justice-Allen et al., Reference Justice-Allen, Trujillo, Corbett, Harding, Goodell and Wilson2010). It was found that concentrations of Mycoplasma spp. in a sand pile positively correlated with the growth of Gram-negative micro-organisms. This suggests that biofilm formation by the bacterial community could account for the survival and replication of mycoplasmas.
Pasteurella multocida
Pasteurella multocida can infect several wild and domesticated animals. Diseases caused by P. multocida include fowl cholera in birds, atrophic rhinitis in pigs, hemorrhagic septicemia in ungulates, enzootic pneumonia in cattle, sheep and goats and snuffles in rabbits. P. multocida has also been recognized as a contributor to debilitating and fatal porcine pneumonia. Recent data suggest that P. multocida can form biofilms in the porcine lung (Ross, Reference Ross2007). Olson et al. (Reference Olson, Ceri, Morck, Buret and Read2002) used the Calgary Biofilm Device to study biofilm formation by bovine pneumonia isolates and chicken cholera isolates of P. multocida in the presence of fetal bovine serum and 10% CO2. The MIC and the MBEC values of planktonic cultures and biofilm cultures were similar for the antibiotics tested with the exception of trimethroprim/sulfadoxine. These observations correlate with clinical cases because animals with pasteurellosis respond well to most antimicrobial agents if no secondary infection is present (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002).
Pseudomonas aeruginosa
P. aeruginosa is found in various environments, especially in soil. P. aeruginosa is an opportunistic pathogen responsible for chronic lung infections in cystic fibrosis patients and infections in immunocompromised individuals (Bazire et al., Reference Bazire, Shioya, Soum-Soutéra, Bouffartigues, Ryder, Guentas-Dombrowsky, Hémery, Linossier, Chevalier, Wozniak, Lesouhaitier and Dufour2010; Ma et al., Reference Ma, Conover, Lu, Parsek, Bayles and Wozniak2009). The biofilm lifestyle of P. aeruginosa is well characterized and is often used as a model organism for biofilm formation (for a recent review see Harmsen et al., Reference Harmsen, Yang, Pamp and Tolker-Nielsen2010b). P. aeruginosa will form biofilm both in the environment and in its host during an infection. At least three EPS are synthesized during biofilm formation: Psl (polysaccharide synthesis locus), Pel (pellicle formation) and alginate (reviewed by Ryder et al., Reference Ryder, Byrd and Wozniak2007). Recent data indicate that Psl is a key component required for proper scaffolding of the matrix (Ma et al., Reference Ma, Conover, Lu, Parsek, Bayles and Wozniak2009). Alginate is a main component of the biofilm matrix of mucoid strains. The extracellular function sigma factor AlgU (also known as AlgT, RpoE, σE and σ22) is responsible for transcription of the alginate biosynthetic operon. An algU mutant showed a dramatic impairment in biofilm formation under dynamic conditions (Bazire et al., Reference Bazire, Shioya, Soum-Soutéra, Bouffartigues, Ryder, Guentas-Dombrowsky, Hémery, Linossier, Chevalier, Wozniak, Lesouhaitier and Dufour2010). Extracellular DNA is also considered an important component of the biofilm matrix of P. aeruginosa because extracellular DNA acts as a component for cell-to-cell connection in the biofilm (Ma et al., Reference Ma, Conover, Lu, Parsek, Bayles and Wozniak2009). Furthermore, the extracellular DNA found in P. aeruginosa biofilm matrix was shown to induce a proinflammatory response by neutrophils (Fuxman Bass et al., Reference Fuxman Bass, Russo, Gabelloni, Geffner, Giordano, Catalano, Zorreguieta and Trevani2010). Degradation of extracellular DNA found in the biofilm matrix by DNase I resulted in a marked reduction in the ability of P. aeruginosa biofilms to induce the release of the proinflammatory cytokines IL-8 and IL-1β and the expression of the activation markers CD18, CD11b and CD66b. The absence of exogenous DNA in the biofilm matrix also led to a reduction in the number of bacteria phagocytosed by neutrophils. The number of neutrophil extracellular traps also decreased in the absence of extracellular DNA in the biofilm matrix (Fuxman Bass et al., Reference Fuxman Bass, Russo, Gabelloni, Geffner, Giordano, Catalano, Zorreguieta and Trevani2010).
Chemical gradients established in biofilms lead to heterogeneity in bacterial gene expression. Laser capture microdissection was used in combination with quantitative real-time reverse transcriptase PCR (RT-PCR) (Lenz et al., Reference Lenz, Williamson, Pitts, Stewart and Franklin2008) or 16S rRNA/rDNA ratios (Pérez-Osorio et al., Reference Pérez-Osorio, Williamson and Franklin2010) to target defined biofilm subpopulations in order to measure gene expression. In thick P. aeruginosa biofilms, cells in the 30-μm zone next to the air–biofilm interface actively expressed genes associated with stationary phase. Cells in the interior portions did not express stationary-phase-associated genes, and therefore, cells located in the center of a biofilm are likely in a late stationary phase-like state or are possibly dormant (Pérez-Osorio et al., Reference Pérez-Osorio, Williamson and Franklin2010).
Diversity in biofilm production, biofilm architecture and control of biofilm formation was observed among human cystic fibrosis isolates (Deligianni et al., Reference Deligianni, Pattison, Berrar, Ternan, Haylock, Moore, Elborn and Dooley2010). Interestingly, it was observed that biofilm-positive strains of P. aeruginosa were capable of entrapping biofilm-negative strains. The biofilm-negative strains could be observed in the mature biofilm.
The resistance to antimicrobial agents by P. aeruginosa increased when cultured as a biofilm (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). Planktonic cultures of an animal wound isolate of P. aeruginosa were sensitive to enrofloxacin, gentamicin, ampicillin, oxytetracycline and trimethoprim/sufladoxine, but when cultured as a biofilm the same isolate was sensitive to enrofloxacin only (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). P. aeruginosa infections in animals are difficult to treat and this clearly suggests that biofilm formation is an important factor during infections.
Riemerella anatipestifer
Riemerella anatipestifer causes the anatipestifer syndrome in ducks. Anatipestifer is characterized by diarrhea, lethargy and respiratory and nervous symptoms. More than 40% of the 43 isolates and reference strains tested were positive for biofilm formation (Hu et al., Reference Hu, Han, Zhou, Ding, Ding and Yu2010). Bacteria cultured as biofilms were more resistant to antibiotics and detergents than their planktonic counterparts. This suggests that biofilm formation in R. anatipestifer may contribute to the persistence of this infection on duck farms.
Salmonella
Animal-derived products, particularly poultry meat, are the main source of Salmonella infections in human. During meat and poultry processing, pathogens such as Salmonella may attach and subsequently form biofilms on a variety of surfaces (Jain and Chen, Reference Jain and Chen2007). The red, dry and rough (rdar) colony morphotype is a multicellular behavior displayed by Salmonella enterica and E. coli. Such colonies are characterized by the production and secretion of cellulose and the expression of curli fimbriae (Römling, Reference Römling2005). These rdar colonies can easily form thick biofilms on abiotic surfaces. The rdar colony phenotype has been associated with the response regulator CsgD and the c-di-GMP producing enzyme AdrA. CsgD stimulates biofilm production indirectly by activating the transcription of the curli biosynthesis operon. The production of c-di-GMP by AdrA is a crucial signal to initiate the biosynthesis of cellulose (Römling, Reference Römling2005).
S. enterica subsp. enterica serovar Typhimurium (or Salmonella Typhimurium) is the primary serovar isolated from slaughtered pigs in Europe (Van Parys et al., Reference Van Parys, Boyen, Verbrugghe, Leyman, Rychlik, Haesebrouck and Pasmans2010). Persistent infections in pigs are a major concern for food safety and human health. The role of biofilm formation in the persistence of Salmonella Typhimurium in porcine tonsils was studied by examining the contribution of biofilm-associated genes csgA, csgD and adrA. It was concluded that Salmonella Typhimurium colonized porcine tonsils in a biofilm-independent manner (Van Parys et al., Reference Van Parys, Boyen, Verbrugghe, Leyman, Rychlik, Haesebrouck and Pasmans2010).
Salmonella Typhimurium phage type DT104 is of particular importance, because this type of Salmonella Typhimurium is resistant to a core group of antibiotics such as ampicillin, chloramphenicol, streptomycin, sulfonamides and tetracycline (Kim and Wei, Reference Kim and Wei2009). Transposon mutagenesis of Salmonella Typhimurium DT104 indicated that several factors, including the production and export of exopolymeric substances, expression of flagella and regulation of exoribonucleases and RNA-binding proteins, were involved in biofilm formation and attachment to surfaces (Kim and Wei, Reference Kim and Wei2009). The Calgary Biofilm Device was used to compare the susceptibility of 3-day-old biofilms and planktonic cells of Salmonella Typhimurium to various disinfectants (Wong et al., Reference Wong, Townsend, Fenwick, Trengove and O'Handley2010). Wong et al. (Reference Wong, Townsend, Fenwick, Trengove and O'Handley2010) observed that Salmonella biofilms were less susceptible to disinfectants than were planktonic Salmonella. However, the disinfectants evaluated were able to reduce the number of viable cells enclosed in biofilms at concentrations and contact times sufficient to eliminate planktonic cells. Despite the reduction in the amount of viable cells in the biofilm, there were enough viable cells remaining to cause further contamination and potentially result in infection. In another study, the Calgary Biofilm Device was used to evaluate the susceptibily of Salmonella isolates from bovine, swine and turkey enteritis to various antimicrobial agents. As previously observed with other bacteria, Salmonella biofilms were resistant to most antibiotics tested (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002).
A study investigating the source of Salmonella contamination in broiler and layer farms in Spain found that dust, surfaces and feces were the main sources of contamination (Marin et al., Reference Marin, Hernandiz and Lainez2009). Approximately 50% of the isolates were able to produce biofilms, and S. Enteritidis was the primary serovar isolated. In addition, Marin et al. (Reference Marin, Hernandiz and Lainez2009) showed that the use of glutaraldehyde, formaldehyde and peroxygen at a concentration of 1% in field conditions was inadequate for the elimination of Salmonella in the farm.
Staphylococcus
Mastitis is an economically important and frequent disease of dairy cows. S. aureus is the primary pathogen isolated from mastitis cases (Melchior et al., Reference Melchior, Fink-Gremmels and Gaastra2006a; Reference Melchior, Vaarkamp and Fink-Gremmels2006b; Oliveira et al., Reference Oliveira, Nunes, Carneiro, Bexiga, Bernardo and Vilela2007). Coagulase-negative staphylococci (CNS), such as S. epidermidis, can also infect the mammary glands of dairy cows, goats and sheep. CNS infections are usually milder than those associated with S. aureus. In general, susceptibility to antimicrobial agents is high, but the recovery rates are poor. This suggests that during infection pathogens associated with mastitis form biofilms which facilitate their persistence in the udder (Melchior et al., Reference Melchior, Vaarkamp and Fink-Gremmels2006b).
Approximately one-third (37.5%) of S. aureus and S. epidermidis isolates from subclinical mastitis produced biofilms (Oliveira et al., Reference Oliveira, Bexiga, Nunes, Carneiro, Cavaco, Bernardo and Vilela2006). It was later observed that the majority of biofilm-positive S. aureus isolates from mastitis cases produced a detectable biofilm within 48 h. On the other hand, biofilm-positive S. epidermidis isolates from mastitis cases required 72 h to produce a detectable biofilm (Oliveira et al., Reference Oliveira, Nunes, Carneiro, Bexiga, Bernardo and Vilela2007). Biofilm production by S. aureus isolated from milk, teat skin and from milking machine unit liners has also been compared (Fox et al., Reference Fox, Zadoks and Gaskins2005). It was found that S. aureus associated with milk are more likely to produce biofilms when compared to S. aureus extramammary sources (teat skin and milking unit liners). This suggests that the biofilm producing strains of S. aureus are able to attach to mammary mucosal surfaces and cause infections at a greater rate than are biofilm-negative strains. A fluorescent in situ hybridization (FISH) protocol for the detection of biofilm formation by staphylococci in contaminated milk has been developed (Oliveira et al., Reference Oliveira, Bexiga, Nunes, Carneiro, Cavaco, Bernardo and Vilela2006). This new assay would allow for the rapid detection of biofilm-positive staphylococci in contaminated milk. Early detection is a key factor for the application of corrective measures in mastitis cases.
Several genes have been associated with biofilm formation by staphylococci. These genes encode the accessory gene regulator Agr, icaADBC which encodes the PIA/PNAG producing enzyme and transporter, and the biofilm-associated protein Bap (Tormo et al., Reference Tormo, Knecht, Götz, Lasa and Penadés2005; Melchior et al., Reference Melchior, van Osch, Graat, van Duijkeren, Mevius, Nielen, Gaastra and Fink-Gremmels2009). The IS257 genes have also been implicated in biofilm formation (Tormo et al., Reference Tormo, Knecht, Götz, Lasa and Penadés2005). There is a good correlation between the ability of S. aureus isolates from bovine subclinical mastitis to form a biofilm and the presence of the intercellular adhesion genes, icaA and icaD (Dhanawade et al., Reference Dhanawade, Kalorey, Srinivasan, Barbuddhe and Kurkure2010). Additionally, there is a strong correlation between the ability of CNS to form biofilms and the presence of bap, despite the absence of the icaADBC operon. Bap is a surface protein encoded by a gene carried in a putative transposon that is inserted in the mobile staphylococcal pathogenicity island SaPIbov 2 (Tormo et al., Reference Tormo, Knecht, Götz, Lasa and Penadés2005). The presence of a gene responsible for biofilm formation on a mobile element suggests that the ability to form biofilm can be acquired horizontally. The relation between biofilm formation and Arg type carried by S. aureus isolates from mastitis cases was also determined (Melchior et al., Reference Melchior, van Osch, Graat, van Duijkeren, Mevius, Nielen, Gaastra and Fink-Gremmels2009). Strains carrying Agr II preferred extracellular niches suggesting that biofilm formation is important for the survival of these strains. On the other hand, strains possessing Agr I were adapted for an intracellular lifestyle suggesting that biofilm formation is probably not as important for their survival. Recently, transposon analysis of a S. aureus isolate producing a proteinaceous biofilm matrix rich in extracellular DNA identified genes important for biofilm formation in a polysaccharide-independent manner. The analysis highlighted the importance of extracellular protease activity and autolysis in biofilm development (Boles et al., Reference Boles, Thoendel, Roth and Horswill2010).
In poultry, S. aureus is normally a part of the skin microbiota; however, it can also be associated with osteomyelitis, bumble foot and arthritis. S. aureus is commonly isolated from the joints, tendon sheaths and the bones of infected animals (Nemati et al., Reference Nemati, Hermans, Devriese, Maes and Haesebrouck2009). S. aureus isolates recovered from poultry between 1970 and 1972 and in 2006 were screened for the presence of biofilm-associated genes (bap, icaA and icaD), and for the presence of genes encoding microbial surface components recognizing adhesive matrix molecules (MSCRAMMs; bbp, cna, ebpS, eno, fib, fnbA, fnbB, clfA and clfB) (Nemati et al., Reference Nemati, Hermans, Devriese, Maes and Haesebrouck2009). No correlation was observed between the presence of MSCRAMM genes and biofilm-associated genes in old or recent S. aureus isolates from healthy or infected chickens. Furthermore, there is no indication that the presence of these genes has changed over time. Some of the recent isolates belonged to the animal-associated methicillin-resistant S. aureus (MRSA) ST398. All MRSA-related isolates were positive for icaD, cna, ebpS, eno, fnbA, fnbB, clfA and clfB. This suggests that MRSA ST398 isolates have the genetic potential for strong adherence which may facilitate the colonization of not only chickens but also humans.
In rabbits, S. aureus can invade subcutaneous tissues through small dermal lesions (Vancraeynest et al., Reference Vancraeynest, Hermans and Haesebrouck2004). In rabbit flocks, two types of S. aureus infections can be observed: infections limited to a small sub-population caused by weakly virulent strains and a chronic infection affecting the rabbitry caused by highly virulent strains. Highly and weakly virulent isolates of S. aureus were screened for biofilm-associated or MSCRAMMs genes (Vancraeynest et al., Reference Vancraeynest, Hermans and Haesebrouck2004). The distribution of the icaA, icaD and bap genes among highly and weakly virulent isolates was similar. This suggests that the clinical symptoms associated with S. aureus infections in rabbits are not related to their biofilm formation potential.
Staphylococcus intermedius is part of the normal microbiota of dogs and pigeons. S. intermedius is an aetiological agent of skin infections in dogs, especially pyoderma (Futagawa-Saito et al., Reference Futagawa-Saito, Ba-Thein, Sakurai and Fukuyasu2006). A study using a large number of S. intermedius isolates indicated that biofilm formation was significantly higher in canine isolates than in pigeon isolates (Futagawa-Saito et al., Reference Futagawa-Saito, Ba-Thein, Sakurai and Fukuyasu2006). Following the description of a new species, Staphylococcus pseudintermedius (Devriese et al., Reference Devriese, Vancanneyt, Baele, Vaneechoutte, De Graef, Snauwaert, Cleenwerck, Dawyndt, Swings, Decostere and Haesebrouck2005), it appeared that several strains formerly identified as S. intermedius should be reclassified. All canine and some equine isolates previously identified as S. intermedius are now considered to be S. pseudintermedius. S. intermedius strains isolated from domestic pigeons and, in some cases, horses appear to belong to the species Staphylococcus delphini. S. intermedius seems to be confined to strains isolated from feral pigeons.
The MBEC of biofilm cultures of S. aureus isolated from bovine mastitis or Staphylococcus hyicus isolated from porcine dermatitis was higher than the MIC of planktonic cultures for all antimicrobial agents tested (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002); similar observations were made by Melchior et al. (Reference Melchior, Fink-Gremmels and Gaastra2006a). Bacteria growing in biofilms appear to be highly resistant to antimicrobial agents at the maximum concentrations used in vivo. Hence, it can be assumed that biofilm formation by mastitis-associated S. aureus can offer an explanation for the poor correlation between bacteriological cure and susceptibility to antimicrobial agents as determined by CLSI (Clinical and Laboratory Standards Institute) testing methods.
Streptococcus
Streptococcus agalactiae or Group B Streptococcus (GBS) can colonize the mammary glands of ruminants. S. agalactiae is able to survive for long periods in udders, resulting in clinical and sub-clinical mastitis (Rinaudo et al., Reference Rinaudo, Rosini, Galeotti, Berti, Necchi, Reguzzi, Ghezzo, Telford, Grandi and Maione2010). GBS can form biofilms and pili, especially type 2a that play an important role during biofilm formation (Konto-Ghiorghi et al., Reference Konto-Ghiorghi, Mairey, Mallet, Duménil, Caliot, Trieu-Cuot and Dramsi2009; Rinaudo et al., Reference Rinaudo, Rosini, Galeotti, Berti, Necchi, Reguzzi, Ghezzo, Telford, Grandi and Maione2010). Pili have a domain called the von Willebrand adhesion domain that is involved in adhesion to epithelial cells. However, the von Willebrand adhesion domain of pili is not required for biofilm formation. Biofilm cultures of a bovine mastitis isolate of S. agalactiae were not killed by the antimicrobial agents tested, whereas planktonic cultures of the same isolate were (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). On the other hand, the MBEC and the MIC of a bovine mastitis isolate of Streptococcus dysgalactiae were comparable for β-lactams and oxytetracycline (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002).
Streptococcus suis is a major pathogen of pigs; infection by this pathogen can result in pneumonia, meningitis, and septicemia. S. suis is also a zoonotic agent and workers in swine farms and pork-processing plants are at a high risk of infection. Bonifait et al. (Reference Bonifait, Grignon and Grenier2008) have shown that fibrinogen-induced biofilm formation by S. suis in a dose-dependent manner. Futhermore, an unencapsulated mutant of S. suis formed more biofilm than the parental strain suggesting that the capsule masks important adhesins and hydrophobic molecules responsible for biofilm formation (Tanabe et al., Reference Tanabe, Bonifait, Fittipaldi, Grignon, Gottschalk and Grenier2010). Additionally, avirulent strains seemed to produce more biofilms than virulent strains (Wei et al., Reference Wei, Li, Zhang, He, Hua, Xia, Cai, Chen and Jin2009). Biofilm-grown cells were more resistant to penicillin G and ampicillin than were planktonic cells (Bonifait et al., Reference Bonifait, Grignon and Grenier2008; Grenier et al., Reference Grenier, Grignon and Gottschalk2009). However, there was no increased resistance to β-lactams by biofilm cultures of a porcine pericarditis isolate of S. suis (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002). Biofilm formation has also been observed with a bovine rumen isolate of Streptococcus bovis (Olson et al., Reference Olson, Ceri, Morck, Buret and Read2002).
Streptococcus pneumoniae biofilms have been detected in a chinchilla model of otitis. It has been proposed that biofilm formation in vivo is intertwined with the formation of extracellular neutrophil traps (reviewed by Moscoso et al., Reference Moscoso, García and López2009).
Yersinia
Yersinia enterocolitica is a food-borne pathogen inhabiting the tonsils of pigs. It tolerates a wide range of temperature and growth conditions, suggesting that it can survive in soil, water and other environments. Therefore, growth as a biofilm may allow Y. enterocolitica to persist in several environmental niches (Kim et al., Reference Kim, Young and Young2008). Flagella are important for the initiation of biofilm formation but biofilm development occurs differently under static conditions or in the presence of shear force (Kim et al., Reference Kim, Young and Young2008).
Yersinia ruckeri is the etiological agent of enteric redmouth disease, also called yersiniosis. Yersiniosis is an economically important infectious disease affecting the rainbow trout industry (Coquet et al., Reference Coquet, Cosette, Quillet, Petit, Junter and Jouenne2002). The presence of Y. ruckeri biofilms on the surface of fish tanks used in fish farms was a potential source of contamination for recurrent infection (Coquet et al., Reference Coquet, Cosette, Quillet, Petit, Junter and Jouenne2002). Yersiniosis is routinely treated with oxolinic acid and biofilm cells were more resistant to this agent than were their planktonic counterparts.
Y. pestis is the causative agent of bubonic plague. It has been suggested that Y. pestis biofilms induce starvation of fleas by blocking their digestive tract. This starvation stimulates the flea into a feeding frenzy involving repeated biting. This feeding frenzy would thereby facilitate the transmission of Y. pestis to new hosts (Darby, Reference Darby2008). Y. pestis biofilms appear to play an important role during the infection of fleas but biofilms play no role in mammalian pathogenesis (Darby Reference Darby2008; Kim et al., Reference Kim, Young and Young2008; Sun et al., Reference Sun, Koumoutsi and Darby2009). The extracellular matrix of the biofilm contains a homopolymer of PGA (Darby, Reference Darby2008). The extracellular matrix is synthesized by proteins encoded by the hmsHFRS operon and these proteins are orthologues of proteins encoded by the pgaABCD operon of E. coli and the icaABCD operon of S. epidermidis (Darby, Reference Darby2008; Hinnebusch and Erickson, Reference Hinnebusch and Erickson2008). Despite the presence of PGA in its matrix, the Y. pestis biofilm cannot be digested by the PGA-degrading enzyme dispersin B. The expression of the hmsHFRS operon is regulated by polyamines (Wortham et al., Reference Wortham, Oliveira, Fetherston and Perry2010); furthermore, c-di-GMP signaling regulates biofilm formation in Y. pestis. The mechanism involved in c-di-GMP signaling is widespread in bacteria. However, Y. pestis is the only bacterium able to form biofilms in fleas (Darby Reference Darby2008).
Yersinia pseudotuberculosis is a food- and water-borne enteric pathogen, from which Y. pestis is thought to have evolved (Haesebrouck et al., Reference Haesebrouck, Vanrobaeys, de Herdt and Ducatelle1995). Similar to Y. pestis, Y. pseudotuberculosis possesses the hmsHFRS operon. Y. pseudotuberculosis can form biofilms in vitro, but it is unable to do so in fleas (Hinnebusch and Erickson, Reference Hinnebusch and Erickson2008). The response regulator PhoP negatively regulates the formation of biofilm in Y. pseudotuberculosis and Y. pestis (Sun et al., Reference Sun, Koumoutsi and Darby2009). PhoP appears to downregulate the diguanylate cyclase HmsT. Interestingly, a Caenorhabditis elegans model has been developed to study biofilm formation by Y. pestis (Darby, Reference Darby2008).
Biofilms and chronic wounds
It has been known for decades that microbial infections have a deleterious effect on wound healing, and the control of bioburden is considered to be an important aspect of wound management (James et al., Reference James, Swogger, Wolcott, deLancey Pulcini, Secor, Sestrich, Costerton and Stewart2008). Biofilm-associated diseases are typically persistent infections that develop slowly, are rarely resolved by immune defenses, and respond poorly to antimicrobial therapy. Chronic wound infections share the above-mentioned characteristics. Molecular techniques have highlighted the polymicrobial nature of wound infections. In animal diseases, wound infections are particularly problematic (Clutterbuck et al., Reference Clutterbuck, Woods, Knottenbelt, Clegg, Cochrane and Percival2007), for example lower-limb wounds in horses. These wounds pose similar problems to pressure sores and diabetic foot ulcers in humans. Recently, Cochrane et al. (Reference Cochrane, Freeman, Woods, Welsby and Percival2009) were the first to demonstrate the presence of biofilms in chronic wounds of horses. They also demonstrated the importance of combining denaturing gradient gel electrophoresis and PCR with culture techniques to analyze the microbes associated with chronic wounds. An in vitro model to study biofilms associated with chronic wounds was recently developed, this new technique uses a constant depth film fermenter to assess the efficacy of antimicrobial treatments (Hill et al., Reference Hill, Malic, McKee, Rennison, Harding, Williams and Thomas2010).
Biofilms and the food industry
The food industry is considered to be part of the realm of public health area rather than the realm of veterinary medicine. However, it is important to keep in mind the impact of biofilm formation when a farm-to-fork (or gate-to-plate) approach to food safety is used. The significance of biofilms in the food industry is well documented. Biofilm formation by bacteria on food products or food processing equipment contributes to spoilage, and contamination of food and the spread of food-borne pathogens (Wong, Reference Wong1998; Uhlich et al., Reference Uhlich, Rogers and Mosier2010; Van Houdt and Michiels, Reference Van Houdt and Michiels2010). Bacteria in biofilms are able to persist in the food industry environment, because biofilms protect bacteria from heat, desiccation, other environmental stresses and antibacterial agents. This intrinsic resistance creates obstacles for the complete cleaning and disinfection of surfaces that come into contact with food. Milk and milk products can harbor a variety of micro-organisms and have the potential to be important sources of food-borne pathogens (Oliver et al., Reference Oliver, Jayarao and Almeida2005). The presence of food-borne pathogens in milk is due to direct contact with contaminated sources in the dairy farm and their secretion from the udder of an infected animal. Overall, biofilms represent potential reservoirs of food-borne pathogens that are difficult to eradicate.
Compounds affecting bacterial biofilm formation and dispersal
There are several strategies to prevent and inhibit biofilm formation. These strategies include the prevention of microbial attachment, prevention of microbial growth, disruption of cell-to-cell communication, inhibition of matrix synthesis and disintegration of the biofilm matrix (Stewart, Reference Stewart2003; Anderson and O'Toole, Reference Anderson and O'Toole2008; Cegelski et al., Reference Cegelski, Marshall, Eldridge and Hultgren2008). Effective biofilm inhibitors could dramatically change the treatment of many infectious diseases (Cegelski et al., Reference Cegelski, Marshall, Eldridge and Hultgren2008). A basic strategy to discover inhibitors of biofilm formation is the direct screening of chemical compounds during biofilm formation assays. In recent years, the development of target-based screening for anti-biofilm agents has been focused on inhibitors of QS (e.g. halogenated furanones, azitrhomycin and 4-nitro-pyridine-N-oxide), compounds interfering with the metabolism of the signal molecule c-di-GMP (e.g. sulfathiazole) or inhibitors of DNA and nucleotide biosynthesis (Landini et al., Reference Landini, Antoniani, Burgess and Nijland2010). Additionally, signal molecules inhibiting biofilm formation can also stimulate biofilm dispersal (Landini et al., Reference Landini, Antoniani, Burgess and Nijland2010). Since QS has a potential role during bacterial infections of animals, the use of QS inhibitors as an antibacterial agent could provide new tools for veterinary medicine. However, the current research is limited to use of QS inhibitors in aquaculture (Boyen et al., Reference Boyen, Eeckhaut, Van Immerseel, Pasmans, Ducatelle and Haesebrouck2009).
Several examples of molecules capable of interfering with biofilm formation have recently been reported. Davies and Marques (Reference Davies and Marques2009) described a small messenger fatty acid molecule produced by P. aeruginosa, cis-2-decenoic acid, capable of inducing the dispersion of pre-established biofilms and inhibiting biofilm development. This molecule was also capable of inducing dispersal of biofilms formed by Gram-negative and Gram-positive bacteria and yeasts. Therefore, cis-2-decenoic acid may function in different kingdoms. A derivative of the marine natural product bromoageliferin called TAGE (trans-bromoageliferin analogue) also had anti-biofilm activity against P. aeruginosa (Huigens III et al., Reference Huigens, Ma, Gambino, Moeller, Basso, Cavanagh, Wozniak and Melander2008). Truchado et al., (Reference Truchado, Gil-Izquierdo, Tomás-Barberán and Allende2009) have observed that chestnut honey and its aqueous extract can act as QS inhibitors. These two compounds also significantly reduce the formation of biofilm by Y. enterocolitica and A. hydrophila. The cathelicidin LL-37 was shown to inhibit F. novicida biofilm formation at sub-inhibitory concentrations (Amer et al., Reference Amer, Bishop and van Hoek2010). The cathelicidin family is a large and diverse collection of cationic antimicrobial peptides found in a variety of vertebrate hosts. They represent an ancient mechanism of the innate immune response used to combat infection. Interestingly, resistance to these antimicrobial peptides is uncommon.
A cross-disciplinary approach combining microbiology and chemoinformatics was recently used to identify new and effective drugs with anti-biofilm activity (Dürig et al., Reference Dürig, Kouskoumvekaki, Vejborg and Klemm2010). Natural compounds from plants inhibiting the formation of biofilms by S. aureus and S. dysgalactiae were identified using this approach. The compounds did not have an effect on planktonic cells at the concentrations needed to inhibit biofilm formation. These plant compounds can be considered drugs that prevent the switch to a biofilm lifestyle. According to the authors, such compounds might be less prone to the development of bacterial resistance than are classic antibiotics.
Bacteriophages can also be used to disperse biofilms, because bacteriophages produce depolymerases and other surface enzymes that degrade bacterial polysaccharides (Anderson and O'Toole, Reference Anderson and O'Toole2008; Richards and Melander, Reference Richards and Melander2009). Unfortunately phage specificity is high and a phage cocktail composed of different types of phages would be necessary to treat a multi-species biofilm.
Vaccination
Vaccination against biofilm-positive pathogens has not been thoroughly evaluated but promising data have been generated. As previously mentioned, PGA is a matrix polysaccharide produced by a variety of bacterial pathogens. Protective antibodies to PGA are elicited when a deacetylated glycoform is used in conjugate vaccines, whereas protective antibodies are not generated when highly acetylated PGA is used (Gening et al., Reference Gening, Maira-Litrán, Kropec, Skurnik, Grout, Tsvetkov, Nifantiev and Pier2010). Chemical synthesis of a series of oligoglucosamine ligands with specific differences in their N-acetylation allowed for the identification of a formulation for a conjugate vaccine that generated protective immune responses against S. aureus and E. coli (Gening et al., Reference Gening, Maira-Litrán, Kropec, Skurnik, Grout, Tsvetkov, Nifantiev and Pier2010). This potential vaccine could be used to generate protective immunity against PGA-producing pathogens. However, the production cost associated with this potential vaccine might be prohibitive for its use in veterinary medicine.
A vaccine for sheep mastitis composed of S. aureus bacterins, crude bacterial extracts or purified PGA from biofilm-cultured bacteria was evaluated (Pérez et al., Reference Pérez, Prenafeta, Valle, Penadés, Rota, Solano, Marco, Grilló, Lasa, Irache, Maira-Litrán, Jiménez-Barbero, Costa, Pier, de Andrés and Amorena2009). Bacterins from strong biofilm-producing bacteria triggered the highest production of antibodies to PGA and were more protective than the vaccine containing the bacterins from weak biofilm-producing bacteria in an intra-mammary challenge. The production of protective immunity was independent of the adjuvant or the S. aureus capsular type used in the challenge. It is suggested that PGA-specific IgG antibodies opsonized bacteria and favored phagocytosis. Thus, bacterins from bacteria producing strong biofilms could be a cost-effective vaccine against ruminant mastitis caused by S. aureus.
Finally, analysis of antigens expressed by a biofilm-culture of A. hydrophila revealed that 15 proteins were repressed and three new proteins were present when compared to a planktonic culture (Asha et al., Reference Asha, Nayak, Shankar and Mohan2004). Interestingly, biofilm cells did not express the S-layer proteins and produced an additional high molecular weight LPS. The above-mentioned changes are probably key factors in the efficacy of an oral vaccine based on a biofilm-culture of A. hydrophila in eliciting a protective immune response in fish.
Conclusion and future challenges
Biofilm formation may not always be a virulence factor, given that many non-pathogenic bacteria produce biofilms (Hall-Stoodley and Stoodley, Reference Hall-Stoodley and Stoodley2005; Hancock et al., Reference Hancock, Dahl and Klemm2010). However, biofilm formation by certain pathogens appears to facilitate their survival in the environment and the host. Biofilm research is therefore an area of intense interest (Haussler and Parsek, Reference Haussler and Parsek2010) and biofilm research has recently gained recognition in areas such as animal health and public health. Reseachers now have access to a wide arsenal of techniques including three-dimensional imaging, specific fluorescent stains and molecular-reporter technology to study biofilms (Costerton et al., Reference Costerton, Stewart and Greenberg1999; Hall-Stoodley et al., Reference Hall-Stoodley, Costerton and Stoodley2004). Furthermore, new techniques to study biofilm are being developed to enhance research on specific bacterial sub-populations found in the biofilm. For example, it is now possible to use laser capture microdissection to isolate subsets of bacterial cells from defined locations in a biofilm and study gene expression in the selected sub-population (Lenz et al., Reference Lenz, Williamson, Pitts, Stewart and Franklin2008).
New tools are required for the prevention, treatment and diagnosis of pathogens that form biofilms during the infection process, because biofilms have unique properties that are absent in planktonic cells (Murphy et al., Reference Murphy, Bakaletz and Smeesters2009). As we develop the next generation of antimicrobial compounds, consideration should be given to the synergies between antibiotics, and other molecules (e.g. biocides, metals, enzymes, surfactants or QS inhibitors) for the treatment of biofilms (Ceri et al., Reference Ceri, Olson and Turner2010). However, before synergies can be measured, new standardized assays have to be developed (Ceri et al., Reference Ceri, Olson and Turner2010). Additionally, the efficacy of biocides against bacteria has to be evaluated for biofilm cultures and cannot be restricted to planktonic cells.
The impact of bacterial biofilm formation in veterinary medicine is obvious. There is a potential for increased resistance to antibiotics, to disinfectants and to the host immune response. The development of such resistance interferes with the treatment of animals and/or effective disinfection of the farm environment. The persistence of antibiotic resistance genes within biofilms is another aspect that should not be neglected, because it has a potential impact on both animal and public health. Furthermore, bacteria rarely form monospecies biofilms and bacteria are also known to attach to pre-existing biofilms. Examples have been documented with L. monocytogenes (Habimana et al., Reference Habimana, Meyrand, Meylheuc, Kulakauskas and Briandet2009), E. coli O157:H7 (Uhlich et al., Reference Uhlich, Rogers and Mosier2010) and P. aeruginosa (Deligianni et al., Reference Deligianni, Pattison, Berrar, Ternan, Haylock, Moore, Elborn and Dooley2010). Therefore, the natural existence of multi-species biofilms adds complexity to the analysis of biofilms. Although studies investigating in vitro biofilm formation have been performed on bacterial pathogens of veterinary importance, very few studies involving the formation of biofilms in vivo have been performed. Further research is required to develop effective strategies to treat and prevent biofilm-associated diseases in animals (Clutterbuck et al., Reference Clutterbuck, Woods, Knottenbelt, Clegg, Cochrane and Percival2007). Further research is also required to develop effective disinfection protocols to eliminate biofilms from the farm and food-processing environments, because biofilms can act as a reservoir for infectious agents.
Acknowledgments
Work in Mario Jacques' laboratory has been supported by a discovery grant (003428) from the Natural Sciences and Engineering Research Council of Canada. The authors would also like to acknowledge the support of the Ministère des relations internationales du Québec (Ve réunion du Comité mixte Québec-Catalogne, projet 05.301-RST-RT), Jenny-Lee Thomassin for proofreading the manuscript, and an anonymous reviewer for taxonomic updates.






