We are very pleased that Dr Rodney Franklin (Fig 1) is the focus of our third in a planned series of interviews in Cardiology in the Young entitled, “Global Leadership in Paediatric and Congenital Cardiac Care.”Reference Tretter and Jacobs1,Reference Tretter and Jacobs2 Dr Franklin was born in London, England, spending the early part of his childhood in the United States of America before coming back to England. He then attended University College London Medical School and University College Hospital in London, England, graduating in 1979. Dr Franklin would then go on to complete his general and neonatal paediatrics training in 1983 at Northwick Park Hospital and University College Hospital in London, England, followed by completing his paediatric cardiology training in 1989 at Great Ormond Street Hospital for Children in London, England. During this training, he additionally would hold the position of British Heart Foundation Junior Research Fellow from 1987 to 1989. Dr Franklin would then complete his training in 1990 as a Senior Registrar and subsequent Consultant in Paediatric and Fetal Cardiology at Wilhelmina Sick Children’s Hospital in Utrecht, the Netherlands. He subsequently obtained his research doctorate at University of London in 1997, consisting of a retrospective audit of 428 infants with functionally univentricular hearts.

Figure 1. Rodney C. G. Franklin, MB BS, MD, FRCP, FRCPCH.
Dr Franklin has spent his entire career as a Consultant Paediatric Cardiologist at the Royal Brompton & Harefield Hospital NHS Foundation Trust, being appointed in 1991. He additionally holds honorary Consultant Paediatric Cardiology positions at Hillingdon Hospital, Northwick Park Hospital, and Lister Hospital in the United Kingdom, and Honorary Senior Lecturer at Imperial College, London. He has been the Clinical Lead of the United Kingdom and Republic of Ireland National Congenital Heart Disease Audit (2013–20), which promotes data collection within specialist paediatric centres. Dr Franklin has been a leading figure in the efforts towards creating international, pan European, and national coding systems within the multidisciplinary field of congenital cardiac care. These initiatives include but are not limited to the development and maintenance of The International Paediatric & Congenital Cardiac Code (IPCCC) and the related International Classification of Diseases 11th Revision (ICD-11) for CHD and related acquired terms and definitions. We had the pleasure to interview Dr Franklin in order to discuss his experience in developing these important coding systems and consensus nomenclature to both improve communication and the outcomes of patients. We additionally discuss his experience in the development and implementation of strategies to assess the quality of paediatric and congenital cardiac care and publicly report outcomes.
Dr Tretter: Tell us about your upbringing, and any role models or events which led both to your pursuit of medicine in general, and specifically to the field of paediatric cardiology.
Dr Franklin: I was born in London. However, my family emigrated when I was 6 months of age to New York, and I spent the first 8 years of my life in New Rochelle, just north of New York City. My mother is American. In fact, both of my grandmothers are also American. My father and both of my grandfathers are British. Each met their spouses on transatlantic crossings. So, there has been an international mix within my family for a long time. I remember very little of my education in New York. We returned to the United Kingdom in 1964 when my father took a job as a journalist for the United Kingdom equivalent of Consumer Reports, called Which? magazine. I was inspired with the concept of medicine by my uncle who was a general practitioner in London, working in a deprived area of the city. He was very hard working and compassionate. I attended Bryanston boarding school in the southwest of the country, and with the decision to pursue a career in medicine made certain to take the appropriate courses. I was fortunate to get into University College London Medical School. Towards the end of my training in 1979, I did a 3-month elective at the Goroka Hospital in the Eastern Highlands Province of Papua New Guinea under their Director, Dr Frank Shann. Professor Shann would later be the Director of the Paediatric ICU at Melbourne Children’s Hospital in Australia. He was a great inspiration to me as a paediatrician. I was put in there as a resident medical officer, looking after children as if I were a junior doctor right away. It was during this experience when I decided I wanted to take care of children. Dr Shann also involved me in research investigating infant pneumonias with direct lung aspirates. This interesting work inspired me regarding the importance of research towards improving care. I would then go on to my general and neonatal paediatrics training at University College Hospital in London, England. It was my interactions with Dr Phil Rees and his visiting paediatric cardiology team from Great Ormond Street Hospital which initially motivated me towards the field of paediatric cardiology. One of my memories from that experience was when we would take our neonates who needed ligation of their patent arterial duct, over to the operating theatres at Great Ormond Street. A call would go out to all the junior doctors and staff once we knew the blood type of the infant that was being taken over, and if your blood type matched, then you would be asked to donate. We would take over our 50 ml of fresh blood from this bank with us in a syringe and they would use this without formal crossmatching if required. This practice does not continue today, but back then this was the best we could offer. I then proceeded to Great Ormond Street Hospital for my junior training in paediatric cardiology.
Dr Tretter: A better part of your career has focused on developing and updating national and international coding systems. Clear communication and mutual understanding are important in any field, especially within medicine. It is obviously important for improved patient care, along with other factors such as appropriate reimbursement. Talk to us specifically about what interested you in pursuing this very important yet seemingly onerous task over the past 25 years. What were the deficiencies in used terminology and coding systems that you saw at the outset of this?
Dr Franklin: During my paediatric cardiology training at Great Ormond Street Hospital, I was inspired by Professor Fergus Macartney, chair of paediatric cardiology, along with the great cardiac morphologists Professors Robert Anderson and Anton Becker. After the completion of my initial junior job at Great Ormond Street Hospital in 1983, there was a gap of 3 months before I could get on to the next stage. To fill this, Professor Macartney employed me for coding of complex CHD using large dot matrix printouts. That was my first introduction to coding and nomenclature, where I became interested in classifications of CHD and ensuring that people were talking about the same entity when looking at outcomes. I realised the huge heterogeneity in CHD, which inspires all of us and holds our interest.
There was no real system of classification in a comprehensive way when I entered the field in the mid-1980s, but instead, many home-grown classification systems. There was already the division of classification in terms of the Van Praaghian (Boston) and Andersonian (London) schools of thought. Professor Anderson used to frequently give lectures at Great Ormond Street Hospital, so I was clearly being “brainwashed,” if you like. Professor Anderson is certainly one of my great mentors and was my supervisor for my medical thesis. One of the great things about Professor Anderson is that he was always willing to look at the evidence at any one time and adapt his own thoughts and systems of understanding towards what was clearly the best evidence at that time.
Dr Tretter: He still does to this day! That is what inspires me about Professor Anderson.
Dr Franklin: Yes, he does, and whilst that may exasperate some, I think this is inspiring. If the evidence changes our understanding, then we should be willing to change and adapt.
Whilst at Great Ormond Street Hospital, I started my medical thesis with Professor Anderson as my supervisor, from 1987 to 1997. I assessed the natural and surgically modified outcomes of infants with double-inlet ventricle and tricuspid atresia,Reference Franklin, Spiegelhalter and Anderson3 determined risk factors for mortality and unsuitability for definitive surgery,Reference Franklin, Spiegelhalter and Rossi Filho4,Reference Franklin, Spiegelhalter and Sullivan5 and established a better understanding for the role of palliation in these patients.Reference Franklin, Sullivan, Anderson, Shinebourne and Deanfield6,Reference Franklin, Spiegelhalter and Anderson7 This experience solidified the importance of the sequential segmental approach towards classification of CHD. I could see that this would be the system on which everything else would be based. By classifying CHD with this system, it would simplify understanding and would influence the way children were treated. With the help of both Professor Anderson and Professor Macartney, along with the statistical expertise of Professor David Spiegelhalter, who was later knighted and is now Professor Sir David Spiegelhalter, we were able to create a system where you could dial in the specific morphology of a patient with either double-inlet ventricle or tricuspid atresia and predict the outcomes. These experiences surrounding my medical thesis impressed upon me the importance and clinical relevance of accurate coding.
Having left Great Ormond Street, I went to Utrecht in the Netherlands in 1989. They had adopted a system of coding and nomenclature in a national database that they used for day-to-day clinical encounters in their paediatric cardiac patients. The system originated from a textbook produced by the Royal Brompton (Fig 2) published in 1985 with a list of 600 congenital heart diagnoses, each with a six-digit code. In Holland, the system was expanded by Drs André Moulaert, and Eric Harinck to 1700 codes, including surgical codes but no post-procedural complications, and little electrophysiology. Knowing my background, they asked me to expand this coding system. I increased this to a total of 4500 codes over the next few years to produce a more comprehensive, in-depth system using the same six-digit codes as a backbone, to additionally include transcatheter and surgeries, complications, electrophysiology, and co-morbidities. In the United Kingdom, these codes were then incorporated into the trans-medical coding system used by general practitioners (Read codes) in the mid-1990s, which later was amalgamated with the American College of Pathologist’s clinical lexicon, the Systematized Nomenclature of Medicine Reference Terminology, to produce SNOMED Clinical Terms (SNOMED CT) in 2002 for use in electronic health records.
Dr Tretter: What were some of the barriers faced when trying to implement these coding and nomenclature systems?
Dr Franklin: There was not that much resistance towards using the nomenclature system we were promoting because Europe in general tended to use the Andersonian approach. So, in a way we were speaking to the converted. It was, however, when becoming more international, that brought the difficulties related to different names being used for the same lesion. This formed the basis for the mission of The International Society for Nomenclature of Paediatric and Congenital Heart Disease (ISNPCHD) , to create a global system allowing synonyms for the same lesion, unified using a single numerical code.

Figure 2. (A) The Diagnosis of Congenital Heart Disease textbook and (B) an example of its 6-digit code classification system.
Another early more practical barrier was the lack of adequate digital resources in healthcare systems. Data were collected on paper and people were not interested in spending time coding without being able to see the usefulness of it. While I was still in Utrecht, I was working with a software engineer Ron Brower who created a successful user-friendly software system at the beginning of the computer era which made it easier for people to enter data. Such systems are of course now widespread.
Dr Tretter: Please explain to our readership The International Paediatric & Congenital Cardiac Code (IPCCC), a coding system, which you played a key role in developing. What is IPCCC, what did it take to develop IPCCC, and what do you see as the main importance of IPCCC?
Dr Franklin: I think it is important to understand the intervening steps first. The Association for European Paediatric and Congenital Cardiology (AEPC) was looking for a European coding system. In 1998, they adopted the entire 6-digit code system, which had been produced by myself and the Dutch, to become the European Paediatric Cardiac Code (EPCC), published in 1999 and 2000.Reference Franklin, Anderson and Daniëls8,Reference Franklin9 In 2000, a separate system was published by the European Association for Cardio-Thoracic Surgery (EACTS) and Society of Thoracic Surgeons (STS), which was more surgically based, with a more mixed terminology system.Reference Mavroudis and Jacobs10,Reference Mavroudis and Jacobs11 On Friday, 6 October, 2000 in Frankfurt, Germany, at the meeting of the European Congenital Heart Surgeons Foundation, prior to the 14th Annual Meeting of EACTS, it was decided to put these two coding systems together into one universal system. (European Congenital Heart Surgeons Foundation [ECHSF] is the former name of European Congenital Heart Surgeons Association [ECHSA].) This collaboration led to The First International Summit on Nomenclature for Congenital Heart Disease held at The Third World Congress of Pediatric Cardiology and Cardiac Surgery, Toronto, Canada, 27 May, 2001 (Figs 3 and 4) and the eventual formation of The International Society for Nomenclature of Paediatric and Congenital Heart Disease (ISNPCHD).

Figure 3. The faculty of The First International Summit on Nomenclature for Congenital Heart Disease at The Third World Congress of Pediatric Cardiology and Cardiac Surgery, Toronto, Canada, 27 May, 2001. Photo taken at The First International Summit on Nomenclature for Congenital Heart Disease at The Third World Congress of Pediatric Cardiology and Cardiac Surgery, Toronto, Canada, 27 May, 2001. Pictured from left to right are: Marie J. Béland, The Montreal Children’s Hospital, Montreal, Canada; Steven Colan, Boston Children’s Hospital, Harvard University, Boston, Massachusetts, United States of America; Francois G. Lacour-Gayet, L’hôpital Marie Lannelongue, Paris, France; Constantine Mavroudis, Peyton Manning Children’s Hospital, Indianapolis, Indiana, United States of America; Robert H. Anderson, Great Ormond Street Hospital for Children, London, United Kingdom; Richard Van Praagh, Boston Children’s Hospital, Harvard University, Boston, Massachusetts, United States of America; Christo I. Tchervenkov, The Montreal Children’s Hospital, Montreal, Canada; Bohdan J. Maruszewski, Children’s Memorial Health Institute, Warsaw, Poland; Jeffrey P. Jacobs, University of Florida, Gainesville, Florida, United States of America; Franco P Stocker, University Hospital, Berne, Switzerland; Rodney C. G. Franklin, Royal Brompton & Harefield Hospital NHS Foundation Trust, London, United Kingdom; Martin J. Elliott, Great Ormond Street Hospital for Children, London, United Kingdom. Franco P Stocker was the First Chair of the Coding Committee of The Association for European Paediatric and Congenital Cardiology (AEPC). Constantine Mavroudis was Chair of The International Congenital Heart Surgery Nomenclature and Database Project of The Society of Thoracic Surgeons (STS) in North America, The European Association for Cardio-Thoracic Surgery (EACTS), and the European Congenital Heart Defects Database of The European Congenital Heart Surgeons Foundation (ECHSF) – (subsequently renamed The European Congenital Heart Surgeons Association [ECHSA] in 2003).

Figure 4. Professor Robert Anderson and Dr Richard Van Praagh agreeing to work together with the future ISNPCHD towards a consensus classification for CHD. Photo taken at The First International Summit on Nomenclature for Congenital Heart Disease at The Third World Congress of Pediatric Cardiology and Cardiac Surgery, Toronto, Canada, 27 May, 2001.
In 2002, we then published a mapped short list, which had a mapping of the short list of the EACTS-STS Congenital Heart Surgery Nomenclature and Database Project and the short list of the EPCC, using the six-digit coding system. Reference Franklin, Jacobs, Tchervenkov and Béland12 This produced the joint system, IPCCC. The IPCCC would then serve as a universal, comprehensive coding system for communication and database usage between these two international coding systems. Reference Franklin, Jacobs and Krogmann13 The mapping process, and making it fully comprehensive, was the initial collaborative work of the group of 12 who initiated The International Working Group for Mapping and Coding of Nomenclature for Paediatric and Congenital Heart Disease (later known as The Nomenclature Working Group or NWG), supported by Martin Elliott and initially led by Christo Tchervenkov (Table 1). Reference Béland, Franklin and Jacobs14 This initiated our annual or twice yearly meetings which have continued for the past 20 years. The NWG became the first committee of ISNPCHD .
Dr Tretter: You are the past president of the ISNPCHD, with Jeff Jacobs being the current president (Table 2). I have had the pleasure to be a member of this society over the past few years and get insight into the long road to developing an expert consensus for the nomenclature of paediatric and congenital cardiac disease and related acquired terms and definitions, based on IPCCC hierarchical structure, which will serve to form the foundation and backbone of The IPCCC ICD-11 Congenital Heart Atlas hosted on the Heart University website [www.heartuniversity.org]. Reference Tretter, Windram and Faulkner15 For those not familiar, please discuss what is the ISNPCHD, its history, and its goals.
Dr Franklin: The ISNPCHD was constituted in January, 2005 with the overall mission of unifying the nomenclature used in paediatric cardiac care under a single terminology [www.ipccc.net]. The reason to develop a formal society was largely related to the interactions with the AEPC. The AEPC had funded the publication of the two editions of the European Paediatric Cardiac Code (EPCC). This understandably led to the need for formal discussions and negotiations related to ownership of the coding system. At this point, The International Working Group for Mapping and Coding of Nomenclature for Paediatric and Congenital Heart Disease was just a group of 12 well-meaning and like-minded experts in the field. We therefore realised we needed to become a formal society and so created the ISNPCHD. We then formally negotiated with the AEPC, and all agreed that there should be free access for all to the coding system. We recognised that if there were barriers to people using the system, financial ones in particular, it just wouldn’t get adopted. So, that was the essence of our society, the ISNPCHD, which became the entity which owns IPCCC and governs IPCCC for usage. If people want to use IPCCC, they can access and download it free of charge. However, if a commercial entity wants to include it in their software, they would simply need to sign a copyright form, which states that they would not knowingly sell it on for its own value within their system.
Table 1. Initial Membership of the International Working Group for Mapping and Coding of Nomenclature for Paediatric and Congenital Heart Disease (also known as the Nomenclature Working Group or NWG), which was the first committee of The International Society for Nomenclature of Paediatric and Congenital Heart Disease (ISNPCHD).
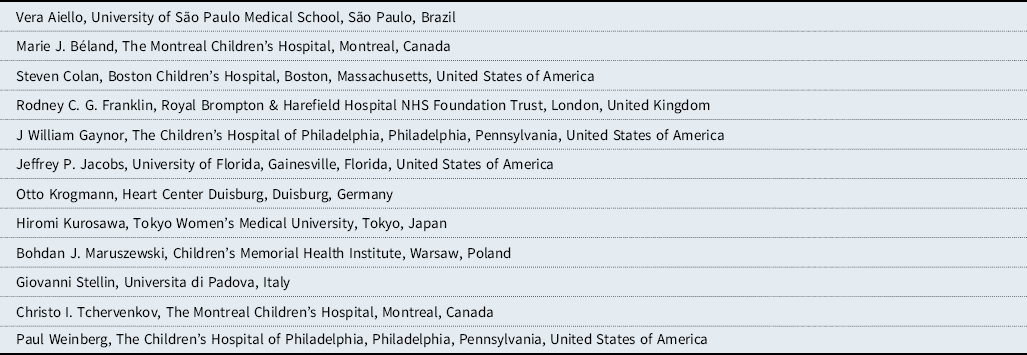
Table 2. Presidents of The International Society for Nomenclature of Paediatric and Congenital Heart Disease (ISNPCHD).

Next, we realised that IPCCC had no definitions for individual lesions. To address this deficiency, during our meeting in Tokyo in 2007, we created two new working groups within the ISNPCHD, in addition to the already existing NWG. The NWG had been there from the start and is the main group responsible for creating IPCCC and maintaining its comprehensive nature. The Definitions Working Group was created in 2007 to define all the 10,000 terms in the Long Lists of IPCCC and the 1000 terms in the Short Lists of IPCCC. The third group is the Archive Working Group, which is the backbone of The IPCCC ICD-11 Congenital Heart Atlas that we are creating with Heart University. The IPCCC ICD-11 Congenital Heart Atlas aims to define and illustrate all the terms in the Short List of IPCCC.Reference Giroud, Jacobs and Spicer16
In 2007, during our meeting in Tokyo, we additionally had a presentation by the World Health Organization (WHO) by the gastroenterologist Professor Kentaro Sugano about the development of ICD-11. They were impressed by our work and felt that we should help develop the CHD part of ICD-11, and to which we all readily agreed. We then did not hear from WHO again until 2009, when I was approached by the WHO to be co-chair of the Internal Medicine Topic Advisory Group with Professor Sugano, for ICD-11 development. This group included a series of subgroups including the Cardiovascular Working Group, within which was CHD. I also became co-chair of the Cardiovascular Working Group within the ICD-11 Topic Advisory Group, alongside Professor Bernard Gersh from the Mayo Clinic. The ISNPCHD then re-engaged with the WHO, and focused our meetings from 2010 onwards towards ICD-11 and creating a much more comprehensive and clinically meaningful classification for CHD within ICD-11.Reference Franklin, Béland and Colan17 The difference between ICD-11 with its previous iterations was that the prior versions were created by statisticians and those interested in classification, but without any clinical involvement. There was “decibel diplomacy,” whereby whoever shouted the loudest had their classification proposals adopted! A revelation occurred within the WHO when it was recognised that it was important and necessary to involve clinicians for future iterations to be adopted within clinical practice. The WHO organised Topic Advisory Groups of a few people, a dozen or so in each specialty, who would use societal input to create a system that would be much more comprehensive and clinically relevant than prior iterations. Jeff Jacobs was also appointed by the WHO to be a member of the Cardiovascular Working Group.
After 8 years of work, ISNPCHD was able to finish our CHD classification for ICD-11, with over 300 diagnostic codes, all with definitions. This IPCCC ICD-11 was an increase from the 26 codes used in ICD-9 and 74 codes used in ICD-10 for CHD, which were largely unhelpful for trying to delve down to different outcomes for various forms of CHD.
These initiatives all involved working with the ISNPCHD team of international leaders over the last 20 years, and particularly closely with Marie Béland and Jeff Jacobs, for the very detailed IPCCC work in the first decade. Without both, we would not have succeeded to where we are now. It has also been a huge privilege and truly inspiring to work with other senior members of the ISNPCHD team over the last two decades, especially Bob Anderson, Paul Weinberg, Steve Colan, Vera Aiello, Otto Krogmann, Hal Walters, Hiromi Kurosawa, Bohdan Maruszewski, Bill Gaynor, Giovanni Stellin, Christo Tchervenkov, Jorge Giroud, and Marshall Jacobs, as well as newer members Lucile Houyel, Leo Lopez, Frédérique Bailliard, Steve Seslar, Marina Hughes, Meryl Cohen, Jim St Louis, Jeff Boris, Amy Juraszek, Allen Everett, Kris Guleserian, Shubhi Srivastsava, and obviously you (Justin Tretter). All of whom, along with their families, I am proud to call my friends.
Dr Tretter: In this effort, you have been a key mediator towards helping draw consensus from two general approaches towards the terminology of CHD, namely the Andersonian and Van Praaghian approaches. The community of paediatric and congenital cardiac care is well aware of some of the competing views on congenital cardiac anatomy. Discuss for our readers some of the challenges in this effort.
Dr Franklin: The first challenge dates back to the early years of IPCCC, when we presented our plan to unite the two main coding systems at The Third World Congress of Pediatric Cardiology and Cardiac Surgery in Toronto in 2001. On 27 May, 2001, there was a well-attended meeting of those interested in this work, with a classic picture of Professor Anderson and Dr Richard Van Praagh burying the hatchet if you will (Fig 4). Not in each other’s back(!), but instead with a handshake as a statement to say this is something they both wanted to do. From that point onwards, there was buy-in from both sides, with representation from both sides in the original 12 involved in the Nomenclature Working Group . We tried to have an understanding that there was a single phenotype that was amenable to be termed or classified in two different ways. Given that the two approaches were scientifically accurate, then it did not matter which approach one chose, as they could be crossmatched and united into a single system. As you are aware, some areas are easier to classify. Meanwhile other areas, even some with seemingly less complex anatomy, such as ventricular septal defects, required hundreds of hours of discussion during our meetings to agree a consensus, for a unified approach. Reference Lopez, Houyel and Colan18 The final published consensus on the classification of ventricular septal defects, which emphasised the importance of both the borders of the ventricular septal defect and the geographic location where the ventricular septal defect opened into the right ventricle, was a perfect example of how our group has worked, accommodating both systems to create a clinically meaningful terminology. Our goal has been for both systems to work side by side in a unified approach. Reference Franklin, Béland and Colan17,Reference Lopez, Houyel and Colan18,Reference Jacobs, Franklin and Jacobs19,Reference Tchervenkov, Jacobs and Weinberg20,Reference Jacobs, Anderson and Weinberg21,Reference Jacobs, Franklin and Wilkinson22
Dr Tretter: During these meetings, I have certainly witnessed the mutual respect between the leaders in our field, despite some of the differing views. What has been your perspective on this?
Dr Franklin: I think what has been inspiring is how the leaders in our field have been able to work together and not be antagonistic. Even if it would take hours and hours to reach an accommodation, there was a willingness to engage in the process. We often would need to bring in third parties of wisdom to bring additional expertise. For example, when we were dealing with electrophysiology and the arrhythmia classification in 2006, we brought in Barbara Deal with Gus Mavroudis from the United States of America and Nico Blom from the Netherlands. We would always seek out leading figures in any given field to make sure that we were getting it right. Because at the end of the day, if the leaders do not buy into the nomenclature, the classification system will not get adopted.
Dr Tretter: How will The IPCCC ICD-11 Congenital Heart Atlas benefit the community of paediatric and congenital cardiac care, and when do you anticipate its completion and availability?
Dr Franklin: The name flips off the tongue so easily! The IPCCC in and of itself has been the backbone of multiple comprehensive databases in congenital cardiac care across the globe for 20 years now, with over a million patients registered into databases and registries using this system, either in its European form or more commonly in the ECHSA and STS Congenital Heart Surgery Databases. The IPCCC and these databases have led to quality improvement by reporting multiple outcomes in children with various forms of CHD. This utilisation and quality improvement have been the greatest achievement of IPCCC. In the United Kingdom, we have had separate research based on IPCCC coding and National Congenital Heart Disease Audit outcomes. The proudest part of this research is that a team from the Clinical Operational Research Unit (University of London) led by Professor Martin Utley and now Professor Christina Pagel, including amongst others Drs Kate Brown, Sonja Crowe and myself, produced the PRAiS (Partial Risk Adjustment in Surgery) risk model. This risk model allows in-house software to monitor the outcomes of a paediatric cardiac surgical programme, based on the centre’s own individual case mix, on a monthly basis, and react appropriately to any negative changes. Reference Brown, Rogers and Barron23,Reference Rogers, Brown and Franklin24
One of the other important aspects of IPCCC is in education and understanding CHD. The numbers and terms may be beautiful for those working with it for decades or those with an in-depth knowledge of CHD, but having an atlas with lesions and phenotypes illustrated represents a huge step forward towards aiding the understanding of CHD and its complexity for future generations to come. The IPCCC ICD-11 Congenital Heart Atlas is an ongoing process which has only just begun. We had started prior to our partnership with Heart University in creating an atlas of morphological images. What has been missing is the other related cardiac imaging modalities to illustrate the lesions such as echocardiography, angiography, computerised axial tomography, and MRI, as well as intraoperative photographs or videos. We have now begun the process to use the over 300 IPCCC ICD-11 terms as the backbone of The IPCCC ICD-11 Congenital Heart Atlas. Each individual lesion will be populated with the associated terms and definitions, as well as links to the associated morphological and cardiac imaging, in order to fully illustrate each lesion in ways that are frequently encountered by the providers of congenital cardiac care. The original aim was to have The IPCCC ICD-11 Congenital Heart Atlas completed by the previously scheduled 2021 Eighth World Congress of Pediatric Cardiology and Cardiac Surgery . Even though the Eighth World Congress has been postponed to 2023 due to the coronavirus disease 2019 (COVID-19) pandemic, we still are aiming to stick to the 2021 goal.
Dr Tretter: What are some of the other coding systems you have been involved in and how do they relate?
Dr Franklin: The International Classification of Diseases, produced by WHO, had an associated interventional classification, which they last published with the ninth revision, ICD-9, in 1978: The International Classification of Procedures in Medicine. For reasons that are unclear, they did not produce a further classification of procedures that are used to treat various problems across medical specialties. Therefore, many countries who had the ability created their own systems for interventional classifications, many using the ICD-9 procedural classification as its backbone. The ICD-11 team realised the importance of this classification of interventional procedures and started to develop the International Classification of Health Interventions (ICHI). ICHI has a very broad scope and is something to be admired, as it not only involves surgical and catheter-based interventions, but also nursing, public health, and psychological interventions, to name a few. Unfortunately for us, ICHI uses a very complex coding system, which involves a three-tiered approach: a target (which is the anatomy), the action (which is the actual procedure undertaken), and the means (which is the approach). When I heard that this was being developed, I shouldered my way into being involved, since the classification of procedures is extremely important to the community of paediatric and congenital cardiac care, and we had already developed a classification system for this in our field. Reference Bergersen, Everett and Giroud25,Reference Bergersen, Giroud and Jacobs26,Reference Brown, Pagel and Brimmell27 We then spent the next 3 years trying to adapt our Short List of over 300 interventions into ICHI, including surgical operations, catheter interventions, electrophysiology procedures, and various imaging procedures. One of the main challenges has been to fit our numerous congenital lesions, such as an intervention on truncal valvar stenosis, into the more widely understood and accepted acquired cardiac lesions, such as an intervention on acquired aortic valvar stenosis. ICHI will hopefully be finalised and published soon. We are also working with SNOMED CT to clean up and create a subset of congenital cardiac terms to match our system within ICD-11.
Dr Tretter: In the United Kingdom, you have been a leader in the development and implementation of strategies to both assess and publicly report the quality of paediatric and congenital cardiac care, and especially paediatric and congenital cardiac surgery. Can you comment on the importance of these initiatives, and can you describe how these initiatives relate to your research related to nomenclature and coding?
Dr Franklin: Most are familiar with the historical problems that we had in Bristol in the United Kingdom in the late 1980s and early 1990s, which related to the quality of surgery in Bristol compared to other centres in the country. Specifically, outcomes were significantly worse following atrioventricular septal defect repairs and the arterial switch operation. It took a whistle blower to reveal the poor outcomes in Bristol, and to illuminate that although the outcomes data were available for quite some time, the appropriate action to address this problem was not undertaken. The problems in Bristol led to the creation of a national database in the United Kingdom in 2000, then called The Central Cardiac Audit Database, with CHD as one component of this database. Reference Brown, Crowe and Pagel28 This database is now the National Congenital Heart Disease Audit, one of six cardiovascular audits within the National Institute for Cardiovascular Outcomes Research. We started to collect data across the United Kingdom and the Republic of Ireland (from 2009) for surgery, interventions, and electrophysiological procedures, including information about both morbidity and mortality. We have published these data, Reference Brown, Crowe and Franklin29,Reference Crowe, Ridout and Knowles30,Reference Rogers, Pagel and Sullivan31 including centre-specific transparent outcomes, since 2007 on our website https://www.nicor.org.uk/national-cardiac-audit-programme/congenital-heart-disease-in-children-and-adults-congenital-audit/. We are now publishing data related to 83 specific procedures, as well as whole centre paediatric surgical performance using PRAiS2 methodology, Reference Rogers, Brown and Franklin24 looking for outliers. Outliers greater than three standard deviations away from other centres will prompt the outlying centre to have a review of their data and current practice in order to understand why their outcomes are discrepant from other centres. More recently, we have been publishing data on post-procedural complications. An additional component of the audit is documenting the success rate of antenatal diagnosis of severe CHD requiring an intervention during infancy, at the mandatory 18 to 20-week fetal ultrasound screening scans performed by obstetric sonographers. The success rate of diagnosing such severe CHD antenatally has shown a huge improvement, because it has enabled the targeting of regions of the United Kingdom with poor rates, leading to enhanced local training and purchase of superior sonographic equipment. It has led to an increased rate of accurate diagnosis in all comers, as well certain specific lesions requiring early surgery, such as hypoplastic left heart syndrome and transposition of the great arteries with intact ventricular septum. Antenatal diagnosis is known to positively influence the outcomes of such patients. Reference Gardiner, Kovacevic and van der Heijden32 I have been involved in this initiative for the past 20 years, clinical lead for the last 7 years, and now moving to a more supportive role.
In the United Kingdom, we think public reporting data is extremely important; however, we do not think that these data should be broken down by specific surgeons. The surgeon is not the only critical component of the treatment of CHD. Surgeons clearly play a crucial role, but it is a complete team that is involved in treating children and adults with CHD. So, we have focused on publishing outcomes stratified by centre. And our agenda has shifted from quality assessment so important for public confidence in our service in the first decade, to enabling quality improvement initiatives going forwards.
Dr Tretter: Finally, can you comment on the differences between the assessment of quality of paediatric and congenital cardiac surgery and the assessment of quality of the non-surgical components of paediatric and congenital cardiac care, both interventional cardiology and non-interventional care?
Dr Franklin: We have historically focused on interventional procedures and outcomes following interventions, including 30-day mortality. We also have data on fluoroscopy times knowing that radiation is a long-term risk to the health of our children. So, we are now in the middle of analysing these data documenting fluoroscopy screening times for the same procedure undertaken by different centres across the United Kingdom. We know that there are clear differences between centres. Some of these differences are related to the type of equipment they have and some are related to procedural strategies. We are trying to understand what other variables may be impacting these differences, whether it is something specific to the diagnostic differences between patients, or, something that is operator-specific.
We would also like to be publishing outcomes stratified by diagnosis, and not be limited just to post-procedural events. We have ambitions to start collecting data stratified by diagnosis from the start of antenatal care with a database created and ready to go, pending finalising the software.
Dr Tretter: Tell us something about your interests and hobbies outside of medicine. If you are not busy with taking care of patients or in the various coding and nomenclature committees and societies, where would we find you?
Dr Franklin: You will find me with my family, often in our family home in Donegal, Ireland. One of the benefits of the nomenclature work has been that at all of our meetings, which have included over 20 meetings in approximately 15 different countries, the members usually bring their families, with many of our grown children remaining in contact with each other around the world. My wife, son and two daughters have often enjoyed a family holiday after the scheduled nomenclature meetings, wherever we may be. Our love of travel has been enhanced by these opportunities. Otherwise, you will find me on a mountain on skis. I have been ski mountaineering since I was eighteen years old and raced competitively as a teenager. I have enjoyed mountain expeditions in Europe, North America, the Artic, and Himalayas, with grant funded exploratory trips to Baffin Island, Kedar Dome, India, and Rolwaling Valley, Nepal. We ski as family at least annually. Closer to home, my wife Michele and I also really enjoy theatre and world music.
Dr Tretter: Well, thank you Dr Franklin. Even being a recent member of ISNPCHD, I had no idea the historical context and hard work underlying what we are creating with The IPCCC ICD-11 Congenital Heart Atlas. The Editorial TEAM of Cardiology in the Young are beyond thankful that you have joined us for our third in a planned series of interviews in Cardiology in the Young entitled, “Global Leadership in Paediatric and Congenital Cardiac Care.” Reference Tretter and Jacobs1,Reference Tretter and Jacobs2
Dr Franklin: It has been a privilege and a pleasure. Thank you for the opportunity.
Financial support
This work received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.









