Introduction
Staphylococcus aureus is an important pathogen which causes serious community and hospital infections. The prevalence of infection and colonisation with methicillin-resistant S aureus (MRSA) is increasing in all infections,Reference Sakoulas and Moellering1 including those of the head and neck.Reference Naseri, Jerris and Sobol2 Between 2001 and 2006, the rate of paediatric S aureus head and neck infections increased by 16.3 per cent in the USA.Reference Naseri, Jerris and Sobol2 Within head and neck infections, the highest rate of MRSA infection occurs in otological infections (34 per cent), followed by sinusal (28.3 per cent) and oropharynx and neck infections (14.2 per cent). In the USA, MRSA infection rates have been highest in the North East Central region. Overall in the USA, MRSA comprised 21.6 per cent of all isolates; corresponding percentages for the years 2001 to 2006 were 11.8, 12.5, 18.1, 27.2, 25.5 and 28.1 per cent, respectively.
This review summarises the studies published over the past two decades which illustrate the growing prevalence of MRSA. It also summarises current therapeutic approaches to MRSA head and neck infections, which may include sinusitis, otitis, periorbital cellulitis, cervical lymphadenitis, tonsillitis, thyroiditis, retropharyngeal abscess, and neck abscesses and wounds.
Specific head and neck infections
The percentage recovery of MRSA from head and neck infections (compared with all S aureus isolates) has been determined by various longitudinal studies, as shown in Table I.
Table I MRSA in head and neck infections: results from longitudinal studies
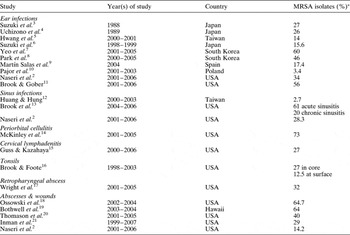
*Of all Staphylococcus aureus isolates. MRSA = methicillin-resistant Staphylococcus aureus
Ear infections
Three Japanese studies performed in the late 1980s and early 1990s assessed the presence of MRSA in ear (amongst other head and neck) infections.Reference Suzuki, Baba, Soyano and Kinoshita3, Reference Uchizono, Ohyama, Nishi, Yoshinaga, Miyata and Miyanohara4, Reference Sugita22
Suzuki et al. Reference Suzuki, Baba, Soyano and Kinoshita3 found the rate of MRSA recovered from new infections to be 27 per cent in middle-ear exudates, 14.3 per cent in nasal discharge, and none in tonsillitis cases.
In 1989, Uchizono et al. Reference Uchizono, Ohyama, Nishi, Yoshinaga, Miyata and Miyanohara4 recovered 231 (52 per cent) MRSA hospital isolates (104 strains) among 448 S aureus isolates; 58 strains (55.8 per cent) were coagulase type II and 35 (33.7 per cent) coagulase type VII. Less MRSA was found in the medical department and out-patients clinics. However, MRSA made up only 15.4 per cent of S aureus isolates recovered from the otolaryngology department, and 26 per cent of S aureus isolates from chronic otitis media. Methicillin-resistant S aureus infected two patients following administration of multiple antibiotics; isolates from these patients produced type II coagulase and resisted multiple antibiotics.
SugitaReference Sugita22 recovered MRSA in one hospitalised and 14 out-patient individuals. Of these isolates, five were from tonsillitis cases, four from patients with cancer and two from chronic otitis media cases.
Since 2000, more reports of MRSA ear infections have appeared.
In the USA in 1999, Santos et al. Reference Santos, Mankarious and Eavey23 described three children with purulent otorrhoea caused by community-acquired MRSA. All required intravenous antibiotics therapy.
In Taiwan, Hwang et al. Reference Hwang, Chu and Liu5 noted that S aureus, including MRSA, had become more common than Pseudomonas aeruginosa in acute otitis externa, granular myringitis and chronic otitis media. They studied 161 patients with otorrhoea and recovered 177 isolates: 77 (43.5 per cent) of S aureus and 29 (18 per cent) of pseudomonas species. The prevalence of community-acquired MRSA infections in discharging ears was 14 per cent (22/161), and these isolates were susceptible to vancomycin, teicoplanin, fusidic acid and minocycline.
In Japan, Suzuki et al. Reference Suzuki, Nishimura and Baba6 reported a nationwide study of otitis media (reporting 466 patients with acute and 476 with chronic otitis media), sinusitis (447 acute and 426 chronic patients), acute tonsillitis (724 patients) and peritonsillar abscess (141 patients). Methicillin-resistant S aureus comprised 15.6 per cent of the 786 S aureus isolates. It was frequently detected in patients with otitis media, although uncommon in cases of tonsillitis and peritonsillar abscess, and was more common in patients previously treated with antibiotics. Vancomycin showed the highest antibiotic activity against the MRSA strains isolated.
In South Korea, Yeo et al. Reference Yeo, Park, Hong, Cha and Kim7 studied 1102 patients with chronic otitis media. The main isolates were pseudomonas species (32 per cent of all isolates) and MRSA (24 per cent). Methicillin-resistant S aureus accounted for 60 per cent (224 of 376) of S aureus isolates.
Also in South Korea, Kim et al. Reference Kim, Song, Lee, Choe, Park and Cho24 in 2005 recovered 3251 S aureus isolates, 1900 (58 per cent) of which were MRSA. Community-acquired infection accounted for 112 (5.9 per cent) of these MRSA infections; of these, 27 were pathogens and 33 colonisers. Most community-acquired MRSA patients had skin, soft tissue or acute ear infections. A new strain of community-acquired MRSA, ST72-SCCmec type IVa without the Panton-Valentine leucocidin gene, was the commonest type identified.
Again in the USA, Laurens et al. Reference Laurens, Becker, Johnson, Wolf and Kotloff25 described an aggressive MRSA ear infection in a 10-year-old child. Despite antimicrobials, intracranial extension developed, as well as osteomyelitis, sphenoid sinusitis, cavernous sinus inflammation and cranial nerve palsies, until the sphenoid sinus was drained.
Again in Japan, Mutoh et al. Reference Mutoh, Adachi, Tsuji, Okunaka and Sakagami26 evaluated the efficacy of mastoidectomy in 18 patients with MRSA-infected chronic otitis media and tympanic membrane perforation, compared with 33 patients with methicillin-sensitive S aureus. Of the MRSA-infected patients, those undergoing mastoidectomy had a better graft success rate and fewer post-operative complications, compared with those not undergoing mastoidectomy.
From 2000 to 2005, again in South Korea, Park et al. Reference Park, Lee, Cha, Lee, Lee and Yeo8 investigated chronic otitis media pathogens and MRSA isolation rates. Of the 5988 staphylococci isolates recovered from a tertiary care hospital, 3712 (62 per cent) were MRSA. Of the 1162 bacterial strains identified in 1360 chronic otitis media patients, 628 (54 per cent) were staphylococci and 288 (46 per cent) of these were MRSA; thus accounting for 25 per cent of identified bacteria. All MRSA isolates were sensitive to vancomycin and teicoplanin, and 88 per cent were sensitive to trimethoprim plus sulphamethoxazole. The annual MRSA isolation rate did not change over the study period.
Again in the USA, Coticchia and DoharReference Coticchia and Dohar27 compared 17 children who developed MRSA otorrhoea after bilateral myringotomy with tympanostomy tube insertion to 19 similar patients with methicillin-sensitive S aureus otorrhoea. The development of MRSA otorrhoea was directly associated with the number of episodes of acute otitis media before bilateral myringotomy with tympanostomy tube insertion, and also with the number of antibiotic treatment courses and the duration of those courses after the procedure.
In Spain, Martín Salas et al. Reference Martín Salas, Gil-Setas and Mazón9 assessed the proportion of MRSA isolates compared with total S aureus isolates for all outpatient infection, including those from ear and tonsillar infections; they found 14.3 per cent in 2003 and 17.4 per cent in 2004.
In Poland, Pajor et al. Reference Pajor, Durko, Jankowski, Bartoszko-Tyczkowska and Stańczyk10 recovered 273 pathogen isolates from 228 patients with chronic otitis media: 117 (42 per cent) were S aureus and 54 (20 per cent) P aeruginosa. There were only four (3.4 per cent) MRSA isolates.
Several studies have evaluated the topical and systemic treatment of MRSA ear infections.
Lee et al. Reference Lee, Lee, Baek and Lim28 demonstrated topical efficacy of vancomycin (formulated with pluronic F-127) in treating MRSA chronic otitis media.
Kashiwamura et al. Reference Kashiwamura, Chida, Matsumura, Nakamaru, Suda and Terayama29 showed topical efficacy of Burow's solution in treating chronic otitis media; 35 (70 per cent) of the 50 ears assessed were ‘cured’ and 10 (20 per cent) were improved.
Jang et al. Reference Jang, Song and Wang30 assessed treatment of MRSA otorrhoea, and found topical vancomycin 25 mg/ml superior (curing 33/35 patients; 94 per cent) to 0.3 per cent gentamicin (curing four of 20; 20 per cent).
Al-Shawwa and WegnerReference Al-Shawwa and Wegner31 treated six children with acute otitis media with otorrhoea secondary to community-acquired MRSA. Five had tympanostomy tubes and one had a perforated tympanic membrane. None responded to β-lactam antibiotics or topical fluoroquinolone. The MRSA strains isolated were susceptible to trimethoprim plus sulphamethoxazole, gentamicin, rifampin and vancomycin. The importance of obtaining cultures from nonresponsive patients and determining the antimicrobial sensitivity was illustrated, as all patients responded to trimethoprim plus sulphamethoxazole and ear drops containing gentamicin or polymyxin B neomycin hydrocortisone.
Hunt and RobbReference Hunt and Robb32 reported a two-year-old child who had developed MRSA otorrhoea following traumatic tympanic membrane perforation, and who was successfully treated with fusidic acid topical drops.
BrookReference Brook33 described an infant with acute otitis media who failed amoxicillin plus clavulanate treatment. Tympanocentesis, performed after 48 hours, recovered MRSA susceptible to clindamycin. The child recovered after clindamycin therapy.
Brook and GoberReference Brook and Gober11 recovered S aureus and MRSA more often in spontaneously draining acute otitis media in children seen after the introduction of seven-valent pneumococcal vaccine (2001–2006), compared with those seen in the pre-vaccine period (1993–1998). Staphylococcus aureus was recovered from four of 50 (8 per cent) children (no MRSA isolates) before the vaccine was introduced, and from nine of 50 (18 per cent) children (five MRSA isolates) afterwards.
Sinusitis
Rutar et al. Reference Rutar, Zwick, Cockerham and Horton34 described a patient with bilateral orbital cellulitis, pansinusitis, cavernous sinus thrombosis and permanent, bilateral blindness due to community-acquired MRSA infection.
Huang and HungReference Huang and Hung12 isolated MRSA from 16 of 601 patients (2.7 per cent) with acute sinusitis. Multiple pathogens were more frequently found in children with MRSA, and eight of nine with multiple pathogens had previously received antibiotics. Five of seven adults with MRSA had undergone previous nasal procedures. All patients' symptoms resolved following oral antibiotics guided by culture sensitivities.
Brook et al. Reference Brook, Foote and Hausfeld13 assessed rates of recovery from MRSA in acute and chronic maxillary sinusitis, comparing the years 2001–2003 and 2004–2006. Two hundred and fifteen isolates were recovered in 2001–2003 (118 from acute and 97 from chronic sinusitis), and 243 isolates in 2004–2006 (126 from acute and 117 from chronic sinusitis). Staphylococcus aureus was isolated from 10 (8 per cent) of the patients with acute sinusitis between 2001 and 2003, of whom three (30 per cent) had MRSA, and from 13 (10 per cent) of the patients with acute sinusitis between 2004 and 2006, of whom nine (69 per cent) had MRSA (p < 0.01). Staphylococcus aureus was found in 15 (15 per cent) of the patients with chronic sinusitis between 2001 and 2003, of whom four (27 per cent) had MRSA, and from 23 (20 per cent) of the patients with chronic sinusitis between 2004 and 2006, of whom four (61 per cent) had MRSA (p < 0.05). Antimicrobials were administered over the last three months prior to patients culture was taken to 122 (57 per cent) of those with chronic sinusitis. Methicillin-resistant S aureus was isolated more often from these (three month treated) individuals (28/122; 23 per cent) than from those not treated previously (10/92; 11 per cent) (p < 0.05).
These data illustrate a significant increase in the rate of MRSA recovery from cases of acute and chronic maxillary sinusitis.
Several authors have described their experience in using oral and topical antibiotics to treat MRSA sinusitis.
GerencerReference Gerencer35 found that oral antibiotics alone (12 patients) or a combination of oral and topical antibiotics (16 patients) were equally effective in treating community-acquired MRSA sinusitis (mean resolution time, 5.7 weeks).
Solares et al. Reference Solares, Batra, Hall and Citardi36 demonstrated the efficacy of mupirocin nasal irrigation in managing 42 exacerbations of chronic MRSA sinusitis in 24 patients. They used either mupirocin nasal irrigations plus oral doxycycline (28 episodes), mupirocin nasal irrigations and oral trimethoprim plus sulphamethoxazole (four episodes), or mupirocin nasal irrigations alone (seven episodes). Only one of 27 repeat culture had MRSA on follow up, giving a recurrence rate of 1.75 per cent (range of recurrences, one to eight episodes).
Tabaee et al. Reference Tabaee, Anand and Yoon37 showed that intravenous antibiotics administered on an out-patient basis were effective in managing MRSA sinusitis. Five of the six patients studied (83.3 per cent) had negative MRSA cultures after such therapy.
Periorbital cellulitis
Anari et al. Reference Anari, Karagama, Fulton and Wilson38 reported a case of MRSA orbital abscess in a premature neonate.
Huang et al. Reference Huang, Lee and Lin39 described a child with bilateral, MRSA-positive, subperiosteal abscesses and multiple brain abscesses complicating acute sinusitis, who was successfully treated with vancomycin and rifampicin.
McKinley et al. Reference McKinley, Yen, Miller and Yen14 studied paediatric orbital cellulitis associated with sinusitis. Fifteen patients required only medical management, whereas 23 needed medical and surgical intervention. Methicillin-resistant S aureus represented 73 per cent of S aureus isolates.
Cervical lymphadenitis
Guss and KazahayaReference Guss and Kazahaya15 studied 62 children with suppurating cervical lymph glands. The commonest infective organism was S aureus (63 per cent of 49 positive cultures); of the S aureus isolates, 27 per cent were MRSA. All MRSA strains were susceptible to clindamycin and trimethoprim plus sulphamethoxazole; 63 per cent were susceptible to ciprofloxacin and 25 per cent to erythromycin. All MRSA isolates were identified during the latter half of the study period (2003–2006); none were identified prior to 2003.
Tonsillitis
Brook and FooteReference Brook and Foote16 investigated the rate of recovery of MRSA from tonsils removed from 44 children because of recurrent group A β-haemolytic streptococci infection, between 1998 and 2003. Methicillin-resistant S aureus was isolated from 16 per cent of the tonsils. Of the 26 S aureus isolates recovered from the tonsillar cores, seven (27 per cent) were MRSA, and of the 16 isolates isolated from the tonsillar surface, two (12.5 per cent) were MRSA. Five of the seven core isolates and all two of the surface isolates were also β-lactamase producers. All MRSA isolates were resistant to oxacillin, penicillin and erythromycin, and were susceptible to clindamycin, trimethoprim plus sulphamethoxazole, and vancomycin.
The emergence of MRSA in the tonsils of children with recurrent group A β-haemolytic streptococcal tonsillitis may contribute to the difficulty in eradicating such streptococci with penicillins, as most of the MRSA isolated in the study by Brooke and FooteReference Brook and Foote16 were also beta-lactamase producers.Reference Brook40 Beta-lactamase-producing MRSA can survive treatment with β-lactams, and can also shield group A β-haemolytic streptococci from penicillins by producing β-lactamase.Reference Brook40
Thyroiditis
Lethert et al. Reference Lethert, Bowerman, Pont, Earle and Garcia-Kennedy41 reported a patient with MRSA-positive suppurative thyroiditis who was successfully treated with vancomycin.
Elorza et al. Reference Elorza and Echenique-Elizonda42 reported a patient who had undergone total cystectomy for invasive bladder carcinoma. Three months later, he developed suppurative thyroiditis due to MRSA.
Retropharyngeal abscess
Constantinides et al. Reference Constantinides, Passant and Waddell43 described a case of MRSA parapharyngeal abscess associated with carotid artery infected pseudoaneurysm.
Sato et al. Reference Sato, Izumi, Toshima, Nagai, Muroi and Komatsu44 presented a patient with acute myeloid leukaemia complicated by MRSA retropharyngeal abscess, successfully treated with vancomycin and gentamicin lavage.
Fleisch et al. Reference Fleisch, Nolan, Gerber and Coffin45 reported two cases of MRSA retropharyngeal abscess in infants, one with jugular vein thrombosis.
Wright et al. Reference Wright, Stocks, Armstrong, Arnold and Gould17 demonstrated an increased incidence of retropharyngeal infection, and an increased role for MRSA in such infections, especially in infants less than one year of age. The number of cases doubled, comparing 2001–2005 with 1997–2001. In the first period, no MRSA was found, although one patient developed mediastinitis. In the second period, eight of 25 patients (32 per cent) with positive cultures had MRSA, and seven cases of mediastinitis occurred. Of the eight children with MRSA, six developed mediastinitis. The median age for all children with retropharyngeal infection was 32.5 months, and that for MRSA plus mediastinitis was six months.
Abscesses and wound infections of the head and neck
Parton et al. Reference Parton, Beasley, Harvey, Houghton and Jones46 presented four patients with MRSA wound infection following head and neck surgery. One patient had an MRSA mediastinal abscess which eroded into the innominate artery, causing a fatal haemorrhage. The others suffered serious wound infection, successfully treated with teicoplanin.
Ahmad and LeeReference Ahmad and Lee47 described two cases of MRSA neck infections, resulting in a deep neck abscess in one patient and the formation of a tracheoesophageal fistula in the other.
Naidu et al. Reference Naidu, Donepudi, Stocks, Buckingham and Thompson48 reported four children with MRSA deep neck abscesses. Drainage and antibiotic therapy successfully treated three patients. One patient developed mediastinitis, but survived after additional surgical treatment and prolonged antibiotic therapy.
Ossowski et al. Reference Ossowski, Chun, Suskind and Baroody18 compared the proportion of community-acquired MRSA infections in paediatric head and neck abscesses in 1999–2001 versus 2002–2004. In the first period, six (40 per cent) of 15 abscesses yielded S aureus, compared with 17 (58.6 per cent) of 29 abscesses in the second period. The proportion of abscesses yielding MRSA increased from 0 per cent (zero of six) in the first period to 64.7 per cent (11/17) in the second (p < 0.01).
Bothwell et al. Reference Bothwell, Shvidler and Cable19 studied 36 community-acquired MRSA isolates from head and neck infections, between 2003 and 2004. The MRSA infection rate increased from 21 to 64 per cent over that period. The distribution of community-acquired MRSA infections was: face (n = 12), nose (nine), ear (seven), neck (six) and other (two). All community-acquired MRSA isolates were resistant to cefazolin and penicillin, but most were sensitive to clindamycin.
Thomason et al. Reference Thomason, Brenski, McClay and Ehmer20 demonstrated an increase in the incidence of MRSA in 245 children who underwent incision and drainage of neck abscesses from 2001 to 2006. Methicillin-resistant S aureus accounted for 57 of the 123 (54 per cent) S aureus isolates, and for 27 per cent of all 209 bacterial isolates across 7 years. The yearly incidence of MRSA infection increased from 9 per cent in 2001 to 40 per cent in 2006. Abscesses in medial locations were less common in the MRSA group (p < 0.01) and the methicillin-sensitive S aureus group (p < 0.001), compared with the non S aureus group. The average patient ages by infective organism were: MRSA, 18.9 months; methicillin-sensitive S aureus, 18.7 months; and non S aureus, 47.6 months. Complication rates and clinical courses were similar in all groups.
Inman et al. Reference Inman, Rowe, Ghostine and Fleck21 studied 288 paediatric neck infections between 1999 and 2007. Staphylococcus aureus was isolated from 48 per cent of abscesses; 29 per cent of these isolates were community-acquired MRSA. Inman et al. could find no clinical risk factors which differentiated those patients at higher risk of MRSA. Patients with MRSA had an average age of 32.5 months, compared with 16 months for those with methicillin-sensitive S aureus.
Lemierre's syndrome
There are three reported cases of Lemierre's syndrome associated with community-acquired MRSA.Reference Fong and Watson49–Reference Kadviharan, Paramasivan, Bangs, Banga, Gupta and Sharma51 One patient had orbital cellulitis,Reference Kadviharan, Paramasivan, Bangs, Banga, Gupta and Sharma51 and another had splenic vein thrombosis.Reference Boga, Ozdogu, Diri, Oguzkurt, Asma and Yeral50
Discussion
The above data illustrate a significant increase in the incidence of MRSA in head and neck infections. This is in concordance with an overall increased incidence of MRSA in various other respiratory and non-respiratory infections.Reference Sakoulas and Moellering1, Reference Naseri, Jerris and Sobol2
The association between previous antimicrobial use and increased isolation of MRSA has been noted for various infections,Reference Boyce52, Reference Boga, Ozdogu, Diri, Oguzkurt, Asma and Yeral50 including sinusitis.Reference Brook, Foote and Hausfeld13, Reference Gerencer35, Reference Schneider-Lindner, Delaney, Dial, Dascal and Suissa53 Brook et al. Reference Brook, Foote and Hausfeld13 and GerencerReference Gerencer35 found that most patients with MRSA chronic sinusitis who had received previous antimicrobial therapy had been treated with either a fluoroquinolone or a macrolide. Since most MRSA strains are resistant to these agents, it is possible that these classes may select for MRSA.
Treatment of MRSA head and neck infections is challenging. When possible, drainage and debridement are of major importance. This includes drainage of abscesses and of infected sinuses or ears.
Although topical therapy of some infections may be possible, it is important to administer systemic antimicrobials that cover these organisms as well as other potential aerobic and anaerobic pathogens that may be present in polymicrobial infections. Although vancomycin represents the ‘gold standard’ of MRSA therapy, reports of increasing in vitro resistanceReference Howden, Johnson, Ward, Stinear and Davies54 and of clinical failuresReference Dombrowski and Winston55 underscore the need for alternative therapies. Older agents with favourable activity, available in both oral and intravenous forms, include trimethoprim plus sulphamethoxazole and clindamycin. At present, there is only limited clinical data to support their routine use as initial therapy of MRSA infections. However, these and other agents are being re-explored as potential treatments for community-acquired MRSA. Newer treatment options include linezolid, quinupristin-dalfopristin, daptomycin and tigecycline.Reference Clements, Halton, Graves, Pettitt, Morton and Looke56
Several studiesReference Suzuki, Nishimura and Baba6, Reference Lee, Lee, Baek and Lim28–Reference Hunt and Robb32, Reference Solares, Batra, Hall and Citardi36, Reference Tabaee, Anand and Yoon37 have discussed the potential use of topical antimicrobials. Nasal irrigation with mupirocin has been used in conjunction with infection control measures to successfully control an MRSA outbreak in an institution for the handicapped.Reference Jensen, Jensen, Larsen, Meyer, Junker and Rønne57 Although intranasal mupirocin is effective in eradicating colonisation, it is only marginally successful in eliminating MRSA colonisation of multiple body sites.Reference Boyce58, Reference Harbarth, Dharan, Liassine, Pascale, Auckenthaler and Pittet59 One major shortcoming of mupirocin is a growing, worldwide resistance. A recent study of 4980 MRSA isolates obtained between 1995 and 2004 from 32 Canadian hospitals reported that the proportion of MRSA with high-level mupirocin resistance, compared with mupirocin-sensitive MRSA, increased from 1.6 per cent in the first five years of surveillance to 7.0 per cent (p < 0.001) in 2004.Reference Simor, Stuart, Louie, Watt, Ofner-Agostini and Gravel60
A high prevalence of mupirocin-resistant MRSA isolates has been documented in surgical intensive care unit patients, despite low levels of mupirocin usage.Reference Jones, Rogers, Brookmeyer, Dunne, Storch and Coopersmith61 Jones et al. studied 302 MRSA isolates and found that 13.2 per cent were resistant to mupirocin, with 8.6 per cent having high-level resistance.
Despite the emergence of mupirocin resistance, this antimicrobial may still be effective in eradicating MRSA from chronically infected sinuses, because of the high intra-sinus concentration achieved with topical use. The use of animal models and prospective, randomised studies may provide more information on this question.
Culture-directed oral and topical antibiotics have been found to be effective in treating MRSA sinusitis.Reference Gerencer35 Although the gold standard culture specimen is obtained via surgical puncture,Reference Anon, Hadley, Craig, Poole, Ambrose and Benninger62 culture specimens obtained via meatal endoscopy can provide adequate results.Reference Benninger, Payne, Ferguson, Hadley and Ahmad63 Such topical antibiotics include gentamicin, tobramycin, vancomycin, ciprofloxacin and mupirocin. Their topical application offers the benefit of a high concentration at the infection site.
Further, prospective studies and continuous monitoring of MRSA isolates from head and neck infections are indicated to monitor future trends.
Conclusion
The data presented in this review demonstrate the increased role of MRSA in sinusitis, and underscore the importance of performing routine cultures of all head and neck infections, especially in patients who fail to respond to empirical antimicrobial therapy.



