Introduction
Nasal dermoids, gliomas and encephalocoeles are rare congenital malformations of ectopic neuroectoderm which occur in one in 20 000 to 40 000 births.Reference Hughes, Sharpino, Hunt and Tucker1 Nasal dermoids are the most common of these midline lesions.Reference Pensler, Bauer and Naidich2
During development, a projection of dura mater extends through the foramen caecum and transiently occupies the prenasal space. Failure of the fonticulus frontalis to fuse, or failure of the foramen caecum at the base of the frontal bones to obliterate, leaves a pathway along which neural tissue may extend into the prenasal space. Persistence of neural tissue results in nasal gliomas and encephalocoeles. Prior to regression back into the cranium, the dura may briefly contact the nasal skin. Defective regression of the embryological neuroectodermal tract may cause involution of ectoderm, leading to dermoid sinuses and cysts.Reference Zapata and Kearns3
Nasal dermoids may present as midline pits, fenestrae or discrete masses. They may appear anywhere from the glabella, along the bridge of the nose, to the base of the columella. There may be intermittent discharge of sebaceous material and/or pus, intermittent inflammation, osteomyelitis, local abscess, broadening of the nasal root or bridge, or intracranial complications.
Because of their clinical behaviour, nasal dermoids are best treated with complete surgical excision. Many surgical approaches have been advocated. Nearly all result in an external scar. Many parents find this difficult to accept, when they have presented with a seemingly small, inconspicuous nasal blemish. The option of an approach with minimal external scarring would obviously be preferred by parents. We wanted to develop a technique that did not result in a scar caused by the surgical approach. Mid-facial de-gloving involves considerable dissection, because the incision is distant to the lesion, but does have the advantage of no external scar. The trans-conjunctival approach may be good for laterally placed lesions, but it gives questionable access for midline lesions. We sought to explore the option of a closed rhinoplasty approach, to investigate whether it would provide adequate access and exposure to enable the removal of superficial nasal dermoids.
Methods
The study was approved by our institutional ethics committee. Participants and their parents gave consent in accordance with the Declaration of Helsinki.
Three boys aged five, nine and 12 years presented with midline nasal dermoids with minimal cutaneous involvement (Figures 1 to 3). Multiple sequences in multiple magnetic resonance imaging planes were performed to obtain maximum information, in order to ensure that the lesions were distinct, localised and without intracranial extension, before embarking on a closed approach. These three cases were very similar, and were all selected as suitable for a closed approach.

Fig. 1 A five-year-old boy referred with a supratip punctum with a protruding hair, and a mass immediately superior to it.

Fig. 2 Operative view showing a dermoid cyst punctum being cannulated.
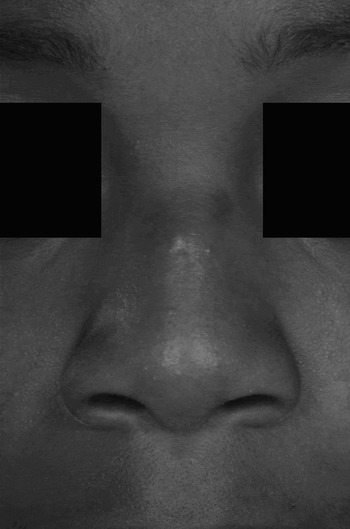
Fig. 3 A 12-year-old boy whose dermoid was a little more superior than those of our other two patients. Note scarring and hypopigmentation of the skin adjacent to the pit, secondary to recurrent infection.
Surgical technique
Excision proceeded in exactly the same way in each case. Under endotracheal general anaesthetic, the area for dissection was infiltrated with 2 per cent lignocaine and 1:80 000 adrenaline. A full transfixion and intercartilagenous incisions were made. An ellipse of skin, containing the punctum, was incised in the line of relaxed skin tension. For complete removal, excision of this skin was unavoidable, regardless of the approach. A sub-superficial muscular aponeurotic system (SMAS) layer was elevated around the cyst. The cyst was gently palpated through the punctum with a lacrimal probe, during the procedure, to aid identification of the tract. The most difficult part of the procedure was elevation of the thin skin overlying the dermoid. Angled, sharp scissors with a semi-blunt dissecting outer edge were best for this. Complete cutaneous elevation allowed exposure of the cyst, either directly with illumination, with or without loupes, or with an endoscope. Once the dermoid had been dissected distally, it could be passed through the incision to allow per-nasal circumferential dissection. There was adequate exposure all the way to the superior limit of all lesions. Internal incisions were closed with 4.0 Vicryl Rapide sutures. The skin breach and elliptical skin incision were closed with interrupted 6.0 Ethilon sutures.
Histopathological examination of the excised specimens was performed to confirm the diagnosis, and to examine for completeness of excision.
Results
Based on histological examination and relatively short follow up, our three patients had complete excision of their lesions and excellent cosmetic results (Figures 4 to 6).

Fig. 4 Post-operative view, showing a barely perceptible scar.

Fig. 5 For this patient, we incised a vertically orientated ellipse for excision of the punctum. The relaxed skin tension fell in this orientation because of its more caudal position. Again, the scar is barely perceptible.

Fig. 6 Three-weeks post-operative photograph, showing some hypopigmentation of the scar, along with some hypopigmentation of an area immediately superior to the scar, which was present pre-operatively. As in the other two cases, this patient and his parents were delighted with the result.
Discussion
A myriad of external approaches have been described for the excision of dermoid cysts, including: vertical, open rhinoplasty, transverse, inverted U, lateral rhinotomy and midbrow incision.Reference Pollock4–Reference Rohrich, Lowe and Schwartz11 Kelly et al. found that midline vertical incisions gave superior exposure compared with other open incisions.Reference Kelly, Strome and Hall7 Denoyelle et al. reported that 60 per cent of scars from vertical incisions widened.Reference Denoyelle, Ducroz, Roger and Garabedian5 Bradley reported that 37 per cent of patients had a poor long-term cosmetic outcome from vertical incisions.Reference Bradley6
Weiss et al. described the only two other reported cases of excision of nasal dermoids through a closed rhinoplasty incision.Reference Weiss, Robson and Mulliken12 In these cases, the indications for using intercartilagenous incisions were quite different from our cases. These authors reported extension of nasal dermoids under the bony nasal dorsum, with intracranial extension. There was minimal or no cutaneous involvement, and most of the cysts were contained deep to the nasal bones. Therefore, bilateral intercartilagenous incisions provided access for endoscopic surgical excision up to the region of the foramen caecum, thus obviating the need for craniotomy.
These two cases were included in Rahbar and colleagues' 30-year, Boston experience of 42 patients with dermoid cysts, the largest reported series thus far.Reference Rahbar, Shah, Mulliken, Robson, Perez-Atayade and Proctor8 External incisions were used for access in the other 40 patients. Five of the 42 patients suffered recurrence. One recurrence occurred in one of the two patients whose dermoids had been excised via a transnasal, endoscopic approach, described by Weiss et al. Reference Weiss, Robson and Mulliken12 This recurrence occurred at the nasal tip, four years after the initial procedure.
External rhinoplasty has been supported by many authors as the preferred approach for extracranial excision of nasal dermoids, and may be combined with a craniotomy for dermoids with intracranial extension.Reference Denoyelle, Ducroz, Roger and Garabedian5, Reference Kelly, Strome and Hall7, Reference Posnick, Bortoluzzi and Armstrong9, Reference Rohrich, Lowe and Schwartz11, Reference Bilkay, Gundogan, Ozek, Tokat, Gurler and Songur13–Reference Bloom, Carvalho, Dory, Brewster, Wickersham and Kearns15 There are no reported unsatisfactory cosmetic results of the transcolumellar scar, amongst the relatively small number of cases published. The scar is well concealed and the approach provides wide exposure. Given such good reported cosmetic results and adequate exposure with this approach, one might question the need to modify it.
Cosmetic results are the most difficult to judge. They are evaluated by subjective criteria. However, there can be no question regarding the scar from the closed rhinoplasty approach as, other than the unavoidable excision of the punctum, there are no external incisions. Transverse broken line external incisions are said to become ‘almost invisible’ when the tissues are handled delicately and sutured precisely. This may be true, but a completely invisible scar is always preferable to an almost invisible one.
All of the cases we selected for a closed rhinoplasty approach involved nasal dermoids that were both distal and superficial. Exposure was entirely adequate. There would not have been significantly more exposure of the cysts had an external rhinoplasty approach been used, and such an approach would have entailed more dissection of uninvolved tissues, potentially leading to more complications, the loss of some nasal support mechanisms, and restricted secondary growth.
Two well known complications of transcolumellar external rhinoplasty incisions in adults (with many large series reported) are asymmetrical healing and necrosis of the lower end of the skin flap (which may result in severe scarring and retraction).Reference Huizing and de Groot16, Reference Toriumi and Johnson17 It has been reported that 1.5 to 25 per cent of patients find the transcolumellar scar unacceptable.Reference Foda18–Reference Constantian22
There is often a residual concavity of the nasal bones after removal of nasal dermoids. Mankarious and Smith have described successful immediate reconstruction using an open rhinoplasty approach.Reference Mankarious and Smith14 One of our cases had a minor concavity of the dorsum of the nasal frame, with a satisfactory aesthetic contour. For more conspicuous concavities, we would still prefer to avoid primary reconstruction, as remodelling of the nasal bones is likely to occur; however, we can report that there was adequate intra-operative exposure to place a graft if required.
When the sinus tract extends deep to the nasal bones, a nasal osteotomy will give better exposure. External rhinoplasty provides wide exposure for nasal osteotomy and allows easy access to follow the sinus tract to the skull base. None of our cases had sinus tracts that extended deep to the nasal bones, and therefore nasal osteotomy was not required. However, it is perceivable that osteotomies could be performed through intercartilagenous incisions, in much the same way as in closed rhinoplasty, for cases with limited deep extension.
A careful pre-operative assessment is essential to choosing an appropriate operative approach. A combined approach with a neurosurgical team should be considered when radiological evidence of intracranial extension is found. A closed rhinoplasty approach is not suitable for lesions in the nasal-glabellar area without a sinus opening. Associated multiple anomalies occur in 6 to 41 per cent of patients.Reference Denoyelle, Ducroz, Roger and Garabedian5, Reference Wardinsky, Pagon, Kropp, Hayden and Clarren23 Arguably, external approaches are more appropriate for patients with locally associated anomalies such as cleft lip.
The primary aim must be total extirpation. This must not be compromised by aesthetic considerations. Recurrence rates of 50–100 per cent have been reported in cases in which dermal components were incompletely removed.Reference Yavuzer, Bier and Jackson10, Reference Carroll, Gaffney and McShane24 Recurrence may result in infection, further surgery and a far worse cosmetic outcome, or, worse still, may potentially lead to ocular or intracranial complications. Therefore, cases suitable for a closed rhinoplasty approach must be carefully selected. Our recommendation, albeit from our currently limited experience, is that this approach is only appropriate for nasal dermoids that are small, superficial and distal.
We know from the experience of others that recurrence may occur years after the initial procedure.Reference Denoyelle, Ducroz, Roger and Garabedian5, Reference Rahbar, Shah, Mulliken, Robson, Perez-Atayade and Proctor8 We acknowledge that long-term follow up is essential to monitor for recurrence and to assess nasal growth and delayed deformity, and this may affect the true outcome. However, based on histological examination and relatively short follow up, our three patients had successful cosmetic results and complete excision of their lesions.
The majority of nasal dermoids are confined to the superficial nasal area.Reference Hughes, Sharpino, Hunt and Tucker1, Reference Rahbar, Shah, Mulliken, Robson, Perez-Atayade and Proctor8, Reference Bloom, Carvalho, Dory, Brewster, Wickersham and Kearns15 Therefore, many dermoid cysts are potentially amenable to excision through a closed rhinoplasty approach.
Conclusion
The closed rhinoplasty incision is another approach in the surgeon's armamentarium for excision of small, superficial, distal nasal dermoids. In well selected cases, this approach gives optimal cosmetic results, provides adequate exposure with minimal dissection, and allows total extirpation.








