Introduction
Myringoplasty is a commonly performed operation in otolaryngology. The literature estimates that myringoplasty success rates, based on graft take, are between 60 and 90 per cent.Reference Kotecha, Fowler and Topham1–Reference Onal, Uguz, Kazikdas, Gursoy and Gokce4 Many authors have debated the various factors that predict success, such as tympanic membrane perforation size, surgical technique, graft type and post-operative dressing.Reference Yung3,Reference Onal, Uguz, Kazikdas, Gursoy and Gokce4 However, no consensus on the optimal approach has been reached.
Traditionally, packing is placed within the external auditory canal following myringoplasty to protect the operative site and hold the graft in situ, thus promoting healing. Bismuth iodoform paraffin paste is widely used in the UK and requires removal approximately two to three weeks post-operatively.Reference Zeitoun, Sandhu, Kuo and MacNamara5 However, many other packing types have been used, including Pope wick, Silastic™ sheeting and Spongostan™ haemostatic sponges.Reference Zeitoun, Sandhu, Kuo and MacNamara5,Reference Lou6 Likewise, various ointments such as Otocomb Otic® and Tri-Adcortyl® Ointment have been trialled to see if these improve myringoplasty success rates.Reference Zeitoun, Sandhu, Kuo and MacNamara5–Reference Nakhla, Takwoingi and Sinha8 Others have argued that using no post-operative dressing may also be safe and appropriate.Reference Javed, Whitwell, Hajioff, Robinson, Rea and Macleod9
Similarly, the optimal site of harvest for the myringoplasty graft has been debated. Temporalis fascia is the most widely employed material for myringoplasty graft, as well as tragal or conchal cartilage and perichondrium.Reference Shekharappa and Siddappa10–Reference Cavaliere, Mottola, Rondinelli and Iemma11 More recently, acellular porcine small intestinal submucosa (Biodesign; Cook Medical, Bloomington, Indiana, USA) has been used in myringoplasty as an alternative to autologous graft materials.Reference Basonbul and Cohen12
No study has previously examined the role of bismuth iodoform paraffin paste versus Spongostan packing alone in terms of graft failure rates in myringoplasty. Likewise, there has been little discussion of the optimal graft material and the impact this has on myringoplasty success rate. This study aimed to determine whether the choice of graft material and type of post-operative packing are associated with higher endoscopic myringoplasty success rates.
Materials and methods
A retrospective review was conducted of all patients undergoing endoscopic myringoplasty for tympanic membrane perforation performed in a single tertiary ENT unit between January 2017 and January 2020 (three years). Data were collected on: patient demographics, tympanic membrane perforation size and site pre-operatively, pre- and post-operative audiology results, intra-operative details (operating surgeon grade, site for graft harvest, packing used), myringoplasty success rate, and post-operative complications. Mean hearing loss was calculated from patients’ audiograms using the pure tone average (PTA) across frequencies of 0.5, 1 and 2 kHz, measured in decibels.
The patients of two consultant otologists were included in this study. Surgeon one typically uses tragal cartilage graft and bismuth iodoform paraffin paste dressing. Surgeon two typically uses conchal cartilage graft, temporalis fat or fascia graft, and Spongostan dressing. Patients are followed up at two to three weeks, three months, and six months post-operatively. All patients under the care of these two consultant otologists who were operated on in the study period were included.
A comparative analysis was undertaken to examine the effect of intra-operative factors, including graft material (conchal cartilage, tragal cartilage, temporalis fat or fascia, Biodesign) and auditory canal packing (bismuth iodoform paraffin paste, Spongostan), on graft success rates. Myringoplasty success was defined as an intact tympanic membrane at six months post-operatively.
Inclusion criteria
All sequential patients who underwent endoscopic myringoplasty or type 1 tympanoplasty during the study time period were retrospectively identified. All patients had been operated by the two consultant otologists in our unit (as is routine practice).
Exclusion criteria
Patients undergoing any further otological procedure (other than myringoplasty or type 1 tympanoplasty) were excluded.
Analysis
Data were stored anonymously and analysed in Microsoft Excel® spreadsheet software. Means, percentages and 95 per cent confidence intervals (CIs) are presented to compare with the data in the literature. The Z-score for comparing two population proportions and statistical significance (defined as p < 0.05) was calculated using the Social Sciences Statistics calculator (www.socscistatistics.com). The strengthening the reporting of observational studies in epidemiology (‘STROBE’) reporting checklist was followed for this study.
Results
Ninety-eight patients were identified who fulfilled the inclusion criteria. Comparisons were made in terms of outcomes between: patients receiving bismuth iodoform paraffin paste versus Spongostan packing intra-operatively, the site or material of graft harvest (tragal cartilage, conchal cartilage, temporalis fat or fascia, and Biodesign), and the operating surgeon. The endoscopic approach was used in all patients.
Choice of dressing
Bismuth iodoform paraffin paste
There were 45 patients in this group, 23 were male and 22 were female. The mean age was 44.47 years (range, 10–84 years).
Regarding the size of the tympanic membrane perforation pre-operatively, 10 perforations were small in diameter (less than 30 per cent of the tympanic membrane area), 27 were medium (30–60 per cent) and 8 were large (more than 60 per cent). Regarding the procedures, 51.1 per cent (n = 23) were performed by a consultant and 48.9 per cent (n = 22) were performed by a supervised trainee. Tragal cartilage or perichondrium was utilised for all 45 cases.
There was an objective improvement or no change between pre-operative and post-operative PTA thresholds in 88.9 per cent of patients (n = 40). The mean average hearing loss was 41.9 dB pre-operatively (range, 12.5–90 dB) and 34.8 dB post-operatively (range, 5–100 dB).
The myringoplasty success rate was 86.7 per cent (n = 39, 95 per cent CI = 73.2–95.0). Six patients (13.3 per cent) had graft failure post-operatively, and a further five patients (11.1 per cent) experienced other complications, including three post-operative infections, one iodine reaction and one ‘dead ear’.
Spongostan
There were 53 patients in this group, 23 were male and 30 were female. The mean age was 24.0 years (range, 10–60 years).
Regarding the size of the perforation pre-operatively, 13 were small, 26 were medium and 11 were large. Regarding the procedures, 37.7 per cent (n = 20) were performed by a consultant and 62.3 per cent (n = 33) were performed by a supervised trainee. Tragal cartilage was used as the graft in 18 patients, conchal cartilage in 16, temporalis fascia or fat in 10, and Biodesign in 6 patients.
There was an objective improvement or no change between pre-operative and post-operative PTA in 84.9 per cent of patients (n = 45). The mean average hearing loss was 33.4 dB pre-operatively (range, 13.75–76.25 dB) and 21.5 dB post-operatively (range, 5–75 dB).
The myringoplasty success rate was 84.9 per cent (95 per cent CI = 72.4–93.3). This was not statistically significant when compared with the success rate for the bismuth iodoform paraffin paste group (Z-score = 0.25, p = 0.80) (Figure 1). Post-operatively, 15.1 per cent of patients (n = 8) had graft failure. The remaining post-operative complications included three post-operative infections, one granular polyp in the external auditory canal and one canal stenosis. In total, 9.4 per cent of patients had complications.
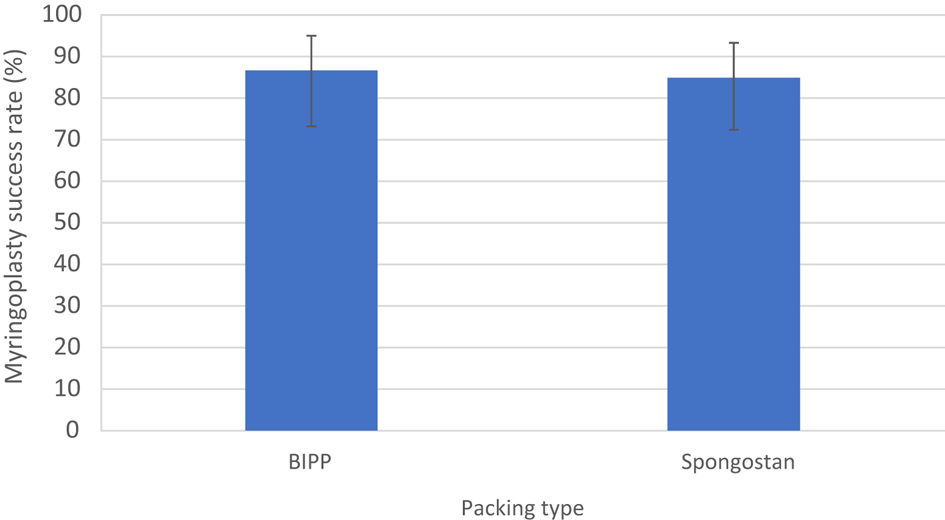
Fig. 1. Myringoplasty success rate (with 95 per cent confidence interval bars) according to post-operative packing type used. BIPP = bismuth iodoform paraffin paste
Choice of graft material
Conchal cartilage
Conchal cartilage was used in 17 patients. Regarding perforation size, 2 were small, 10 were medium and 5 were large. Eight procedures were carried out by a consultant and nine were performed by a supervised trainee. Mean audiology thresholds improved from 34.4 dB to 23.3 dB, with 15 patients (88.2 per cent) showing an improvement or no change between pre- and post-operative audiograms.
The myringoplasty success rate was 100.0 per cent (one-sided 95 per cent CI = 97.5–100.0). The graft failure rate was 0.0 per cent (n = 0), and 5.9 per cent of patients (n = 1) had a post-operative infection.
Tragal cartilage
Tragal cartilage or perichondrium was used in 65 patients. Regarding perforation size, 13 were small, 39 were medium and 13 were large. Thirty-one procedures were carried out by a consultant and 34 were performed by a supervised trainee. Mean audiology thresholds improved from 39.8 dB to 30.2 dB, with 57 patients (87.7 per cent) showing an improvement or no change between pre- and post-operative audiograms.
The myringoplasty success rate was 84.6 per cent (95 per cent CI = 73.5–92.4). There was no statistically significant difference from conchal cartilage (Z-score = 1.73, p = 0.08) (Figure 2). The graft failure rate was 15.4 per cent (n = 10), and 3.1 per cent of patients (n = 2) had a post-operative infection.
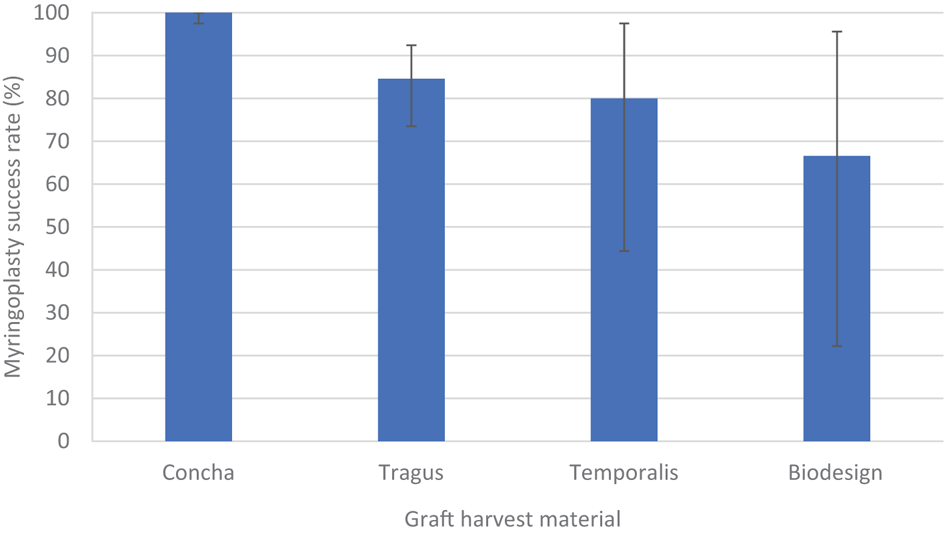
Fig. 2. Myringoplasty success rate (with 95 per cent confidence interval bars) according to graft harvest material or site.
Temporalis fat or fascia
Temporalis fat or fascia was used in 10 patients. Regarding perforation size, five were small, three were medium and two were large. Four procedures were carried out by a consultant and six were performed by a supervised trainee. Mean audiology thresholds improved from 30.6 dB to 21.9 dB, with nine patients (90.0 per cent) showing an improvement or no change between pre- and post-operative audiograms.
The myringoplasty success rate was 80.0 per cent (95 per cent CI = 44.4–97.5). There was no statistically significant difference from conchal cartilage (Z-score = 1.92, p = 0.05) (Figure 2). The graft failure rate was 20.0 per cent (n = 2); 10.0 per cent of patients (n = 1) had a post-operative infection and 10.0 per cent (n = 1) had canal stenosis.
Biodesign
Biodesign was used in six patients. Regarding perforation size, two were small, three were medium and one was large. All six procedures were performed by supervised trainees. Mean audiology thresholds improved from 31.9 dB to 19.0 dB, with five patients (83.3 per cent) showing an improvement or no change between pre- and post-operative audiograms.
The myringoplasty success rate was 66.7 per cent (95 per cent CI = 22.2–95.7). This was statistically significant compared with conchal cartilage (Z = 2.49, p = 0.01) (Figure 2). The graft failure rate was 33.3 per cent (n = 2). There were no other post-operative complications reported in this group.
Operating surgeon
The procedures for a total of 44 cases were performed by a consultant, with a graft failure rate of 14.0 per cent (n = 6, 95 per cent CI = 5.3–27.9) and a complication rate of 11.4 per cent (3 post-operative infections, 1 iodine reaction and 1 granular polyp in the external auditory canal). Post-operatively, 37 patients (86.0 per cent) had an improvement or no change in their audiological thresholds.
In 56 cases, the procedures were performed by a supervised trainee, with a graft failure rate of 14.5 per cent (n = 8, 95 per cent CI = 6.5–26.6) and a complication rate of 8.9 per cent (3 post-operative infections, 1 ‘dead ear’ and 1 canal stenosis). Post-operatively, 48 patients (87.3 per cent) had an improvement or no change in their audiological thresholds.
Discussion
This study has demonstrated the impact of various factors on long-term myringoplasty success rates, notably the type of packing used and the material used to graft the tympanic membrane perforation. This is the largest study to assess the difference between bismuth iodoform paraffin paste and Spongostan in terms of myringoplasty success.
The overall success rate for endoscopic myringoplasty was 86 per cent. In this study, there was no significant difference between graft failure rates in patients receiving bismuth iodoform paraffin paste versus Spongostan (13.3 per cent vs 15.1 per cent, respectively; p > 0.05), and the proportions of patients with improved audiological thresholds were equivalent. The graft success rate was superior to that in the existing literature, which has estimated the success rate in patients receiving bismuth iodoform paraffin paste to be approximately 75 per cent.Reference Zeitoun, Sandhu, Kuo and MacNamara5–Reference Nakhla, Takwoingi and Sinha8 This is the first study to assess the value of Spongostan in terms of endoscopic myringoplasty success.
In this study sample, there was one adverse reaction to iodine. This is a complication unique to the use of bismuth iodoform paraffin paste, which should be avoided in those with known sensitivity to iodine.Reference Bennett, Bartle and Yung13 Specifically, one patient had a minor allergic reaction, which resolved on removal of the pack, with no long-term complications. Great care must be taken when placing the bismuth iodoform paraffin paste: it must not be packed too tightly (which might disturb the tympanomeatal flap), but also not too loosely (as this may allow early extrusion).Reference Nakhla, Takwoingi and Sinha8 Bismuth iodoform paraffin paste requires removal from the ear canal, which can sometimes cause patient discomfort and bleeding (patients with bismuth iodoform paraffin paste in our cohort were seen at three weeks post-operatively for removal; however, patients in both cohorts had three out-patient appointments in total before being discharged).Reference Alsanosi14 This latter issue highlights one of the benefits of Spongostan, which is an absorbable, haemostatic packing material that does not require removal post-operatively.15
The choice of bismuth iodoform paraffin paste or Spongostan as dressing to the ear canal was made according to the preference of each consultant in our study. When comparing the bismuth iodoform paraffin paste and Spongostan patients, the Spongostan cohort were largely younger patients, and a larger proportion of cases were performed by a supervised trainee. This may have an impact on the generalisability of the results. The difference in mean ages between the two treatment groups was an incidental observation.
Literature has previously suggested that tragal or conchal cartilage is superior to temporalis fat or fascia in tympanic membrane reconstruction in myringoplasty, with previous success rates stated as 97.7 per cent.Reference Demirpehlivan, Onal, Arslanoglu, Songu, Ciger and Can16,Reference Zahnert, Hüttenbrink, Mürbe and Bornitz17 When considering the site of tympanic membrane reconstruction graft harvest in our study, conchal cartilage had a success rate of 100.0 per cent and tragal cartilage had a success rate of 84.6 per cent. Despite this apparent superiority, the difference failed to reach statistical significance (p > 0.05). The use of conchal cartilage showed a statistically significant difference from Biodesign (p < 0.05); however, this may be an unreliable estimate because of the small number of patients within these respective cohorts. This study supports the notion that cartilage-reinforced myringoplasty is superior to temporalis fat or fascia with regard to long-term success.Reference Demirpehlivan, Onal, Arslanoglu, Songu, Ciger and Can16,Reference Zahnert, Hüttenbrink, Mürbe and Bornitz17
The authors postulate that the more concave shape of conchal cartilage compared with the less concave tragal cartilage may confer an advantage when considering myringoplasty success and graft take. This has not been investigated in the literature previously, and further study would be needed for this to be adequately assessed.
The relationship between perforation size and myringoplasty success has been debated in the literature.Reference Lee, Kelly and Mills2,Reference Nakhla, Takwoingi and Sinha8,Reference Wasson, Papadimitriou and Pau18 In our study, the distribution of small (less than 30 per cent of the tympanic membrane area), medium (30–60 per cent) and large (more than 60 per cent) tympanic membrane perforations was equal between the subgroups.
• Myringoplasty success rate is estimated to be around 60–90 per cent
• Graft success depends on factors including perforation size, surgical technique, graft type and post-operative dressing
• In this study, Spongostan ear canal packing was equivalent to bismuth iodoform paraffin paste packing in terms of myringoplasty success rate
• Conchal cartilage was the superior graft harvest material when compared to tragal cartilage, Biodesign, and temporalis fat or fascia success rates
• The overall success rate of endoscopic myringoplasty was 86 per cent
A strength of this comparative, retrospective review is that the data are derived from two consultant otologists who either performed or supervised a trainee performing all of the myringoplasty procedures assessed. Likewise, all patients in this study were followed up to six months, which is longer than in other studies (typically three months), and demonstrates the long-term impact of these factors on myringoplasty success.
Further investigation is required to determine all factors that account for myringoplasty success, in order to achieve consensus and potentially standardise the approach used amongst ENT surgeons.
Conclusion
Multiple factors are theorised to impact myringoplasty success rates. This study has shown that Spongostan packing is equivalent to bismuth iodoform paraffin paste in terms of myringoplasty success. Conchal cartilage was the superior graft harvest material in this study when compared with the success rates for tragal cartilage, Biodesign, and temporalis fat or fascia. Biodesign as graft material had a poor outcome in this study, but the cohort size was too small to draw a definitive conclusion. Thus, the post-operative packing and graft material must be chosen with these considerations in mind.
Acknowledgement
The authors would like to thank the ENT department staff at Morriston Hospital, Swansea.
Data availability statement
Data are available from the authors on reasonable request.
Competing interests
None declared




