Introduction
Alkaptonuria is a rare inborn error of metabolism (autosomal recessive), in which there is increased homogentisic acid caused by the lack of the enzyme homogentisate dioxygenase. Excess homogentisic acid is oxidised to a melanin-like polymer, a process known as ochronosis. The clinical manifestations of alkaptonuria are due to either the excess homogentisic acid or the ensuing ochronosis.Reference Ranganath and Cox1
Alkaptonuria can be recognised at birth by the characteristic dark urine and discolouration of nappies due to homogentisic aciduria. However, if this is missed or not recognised as being of importance, patients grow into early adulthood and manifest the full multisystem involvement with premature irreversible marked morbidity, affecting virtually all connective tissues.Reference Ranganath, Jarvis and Gallagher2 Therefore, all opportunities to enhance early diagnosis are important and worthwhile. This is especially true now that a potential disease-modifying therapy, nitisinone, is available.
While the major morbidity of alkaptonuria derives from involvement of the musculoskeletal system, otological symptoms such as discolouration of the pinna and cerumen are well documented and are cardinal features.Reference Perry, Suwannarat, Furst, Gahl and Gerber3–Reference Srsen7 Three case reports also make reference to discolouration of the tympanic membrane.Reference Sanji, Reddy and Channegowda8–Reference Pau10 Some studies have additionally suggested that hearing loss may be a feature of alkaptonuria.Reference Sagit, Uludag and San9, Reference Pau10 Nose and throat symptoms are less commonly documented, but include discolouration of nasal and laryngeal cartilage.Reference Helliwell, Gallagher and Ranganath6, Reference Sanji, Reddy and Channegowda8
Systematic investigation and reporting is difficult in rare diseases such as alkaptonuria, as most reports are of individual cases. It is often difficult to get an idea of the true frequency of clinical features. Studying a series of patients enables a balanced description of clinical manifestations.
This study aimed to describe the ENT manifestations of alkaptonuria in a cohort of patients presenting to the National Centre for Alkaptonuria at the Royal Liverpool University Hospital, and to discuss potential causes of hearing loss.
Materials and methods
The National Centre of Alkaptonuria was established at the Royal Liverpool University Hospital in April 2012 and is supported by government funding for rare clinical diseases. Patients attend on a yearly basis, and are assessed by otorhinolaryngologists and a range of other specialists. All patients have a proven diagnosis of alkaptonuria, both by means of homogentisic aciduria and genetic testing.
During their visit, patients complete a detailed questionnaire regarding their condition. General demographics are collected, including gender and age. Patients are asked specific questions related to ENT manifestations. These address otological signs such as discolouration, otalgia, hearing loss, and rhinological and laryngological symptoms.
All ENT assessments were carried out in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and the Helsinki Declaration of 1975, as revised in 2000. In addition, the institutional review body (Royal Liverpool University Hospital) explicitly approved the National Alkaptonuria Service from which these data were generated.
Informed consent for inclusion in the study was obtained from all patients. As this is a clinical practice article, a standard research ethics process was not necessary. The data from these patients have been completely anonymised. The data were obtained following standard clinical assessments upon referral to the National Alkaptonuria Service in Liverpool. Patients are informed verbally and through written materials about the activities of the National Alkaptonuria Service; these materials included a patient information booklet of the National Alkaptonuria Service that explicitly informs them about the assessments.
All patients underwent a full ENT examination, including otoscopy and flexible nasolaryngoscopy. Pure tone audiometry was performed along with tympanometry where appropriate. Pure tone audiometry results were averaged for right and left ears using 0.5, 1, 2, 4, 6 and 8 kHz frequencies to ensure low and high frequency losses were not missed. The 8 kHz hearing frequencies were also analysed in isolation to allow comparison with previous studies. Hearing loss of 20 dB was accepted as the cut off for normal hearing.11 Individual audiograms were reviewed to establish the type of hearing loss. A pre-printed proforma was used to record data.
Results
Twenty patient data sets were analysed. Eleven patients were male and nine were female. The average age of patients was 48 years, with a range of 18–72 years. The average age at diagnosis was 24 years, with a range of 0–65 years. Eighteen of the 20 patients (90 per cent) had an ENT sign or symptom.
Otological signs and symptoms
Eighteen of the 20 patients had 1 or more otological sign or symptom (Table I). The majority of these were discolouration of the pinna or cerumen (Figures 1–3). Other signs included discolouration of the tympanic membrane or middle-ear cavities (observed as darkening behind the tympanic membrane) (Figure 4). Of the four patients without discolouration, three reported other ENT symptoms including tinnitus and otalgia.

Fig. 1 Pinna discolouration.

Fig. 2 Pinna discolouration in another patient.

Fig. 3 Black discolouration of cerumen.
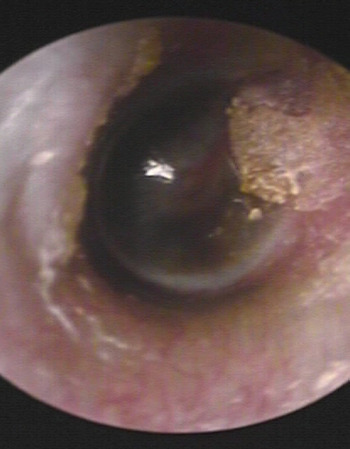
Fig. 4 Middle-ear discolouration.
Table I Otological signs and symptoms

Audiological findings
Pure tone audiometry averages demonstrated hearing loss in 7 of the 20 patients. The types and patterns of hearing loss are shown in Table II. All were cases of mild hearing impairments. The average age of those patients with hearing loss was 63 years (range, 53–72 years). All tympanograms performed (where applicable) were type A (normal).
Table II Patients with average hearing thresholds above 20 dB HL

Hearing in patients with a hearing threshold above 20 dB HL at 8 kHz was also examined in isolation (Table III). Ten of the 20 patients met this criterion. The average age for these patients was 54.7 years (range, 22–72 years). All 10 patients had some degree of high frequency loss; this was a mild impairment in 50 per cent of cases.
Table III Patients with hearing loss at 8 kHz

Degree of hearing loss as per British Audiology Society.11 *Threshold from worse hearing ear.
Nasal signs and symptoms
One patient had discolouration of the nasal septum on examination. Six patients reported nasal symptoms; three reported nasal obstruction, two hyposmia and three rhinorrhoea.
Throat signs and symptoms
One patient had discolouration affecting the area adjacent to the apex of the right pyriform fossa, as observed with flexible nasolaryngoscopy. Three patients reported throat symptoms: one reported occasional dysphagia; one reported intermittent dysphagia and hoarseness; and the third patient reported mild dysphagia and slurred speech, but this was attributed to a previous stroke.
Discussion
We report, for the first time, the ENT findings in a cohort of alkaptonuria patients. The findings included discolouration of: cerumen, the middle ear and tympanic membrane, and the cartilages of the pinna and nasal septum, as well as areas of the pharynx. Hearing loss, in relation to findings within this cohort of patients and in previous reports, is also discussed.
Historically, the cardinal features of alkaptonuria, including discolouration of sclera and the external ear, were described by Garrod in his first published manuscript in 1899, in which he outlined the key features of the disease.Reference Garrod12 He described the condition more extensively in his subsequent seminal work Inborn Errors of Metabolism, published in 1909.Reference Garrod13
Discolouration of the pinna is well documented in a number of studies.Reference Turiansky and Levin4–Reference Helliwell, Gallagher and Ranganath6 An article on the natural history of the condition describes this discolouration as developing in patients over the age of 30 years.Reference Phornphutkul, Introne, Perry, Bernardini, Murphey and Fitzpatrick5 Our study corroborates this, with no patients under the age of 30 years displaying pinna discolouration. Nodules on the pinna have been described as a presenting feature,Reference Sanji, Reddy and Channegowda8 although none were observed in this study.
Three case reports make reference to discolouration of the tympanic membrane.Reference Sanji, Reddy and Channegowda8–Reference Pau10 In one, the presenting features were hearing loss and tinnitus.Reference Sagit, Uludag and San9 This was a case of bilateral, mixed, high frequency hearing loss. It was proposed that the conductive element of the hearing loss was due to altered tympanic membrane elasticity or ochronotic impairment of the inter-ossicular joints. A further case demonstrating darkening of the tympanic membrane also found a mixed, high frequency hearing loss and concluded similar mechanisms as the cause.Reference Pau10
In this study, two patients had discolouration of the tympanic membrane, both right-sided. One was described as a general dark discolouration, with the other displaying a dark rim around the tympanic membrane. Another patient had dark discolouration of the middle ear. These findings did not seem to correlate with hearing loss in all cases. The patient with general dark discolouration of the tympanic membrane had normal hearing thresholds and no other otological symptoms. The patient with the dark rim around the right tympanic membrane displayed a mild bilateral high frequency hearing loss, but reported no symptoms. The patient with the dark middle ear showed a mild bilateral sensorineural high frequency hearing loss, but reported no symptoms.
A search of previous reports of hearing loss associated with alkaptonuria revealed two cases of mixed high frequency hearing loss.Reference Sagit, Uludag and San9, Reference Pau10 Only one of the patients in this study demonstrated a similar pattern. It has been proposed that stiffening of the tympanic membrane is one potential cause for the conductive element. Despite this, in the two previous reported cases, type A tympanograms were recorded. In this study, of the two patients with dark tympanic membranes, one had normal hearing thresholds and therefore did not have a tympanogram, and the other had a type A tympanogram. Loss of compliance of the tympanic membrane would also be unlikely to give a solely high frequency loss.
Another proposed theory for a conductive hearing loss is inter-ossicular joint ochronosis.Reference Sagit, Uludag and San9 These synovial joints have, as of yet, not undergone any direct histological study. They do, however, share similarities with the elbow joint, as they are non-weight bearing joints, where histological examination has shown marked pigmentation of the cartilage.Reference Helliwell, Gallagher and Ranganath6 Histological examination of bone shows slight pigmentation of the periosteal surface, but not of the bone itself. Tendons and ligaments are variably pigmented, and spontaneous ruptures are reported.Reference Helliwell, Gallagher and Ranganath6 Therefore, if the cause of the conductive element is within the middle ear, a potential mechanism could be ossicular discontinuity. In our series, however, no significant conductive loss was seen.
When hearing loss was analysed in more detail, 10 of the 20 patients had hearing loss at 8 kHz. The average age of these patients was 54.7 years (Table III). Because of the small numbers studied, this average age may be somewhat skewed; one patient with very mild hearing impairment at high frequencies (bilateral threshold at 8 kHz of 25 dB HL) was aged 22 years. Given that hearing loss is common in the general population, with quoted figures of 45.9 per cent,Reference Cruickshanks, Wiley, Tweed, Klein, Klein and Mares-Perlman14 it is unclear from this study whether high frequency hearing loss is an associated feature of alkaptonuria.
As the majority of patients in this study had normal hearing thresholds, and given that those with increased thresholds are more likely to have a sensorineural hearing loss, it is difficult to conclude that there is an association between hearing loss and alkaptonuria. Further audiological examination of patients during yearly reviews will help to clarify whether any association exists.
Dark pigmentation of the cerumen is also commonly observed in alkaptonuria patients, and is the presenting feature in some cases. It may occur early in otherwise asymptomatic individuals.Reference Srsen7 In this study, 13 patients (65 per cent) had discolouration of the cerumen. The average age of these patients was 50 years (range, 19–72 years). Three patients were under 30 years old, indicating that although the majority of symptoms develop after the age of 30 years, cerumen discolouration is an early symptom that could have important diagnostic potential.
Nose and throat signs and symptoms are not as well documented. In the case report of the patient presenting with pinna nodules, examination revealed pigmentation of the nasal end of the eustachian tube, and discolouration of the valleculae and pyriform fossae.Reference Sanji, Reddy and Channegowda8 Autopsy studies have shown involvement of the laryngeal cartilages.Reference Helliwell, Gallagher and Ranganath6 In this study, one patient had discolouration of the septal cartilage and another had discolouration of the area adjacent to the apex of the right pyriform fossa.
• Alkaptonuria is a rare inborn error of metabolism
• The majority of patients have ENT manifestations
• Pinna and cerumen discolouration are the most common clinical signs
• Early diagnosis allows patients to be offered potentially disease-modifying therapy
Otological presentation and recognition that leads to early diagnosis (by confirming homogentisic aciduria) is important. Treatment to date has been supportive and palliative. However, nitisinone has the potential to modify the disease by decreasing homogentisic aciduria. It is therefore important to recognise alkaptonuria early so that patients may be offered treatment. Specialist centres, such as the UK National Centre of Alkaptonuria, have the expertise and knowledge to manage alkaptonuria optimally. Early recognition and referral are important for a rare disease such as alkaptonuria.
Conclusion
Despite its rarity, alkaptonuria is a condition that could present to the otolaryngologist. Successful early diagnosis and referral to a specialist centre is essential so that disease-modifying therapy such as nitisinone can be administered. Equally, this allows appropriate investigation and management of the ENT aspects of alkaptonuria.









