Introduction
In the last ten years, Western countries have suffered a number of prominent mass-casualty disasters. Those responding to the terrorist attacks on New York,Reference Simon and Teperman 1 LondonReference Lockey, Mackenzie and Redhead 2 and MadridReference Gómez, Domínguez and Pedrueza 3 reported that communication and information management were key barriers to an effective response. The rapid evolution of mobile technology during the past 10 years offers the potential to address information management in disaster settings through the development of mobile health care technology (mHealth) applications. The World Health Organization defines mHealth as “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices.” 4
The increasing computing power of mobile devices allows the devices to take on new roles in health care, but they have been under-utilized in disaster medicine. Most emergency medical services still rely on paper-based systems.Reference Kindsmüller, Mentler and Herczeg 5 These systems do not scale well to large disasters and can result in lost information.Reference Lenert, Chan and Kirsh 6
To evaluate the further development of mobile technologies for use by frontline health care workers in the care of disaster victims, a literature review was conducted. This paper examines the different types of systems under development, the outcomes from evaluation of these systems, and the lessons that could be applied to future system development.
Methods
Sources of Information
Research on mHealth takes place across a number of disciplines, including medicine, computer science, and interdisciplinary fields such as medical informatics. To capture this diversity, the authors searched multiple databases and other Web-based sources of information. Papers were restricted to those published within the past five years, as the pace of change in mobile technology makes recent research the most relevant.
Search Strategy
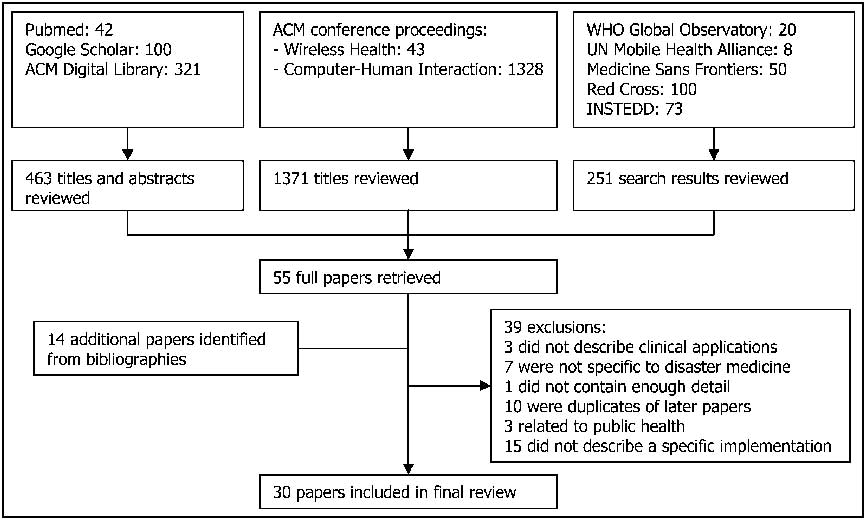
The search strategy is portrayed diagrammatically in Figure 1. Full details of the search terms used are in Table 1. PubMed was searched for papers containing MeSH (the US National Library of Medicine's Medical Subject Headings) terms related to disaster or emergency medicine. To restrict the results to papers relevant to mobile technology, MeSH terms were used for cellular telephones or handheld computers. The following medical informatics journals were searched using PubMed for any papers relating to disaster or emergency medicine:
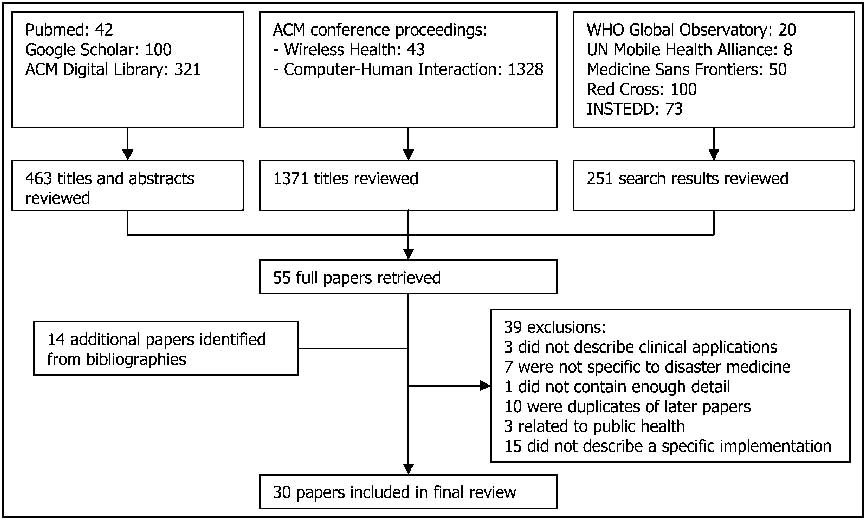
Figure 1 Search Strategy
Table 1 Search Terms
-
• Journal of the American Medical Informatics Association;
-
• International Journal of Medical Informatics; and
-
• Methods of Information in Medicine.
The Association for Computing Machinery (ACM) digital library was searched for keywords relevant to mHealth and disaster medicine to obtain papers from the computer science literature. Papers from recent conference proceedings were also reviewed. Due to the large number of papers in the conference proceedings, initial inclusion was based on title alone.
To ensure that papers from interdisciplinary fields were not missed, Google Scholar was searched for keywords relevant to mobile technology and disaster medicine. The top 100 results (out of 10,600) were reviewed. For each relevant paper, the top 10 “related articles” were checked. Web sites of a number of international organizations involved in disaster relief were also screened for appropriate information.
For each included paper, the bibliography was scanned for references to other relevant papers. Project Web sites, where they existed, were then scanned to find references to more up-to-date papers.
Criteria
Inclusion criteria were as follows:
-
• papers describing a specific implementation of a mobile system for use by health care workers in disaster medicine - either research projects or deployed systems;
-
• papers published in the English language; and
-
• papers published since 2006.
Exclusion criteria were as follows:
-
• papers detailing an early version of a system, when a later paper by the same authors was available;
-
• papers that did not consider clinical applications, such as those discussing only administrative initiatives, communication systems or purely technical aspects;
-
• mobile technologies that were applicable only in a hospital or community environment without being of use in disaster medicine; and
-
• papers that focused on public health (e.g., reporting of infectious disease cases) rather than direct clinical care of disaster victims.
Results
The initial search identified 55 papers. A review of the bibliographies of those papers yielded a further 14 papers. Thirty-nine exclusions were made, leaving 30 papers for the final review (Figure 1).
Most reports described early research or working prototypes; only two referred to systems that had been deployed in actual disasters.Reference Meade and Lam 7 , Reference Levy, Blumberg and Kreiss 8 All projects were based in high-income countries, although some had been tested in low-income countries. Six of the projects were run by the military; the remainder were civilian.
The systems described by the 30 papers reviewed were classified into the five categories described in the following section. For each category, the functions of the system were summarized, the important features of different implementations were compared, and evaluation methods used were discussed. A detailed comparison of features of the individual implementations is given in Table 2. Most systems fall into one of the categories described below, although some systems fit into multiple categories.
Table 2 Comparison of Implementations

Abbreviations: 2G, second generation cell phone network; 3G, third generation cell phone network; 3.5G, High-Speed Downlink Packet Access (HSDPA) cell phone network; CBRN, chemical, biological, radiological, nuclear; Cell phone, cellular phone network of unspecified type; EtCO2, end-tidal CO2; EWS, Early Warning Score; IrDA - short-range infrared communication protocol; Satphone, satellite phone; SMS, short message service (text messages); SpO2, pulse oximetry: temp - body temperature; WiFi, IEEE 802.11 Wireless Local Area Network; WiMAX, IEEE 802.16 long-range Wireless Local Area Network; ZigBee, IEEE 802.15.4 low-rate Wireless Personal Area Networks
Discussion
System Types
Disaster Scene Management
This category includes systems that facilitate triage of patients at a disaster scene and electronically collate data about them. These systems aim to allow the incident manager to allocate resources appropriately and hospitals to be forewarned of the number of patients being sent. These systems are designed to replace the existing paper-based techniques for triaging and collating casualty data.
The key components of these systems are an electronic triage tag attached to each patient, and a communications network to allow the information to be collated. At a minimum, the triage tag needs to hold a unique identifier and current triage status for each patient.Reference Nestler, Artinger and Coskun 9 In some systems, the triage tag stores additional data about the patient until a communication network is available to transmit the data.Reference Inoue, Sonoda and Oka 10 The triage tags may themselves form part of the communication network if they have long-range communication abilities,Reference White 11 or may rely on devices held by the rescuers to transmit their data.Reference Inoue, Sonoda and Oka 10 An alternative approach is to use paper triage tags with barcodes to uniquely identify patients. In this case, all of the data is stored on the rescuers’ handheld devices.Reference Zhao, Rafiq and Hummel 12
The communication networks most commonly used to transfer the data collected are cellular networks or WiFi (wireless local area networks). Cellular networks have the advantage of being widely available in many countries, although they may become congested or damaged during disasters, limiting their usefulness.Reference Nakajima 13 WiFi networks allow a higher data rate and are less vulnerable to damage, but need to be deployed by the rescue team. Buildings or underground areas may cause network blackspots, so systems need to be designed to cope with loss of network connectivity. One way to work around this problem is for the rescuers’ devices to store data and then automatically transmit it when they move into an area with network coverage.Reference Zhao, Rafiq and Hummel 12
To improve the data available to the incident commander, some systems track the geographic location of patients. The Global Positioning System (GPS) is one method for doing this but it does not work well inside buildings.Reference Zhao, Rafiq and Hummel 12 Systems that use WiFi can instead use either the location of the nearest WiFi network nodeReference White 11 or trilateration (calculating position using the distance from multiple nodes).Reference Lenert, Chan and Kirsh 6 , Reference Maglogiannis and Hadjiefthymiades 14 Alternatively, dedicated systems such as ultrasound beacons can be used to determine location.Reference Curtis, Pino and Bailey 15 This works well in hospital settings in which sensors can be prepositioned around the building, but such infrastructure is unlikely to be available at disaster scenes. The positions of patients may be displayed on maps or aerial photographs to allow better visualization of the disaster area. Location trackers may be located both in triage tags attached to patients and in rescuers’ handheld devices,Reference White 11 or solely in the rescuers’ devices.Reference Zhao, Rafiq and Hummel 12 In the latter case, the location of patients is only updated when they come into contact with a rescuer, which could be problematic for ambulatory patients.
Some systems allow transmission of photographs,Reference Abuan 16 live videoReference White 11 , Reference Zhao, Rafiq and Hummel 12 or medical images.Reference Chu and Ganz 17 These may be used for situational awareness, identification of patients or remote diagnosis. Two systems make reference information and guidelines for dealing with hazardous materials available to rescuers.Reference White 11 , Reference Zhao, Rafiq and Hummel 12 Another feature built into some systems is monitoring of patients’ vital signs. This is discussed further in the following section.
Evaluation of these systems is based on exercises with actors playing the roles of patients. None of these systems have been evaluated in an actual disaster.
Telemonitoring
After triage, patients may be left alone for some time. Remote monitoring of their condition allows rescuers to focus on the highest priority patients, while still being alerted to any patients whose condition deteriorates after triage. These systems may relay the raw observations to a central monitoring station, or alternatively provide an automatic mechanism to update the priority of patients depending on their condition. Monitoring devices may also be attached to the rescuers in case they become affected by hazards in the environment.Reference Zhao, Rafiq and Hummel 12
Monitoring devices can be used for monitoring patients at a disaster site, during transfer to hospital or after arrival in hospital. Systems designed for use at a disaster site usually communicate with a base station using shorter-range technologies such as BluetoothReference Chu and Ganz 17 or ZigBee;Reference White 11 the base station then transmits the data to the central server using WiFi or cellular networks.
Systems designed for use during transfer or at a hospital tend to be mobile versions of the normal patient monitoring equipment. As such, they rely on existing communications networks, either cellular (in the ambulance)Reference Chang, Tan and Chen 18 or WiFi networks (in-hospital).Reference Curtis, Pino and Bailey 15 This limits their applicability in disaster scenarios, when cellular networks may be unavailable. However, it offers the advantage that staff are familiar with the systems, as they are routinely used in hospitals and ambulances. One solution to the problem of network availability is to use satellite communications,Reference Nakajima 13 although this is considerably more expensive.
The most common method of monitoring is pulse oximetry,Reference Lenert, Chan and Kirsh 6 , Reference White 11 , Reference Chu and Ganz 17 for monitoring oxygen saturation and pulse rate. Other features that can be monitored include blood pressure,Reference White 11 electrocardiogram (ECG),Reference Chu and Ganz 17 body temperature,Reference Chang, Tan and Chen 18 blood glucose,Reference Kang, Shin and Koo 19 pupil sizeReference Nakajima 13 and end-tidal CO2.Reference Wouhaybi, Yarvis and Muse 20
Most systems use standard touch-screen or keyboard user interfaces, although the use of speech recognition has been tested.Reference Wouhaybi, Yarvis and Muse 20 One system features step-by-step navigation instructions to guide the doctor to the location of the patient who is deteriorating.Reference Maglogiannis and Hadjiefthymiades 14
As these systems can be used in day-to-day hospital or ambulance settings, their evaluation is easier. Most of the systems have been tested on real patients in these settings, but none have been used in a disaster scenario.
Medical Image Transmission
This category of technology involves the remote transmission of images to allow diagnosis by experts who are not at the disaster site. This is sometimes referred to as telemedicine or teleradiology. Telemedicine has historically been conducted over dedicated lines, but newer systems typically use cellular networks to transmit images.
Patient assessment at the disaster scene can be facilitated by the transmission of FAST scans (Focused Assessment with Sonography for Trauma)Reference Blaivas, Adhikari and Shiver 21 and ultrasound scans for identification of traumatic brain injury (imaging of optic nerve sheath diameter and carotid artery Doppler).Reference Ganapathy, Joshi and Yadegar 22 X-ray images can be transmitted from a field hospital for expert assessment.Reference Meade and Lam 7 Dental radiographs can be transmitted for comparison with records held elsewhere to allow identification of the bodies of disaster victims.Reference Salo, Salo and Liisanantti 23
For high-speed transmission, WiMAX networks may be used.Reference Niyato, Hossain and Diamond 24 These are long-range wireless networks (up to 50 km) designed to provide internet access in metropolitan areas, but are not yet widely available.
Initial evaluation of these systems used a lab-based approach to assess the suitability of particular communication technologies for transmitting imaging data. The next step of evaluation was based on transmitting images of healthy volunteers. The final stage is to test the system with real patients, although only one system has been tested in this way.Reference Meade and Lam 7
Decision Support Applications
This category includes applications running on mobile devices to assist health care workers with decision-making in disasters. They are used in the areas of triage, monitoring and hazardous materials to assist rescuers in following predefined algorithms.
Triage applications allow the rescuer to enter the physiological parameters of the patient into a handheld device, which then displays the appropriate triage category.Reference Padmanabhan, Burstein and Churilov 25 , Reference Schell, Wohl and Rathe 26 They can also calculate the Revised Trauma Score, Glasgow Coma Score and Early Warning Score.Reference Sufi, Fang and Cosic 27 These applications replace the paper-based algorithms that would normally be used for this purpose.
Another group of applications provide portable reference information for the identification and treatment of patients affected by Chemical, Biological, Radiological and Nuclear hazards.Reference Schell, Wohl and Rathe 26 , Reference Swain 28 , Reference Williamson 29 This provides individual rescuers with algorithms to identify and treat patients suffering from conditions that would not be encountered in everyday practice.
Most of the applications in this category do not use communication networks to collate the information, so existing paper-based methods would have to be used to accomplish this. One exception is an application for calculation of Early Warning Scores, which includes a facility for transmitting the score to a hospital server using Short Message Service (SMS).Reference Sufi, Fang and Cosic 27
These systems were initially evaluated using lab-based exercises. In these exercises, participants were given written scenarios and asked to use the mobile applications to make decisions such as the appropriate triage category or treatment. Lab-based exercises can give an early indication of usefulness, but do not take into account the problems that are likely to be encountered in a chaotic disaster situation. Evaluation of the tools during disaster exercises allows for usability assessment, but this has only been done for one of the decision support systems.Reference Schell, Wohl and Rathe 26
Field Hospital IT Systems
One paper describes an IT system for a field hospital.Reference Levy, Blumberg and Kreiss 8 Although many elements for this application involve fixed infrastructure, there are mobile elements. A wireless network allows medical staff to access electronic patient records and radiological images using laptops. Patient locations are updated as they move through the different areas of the hospital by scanning barcodes printed on wristbands. This allows the command staff to utilize real-time information on occupancy in different areas of the hospital. Evaluation of this system is based on data gathered during a real deployment.
Evaluation of Systems
Deployment in Disasters
Only two papers describe systems that have been deployed in a disaster. A telemedicine system used by the US military in the response to the 2005 earthquake in Pakistan allowed 44 remote consultations to be carried out with specialists in the US, including three radiology consultations.Reference Meade and Lam 7 A satellite link enabled communications to be set up immediately, although the cost (US $7.00 per minute) was a significant constraint. The satellite link was supplemented by other communication systems once they became available. The telemedicine services were felt to be useful by the clinical staff, who readily accepted the new technology.
A mobile field hospital IT system was deployed by the Israel Defense Force Medical Corps in response to the 2010 Haiti earthquake.Reference Levy, Blumberg and Kreiss 8 The system worked well and helped with efficient management of resources, identification and tracking of patients, continuity of care and effective discharge. The system was reliable and available more than 99.9% of the time. The wireless network was set up within six hours, but was later supplemented by a wired network to improve speed and reduce susceptibility to interference. Laptops were helpful because their battery power allowed continued operation when power failures occurred. A paper-based backup system was used to provide redundancy.
Evaluation of Prototypes
Since only two systems have been deployed, it is not possible to provide a comprehensive review of how mobile technology performs in real disasters. Evaluations of prototypes allow lessons to be drawn that will be relevant in the development of future systems. The outcomes measured in different evaluations vary too much to allow meta-analysis, but it is possible to draw some conclusions about the benefits of using electronic systems. Probability values (P values) are stated below where they are available in the original papers.
Using mHealth makes a small difference to the speed of the triage process. Three studies comparing paper-based to electronic triage found the electronic system to be slightly faster:
-
• 42 seconds per patient for paper triage vs. 38 seconds for electronic;Reference Inoue, Sonoda and Oka 10
-
• 36.6 minutes for paper triage of all patients in a 40-casualty incident vs. 34.7 minutes using electronic triage, P = .0008;Reference Schell, Wohl and Rathe 26
-
• 5 minutes per patient for triage and data entry using paper vs. 3.4 minutes using electronic triage.Reference Zhao, Rafiq and Hummel 12
One study found that a lack of familiarity with equipment can lead to increased triage times (19 seconds per patient using paper triage vs. 25.9 seconds using electronic triage).Reference Nestler, Artinger and Coskun 9
When considering the flow of patients throughout the whole disaster site, the benefits are clearer. Eliminating the need to track patients manually decreases the time required to transport all patients to treatment areas (41 minutes for 62 patients using paper triage vs. 23 minutes using electronic).Reference Inoue, Sonoda and Oka 10 Patients can leave the disaster site more quickly due to automatic allocation of ambulances (56 minutes for 66 patients using paper triage vs. 42 minutes using electronic).Reference Inoue, Sonoda and Oka 10 The average time individual patients spend in the treatment area is reduced with electronic triage (47 minutes average time in treatment area for walking wounded with paper triage vs. 38 minutes with electronic; 24 minutes with paper triage vs. 18 minutes with paper triage for seriously wounded).Reference Lenert, Chan and Kirsh 6 One reported problem with electronic tags that may slow the triage process is that triage status cannot be seen at a glance, unlike colored paper tags.Reference Jokela 30
Electronic triage improves the quality of care received by patients. Accuracy of triage increases (53% with paper vs. 67% with electronic triage in one study; composite score of 48.1 with paper vs. 53.4 with electronic, P = .02 in another).Reference Padmanabhan, Burstein and Churilov 25 , Reference Schell, Wohl and Rathe 26 Completeness of patient information increases (34% with paper triage vs. 71% with electronic).Reference Lenert, Chan and Kirsh 6 Serious errors such as losing track of patients and errors in patient identification are eliminated with the use of electronic triage (from 6% with paper to 0% and from 20% with paper to 0% respectively).Reference Lenert, Chan and Kirsh 6 Rapid arrival of groups of patients causes less degradation in the ability of responders to record patient data.Reference Lenert, Chan and Kirsh 6 Patients can be reassessed more frequently with electronic triage (from 2.9 to 7.8 times during the course of an exercise),Reference White 11 allowing deteriorating patients to be spotted quickly. Information about triage classifications is available to incident commanders 47 minutes earlier,Reference Jokela 30 allowing resources to be allocated more efficiently. Subjectively, rescuers believed that electronic triage systems improved efficiencyReference Jokela 30 and patients perceived monitoring systems as useful.Reference Curtis, Pino and Bailey 15
Electronic disaster scene management systems streamline communication. The need for radio and telephone conversations is reduced (from 55 to 30 conversations over a two-hour period).Reference White 11 , Reference Lenert, Chan and Kirsh 6 A reliance on wireless communications can be problematic due to high levels of electromagnetic noise in disaster zones. Helicopters with microwave video transmission capabilities and fire engines are notable sources of interference.Reference Lenert, Chan and Kirsh 6 Mesh networks, which allow each node (such as a rescuer's handheld device) to relay information from other nodes, provide resilience against the loss of communications links.Reference Lenert, Chan and Kirsh 6 Decentralized grid computing, which distributes the processing among multiple computers at different locations, is necessary to cope with the volume of data produced by monitoring devices in large-scale disasters involving thousands of patients.Reference Sufi, Khalil and Cosic 31
Evaluations have shown that it is possible to transmit radiological images to remote locations. FAST scans can be successfully transmitted over cellular networks and the results can be interpreted remotely with confidence.Reference Blaivas, Adhikari and Shiver 21 X-ray images can be transmitted over cellular networks.Reference Maglogiannis and Hadjiefthymiades 14 Cellular networks are fast enough for this purpose: an X-ray image (at a resolution of 4 megapixels) can be transmitted in one minute and a FAST scan in under two minutes.Reference Maglogiannis and Hadjiefthymiades 14 For areas where cellular signals are unavailable, satellite links may be used for transmitting X-rays, although these are very slow.Reference Meade and Lam 7 There have been no reported exercises to assess the difference that the availability of these images would make to clinical outcomes, and the level of training required to acquire good-quality images may limit the applicability of these technologies.
Lessons Learned
Equipment trials highlighted a number of issues. While many systems used off-the-shelf components, field tests showed that off-the-shelf handheld devices are not durable enough for use in disaster zones.Reference Abuan 16 , Reference Jokela 30 The limited battery life of handheld devices is a key constraint, with lifetimes of between 20 minutesReference Abuan 16 and 3.5 hoursReference Zhao, Rafiq and Hummel 12 reported. Bulky equipment may interfere with carrying patients.Reference Walderhaug, Meland and Mikalsen 32 Data input into portable devices may be difficult while wearing examination gloves,Reference Walderhaug, Meland and Mikalsen 32 although it is possible to design stylus-based input devices that can be used while wearing hazmat suits.Reference Zhao, Rafiq and Hummel 12 The use of speech recognition to control telemedicine systems is problematic because users’ speaking styles change when they are in an emergency situation.Reference Wouhaybi, Yarvis and Muse 20 No cost-benefit analyses were found, but the cost of new equipment is likely to be a barrier to uptake.Reference Jokela 30
Lack of familiarity with complicated equipment is a serious problem. Mass-casualty incidents are rare for an individual responder, and technologies must be used every day if they are to be successfully used in a disaster.Reference White 11 Most evaluation exercises are carried out immediately after training, and so do not take into account the deterioration of skills that is likely to occur between training and use. A possible solution to this is to integrate disaster systems with those used in the daily working environment.Reference Kindsmüller, Mentler and Herczeg 5 , Reference Curtis, Pino and Bailey 15 Rescuers do not trust new technology unless they have extended training and testing.Reference White 11 They report that they do not like the feeling that they are “being watched” by the technology.Reference White 11 This is reflected in the fact that the new technology is more popular with incident commanders than first responders.Reference White 11 A key theme that emerges is that end users of the technology must be involved throughout the development process.Reference Nestler, Artinger and Coskun 9 , Reference White 11
Limitations
This literature review covers a number of fields. The search strategy, which included conference proceedings and other unpublished work, aimed to identify as many relevant papers across the breadth of disciplines as possible, yet some papers may have been missed. Nonetheless, the range of systems described covers the variety of clinical applications that would be expected in this area, and therefore offers insight into mHealth in disaster medicine.
To give a clear picture of the range of available technologies, it was necessary to include all papers found in the search without making exclusions based on quality. Many papers did not give sufficient information to allow the reader to judge whether the proposed technology offered any clinical benefit. Most papers lacked a full description of the statistical analysis done. Few of the papers attempted to blind the comparison of systems, raising the possibility of observer bias. The large number of positive results raises the possibility of publication bias.
Conclusions
This review identified five categories of mobile technology systems for use in disaster medicine. Of these, only field hospital IT systems and teleradiology systems have been deployed in real disasters. Evaluations of prototype systems suggest that electronic triage and decision support systems should allow faster processing and transport of patients, along with improved accuracy of triage. Systems for monitoring unattended patients should allow deterioration to be spotted. Teleradiology technology should allow experts situated away from the disaster area to assist in the diagnosis of traumatic injuries. However, these benefits have yet to be proven in practice and there are concerns about the increased cost of equipment and extra training required.
Most of the research and evaluation in this field has taken place in high-income countries. The mobile nature of the technology should allow it to be deployed in other parts of the world. The minimum requirements of access to electricity and a cellular network can be met in most countries, with cellular networks now covering 90% of the world's population. 35 All the categories of technology should be applicable in low-income countries, with telemedicine systems perhaps the most useful due to large distances between hospitals. For long-term deployments in low-income countries, access to the necessary supplies for maintaining equipment may be difficult, particularly if equipment failures increase in deployments to areas with hostile climates.
This review shows that mHealth can have a range of applications in disaster medicine, but there is not yet enough evidence on its impact. Future research should aim to provide robust, unbiased evidence of the benefits of mobile technology, while addressing the shortcomings that have been identified in previous projects. This will enable the widespread deployment of these systems so that in future disasters, resources can be optimally deployed to save lives.
Abbreviations
- FAST:
-
Focused Assessment with Sonography for Trauma
- GPS:
-
global positioning system
- IT:
-
information technology
- mHealth:
-
mobile health care technology