Introduction
Endoscopic sinus surgery and skull base surgery have evolved dramatically since they were popularised by Walter Messerklinger and David Kennedy in the late 1970s, owing particularly to the development of the rigid Hopkins rod endoscope and bespoke instruments. Over the subsequent 40 years, endoscopic endonasal surgery has developed to allow treatment of complex neurosurgical, craniofacial and skull base lesions that would otherwise require extensive open-approach surgery for access.
Topical and injected local anaesthetic techniques in nasal surgery are well established, developing from the historical use of cocaine (2–3 mg/kg), which is both a potent vasoconstrictor and anaesthetic agent.Reference Campbell, Cherri, Warren, Prazma and Pillsbury1 Injected local anaesthetic preparations of lidocaine are typically combined with adrenaline to offer a short acting anaesthetic effect with simultaneous vasoconstriction and higher dose toxicity (7 mg/kg) because plain local anaesthetic would result in vasodilatation and a significantly lower limit of dose toxicity (3 mg/kg). Longer acting agents like levobupivacaine do not confer an advantage with regards to dose toxicity despite being available in preparations combined with adrenaline.Reference Friedman, Venkatesan, Lang and Caldarelli2
This contemporary review of local anaesthetic techniques, focusing on the use of lidocaine with adrenaline as an injectable block, is specifically directed towards endonasal surgery and emphasises the potential role in endoscopic sinus surgery using local anaesthetic midfacial nerve blocks. A review of the contemporary literature and combination of modified dental techniques and intraoral anatomy is combined with in vivo surgical experience to provide an up-to-date guide for the endoscopic sinus surgeon wishing to perform surgery on suitable patients.
Materials and methods
Relevant anatomy
The nasal cavity is innervated by four systems: sensory, motor, autonomic and parasympathetic. Although a large number of nerves contribute to the sensory supply of the nasal cavity, they predominately originate from the ophthalmic (V1) and maxillary (V2) division of the trigeminal nerve. The ophthalmic division exits the skull via the superior orbital fissure, providing sensation to structures derived from the frontonasal prominence via three main branches (Table 1). The majority of sensory innervation to the nasal cavity is supplied by the maxillary division (Figure 1). It emerges from foramen rotundum and innervates structures derived from maxillary prominence of the first pharyngeal arch via nine sensory branches (Table 1). Key areas manipulated during endoscopic sinus surgery include the sinuses, nasal vestibule, columella, lobule, nasal septum and the turbinates (Table 2). Good understanding of pertinent local innervation is essential to enable effective local anaesthetic surgery.

Fig. 1. Schematic diagram of sensory innervation of the nasal cavity.
Table 1. Sensory branches of the trigeminal nerve

Table 2. Sensory innervation of the nasal cavity

The sensory branches of V2 (Table 3) which supply the nasal cavity can be effectively reached via the pterygopalatine ganglion, situated within the pterygopalatine fossa. This small-volume, cone-shaped space is located between the maxilla, sphenoid and palatine bone. It has seven foramina (Table 4), the most clinically relevant of which include the sphenopalatine foramen, the greater palatine foramen and the pterygomaxillary fissure.
Table 3. Boundaries of the pterygopalatine fossa

Table 4. Foramina of the pterygopalatine fossa

The sphenopalatine foramen is located at the junction between the palatine bone and the sphenoid bone. The cristae ethmoidalis protects this foramen and forms a consistent feature in the unoperated patient. Typically, the sphenopalatine foramen is found just posterior to the maxillary antrum, at the posterolateral edge of the middle turbinate between the middle and superior meatus (Figure 2). This conduit transmits the nasopalatine nerve, posterior superior nasal nerve and the sphenopalatine artery and vein.
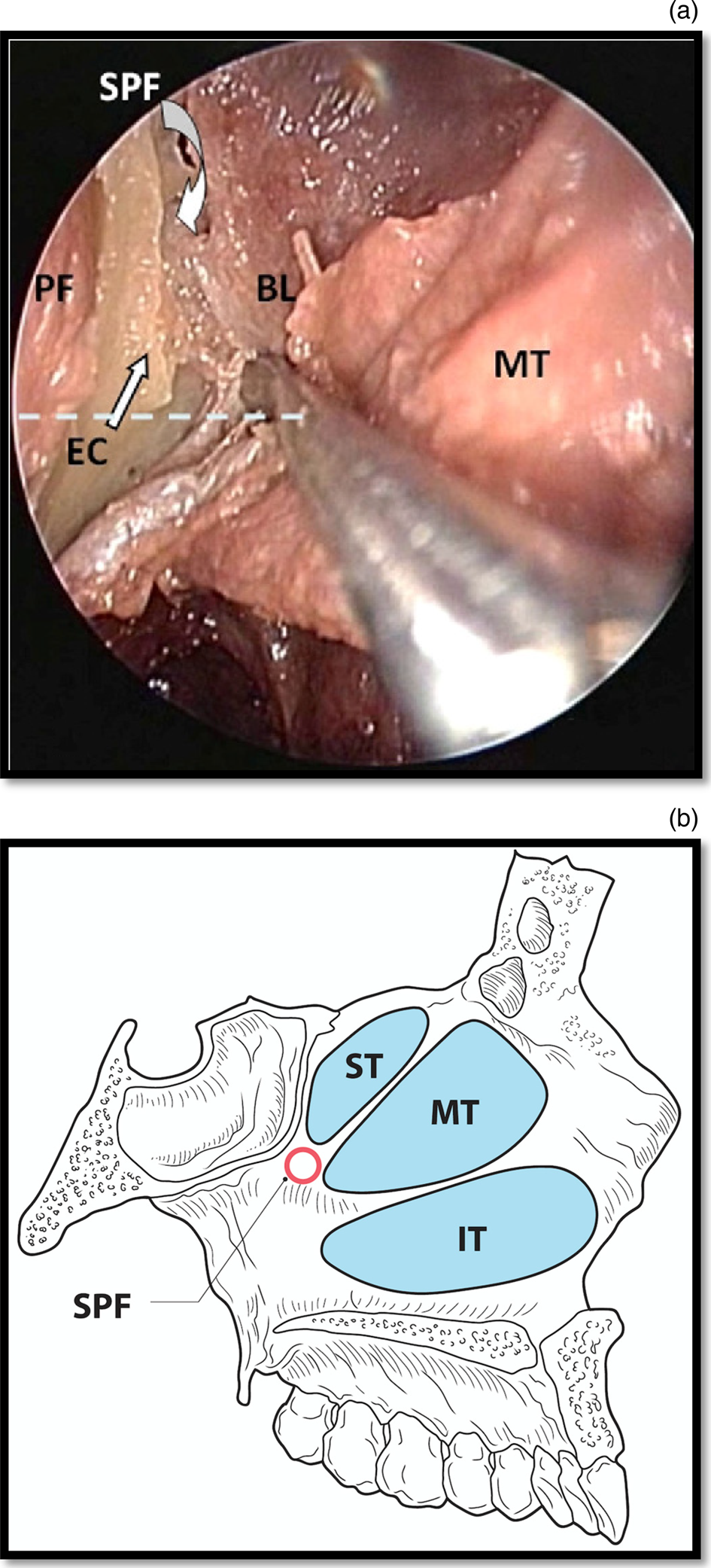
Fig. 2. (a) Endoscopic view of the right sphenopalatine foramen and (b) schematic diagram showing the anatomy of the sphenopalatine foramen. SPF = sphenopalatine foramen; PF = posterior fontanelle; BL = basal lamina; MT = middle turbinate; EC = ethmoid crest; ST = superior turbinate; IT = inferior turbinate
The greater palatine foramen is situated along the posterior aspect of the hard palate of the greater palatine canal, formed between the articulation of the maxillary bone and the palatine bone. Clinically, it is identified between the second and third molars approximately one centimetre towards the midline of the palate from the gingival margin (Figure 3). It transmits the descending palatine vessels and greater palatine nerve.

Fig. 3. Schematic diagram demonstrating the greater palatine foramen.
Finally, the pterygomaxillary fissure is the narrow gap between the infratemporal surface of the maxilla and the lateral pterygoid plate (Figure 4). Located posterior, superior and medial to the maxillary tuberosity, it connects the pterygopalatine fossa with the infratemporal fossa and transmits the terminal part of the maxillary artery and the posterior superior alveolar nerve.
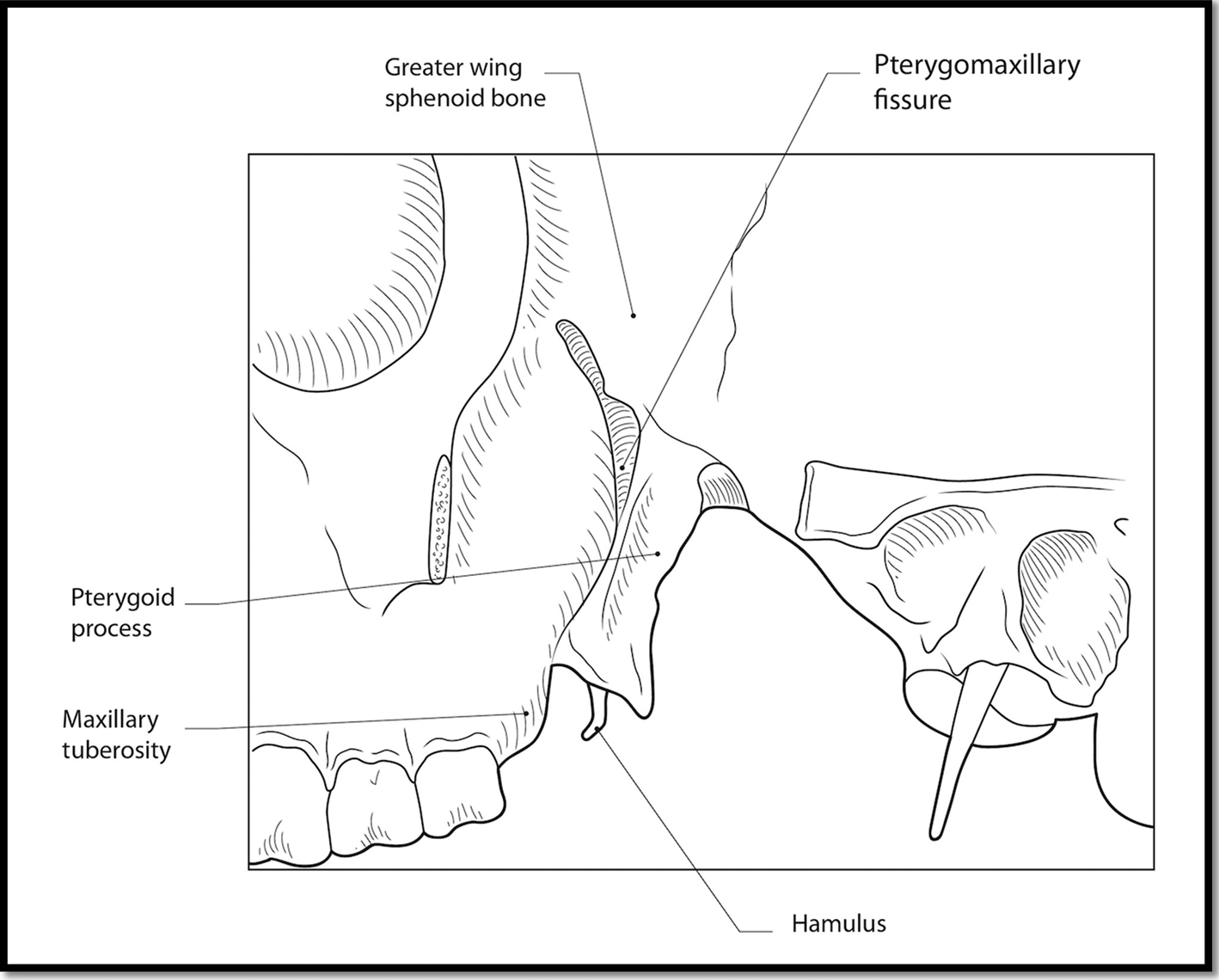
Fig. 4. Schematic diagram demonstrating the pterygomaxillary fissure.
Patient selection
Patient selection is a vital aspect of successful local anaesthetic endoscopic sinus surgery and pre-operative assessment may form an unwitting part of the consultation. Patients who are stoical and have had previous procedures performed under sedation or local anaesthetic may better tolerate local anaesthetic endoscopic sinus surgery. Similarly, those who are tolerant of dental procedures may be familiar with the anaesthetised mid-face and may tolerate local anaesthetic endoscopic sinus surgery better than those who are dentally and surgically naive. Patients tolerating endoscopic assessment during out-patient clinic may be more co-operative during local anaesthetic endoscopic sinus surgery, particularly when inspecting sensitive areas such as the middle meatus. Local anaesthetic endoscopic sinus surgery may be of particular worth in patients with multiple cardiorespiratory comorbidities who are deemed unfit for general anaesthetic. Simultaneous electrocardiogram and oxygen saturation monitoring is recommended throughout.
The authors recommend initial use of 4.4 ml Lignospan® (2 per cent lidocaine +1:80 000 adrenaline) applied endonasally on neuropatties. This permits mucosal anaesthesia and decongestion, meaning subsequent instrumentation is less stimulating in the event of a partial or non-functional block. Next, a dental syringe is loaded with Lignospan. These cartridges have the advantage of being self-aspirating by virtue of the elastic recoil of the rubber end piece; when pressure is removed from the plunger, the cartridge will aspirate. A variety of gauges and lengths are available for dental anaesthetic needles; however, most authorities recommend a 27-gauge needle in order to reduce the risk of non-aspiration.Reference Meechan, Czachur, McCabe and Blair3 The preferred local anaesthetic blocks of the individual authors are described below.
Results
Nasopalatine foramen block
Anatomy
The incisive nerve is the terminal branch of the nasopalatine nerve which receives its name as it emerges from the incisive foramen. It communicates with the anterior palatine nerve and supplies sensation to the upper incisors, adjacent gingivae, anterior palate and pre-maxilla as well as the surrounding mucosa.
Technique
The incisive papilla is the pear-shaped, midline mucosal fold situated on the palatal surface between the central incisors.Reference Solomon and Arunachalam4 This should be compressed using a cotton swab and then a 27 G short dental needle should be inserted just lateral to the papilla at 45 degrees. Local anaesthetic solution should be deposited slowly until the needle has penetrated approximately 5 mm, directly over the nasopalatine foramen. A small volume of less than 0.5 ml is usually enough to anaesthetise this area. Once blanching has been observed independent of that produced by direct pressure from the cotton swab, this volume of infiltration would be deemed sufficient (Figure 5).
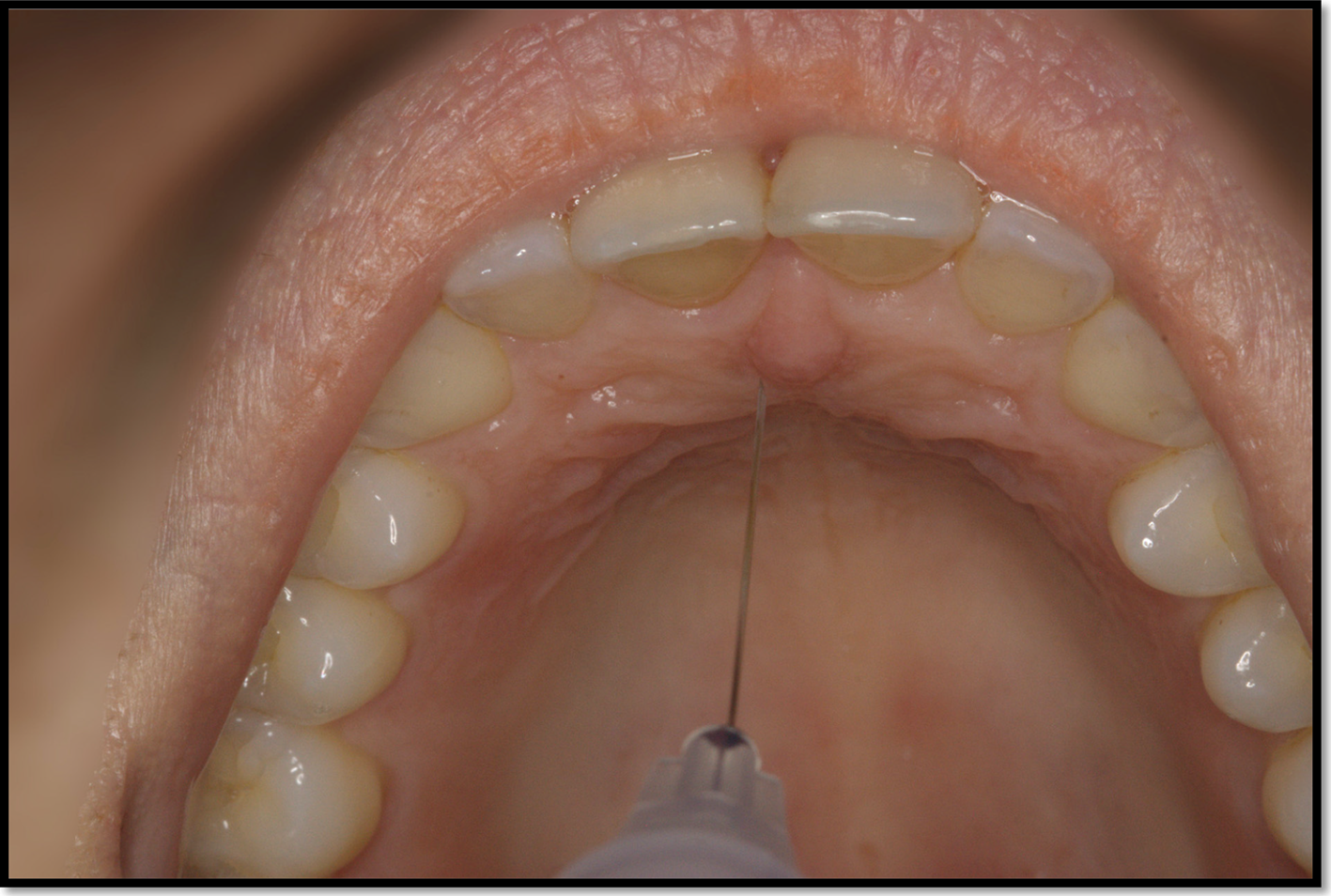
Fig. 5. Image showing nasopalatine foramen block.
Sphenopalatine ganglion block (endonasal)
Anatomy
The sphenopalatine nerve and artery emerge from the sphenopalatine foramen. Endoscopically this can be located during sphenopalatine artery ligation by elevating the middle meatal mucosa at the posterior fontanelle until the crista ethmoidalis is identified, behind which the vessels emerge. The posterior end of the middle turbinate is therefore a useful endoscopic landmark in identifying the mucosal region in which the nerve emerges. The natural ostium of the maxillary sinus may also serve as a landmark as the maxillary artery can be located in the posterior maxillary sinus wall endoscopically and traced medially to identify the level of the sphenopalatine foramen and artery.
Technique
Under endoscopic guidance, the middle turbinate is carefully medialised in order to visualise the posterior attachment of the middle turbinate at the lateral nasal wall. A spinal needle can be attached to a 2 ml Luer lock syringe and carefully introduced into the middle meatus to inject into the area described, placing the sphenopalatine artery into vasospasm as well as anaesthetising the septum, inferior and middle turbinates, anterior face of the sphenoid, and nasal floor.
Maxillary nerve block via greater palatine foramen
Anatomy
The greater palatine foramen transmits the greater palatine branches of the sphenopalatine nerve to supply the bony and mucosal structures of the hard palate excluding the incisors and pre-maxilla. The upper teeth are supplied by the superior alveolar nerve and are not supplied by the greater palatine nerve. More proximally, the foramen communicates with the pterygopalatine fossa and pterygomaxillary fissure, where the maxillary nerve gives off the pterygopalatine nerve. The greater palatine foramen and canal are utilised in this block for retrograde injection resulting in a more proximal block, the effects of which can be assessed by asking about hard palatal sensation.
By comparison, the nearby lesser palatal foramen transmits the lesser palatine nerves which supply the soft palate, uvula and the majority of the tonsillar fossa above the tongue base, so an inadvertent block here results in diminished oropharyngeal and velopharyngeal sensation but with preservation of the gag reflex.
Technique
A 27-gauge needle is inserted perpendicular to the mucosa, 1 cm medial to the upper second molar. A cotton bud may aid identification of the greater palatine foramen. The swab will sink slightly into the depression of the foramen, enabling firm pressure to be applied. This pressure anaesthesia helps reduce the pain of injection.Reference Malamed5 The needle should be directed slightly superolaterally to follow the canal for at least 10 mm before injecting local anaesthetic to ensure penetration into the pterygopalatine foramen. This will block the greater palatine nerve as it enters the greater palatine foramen (Figure 6).
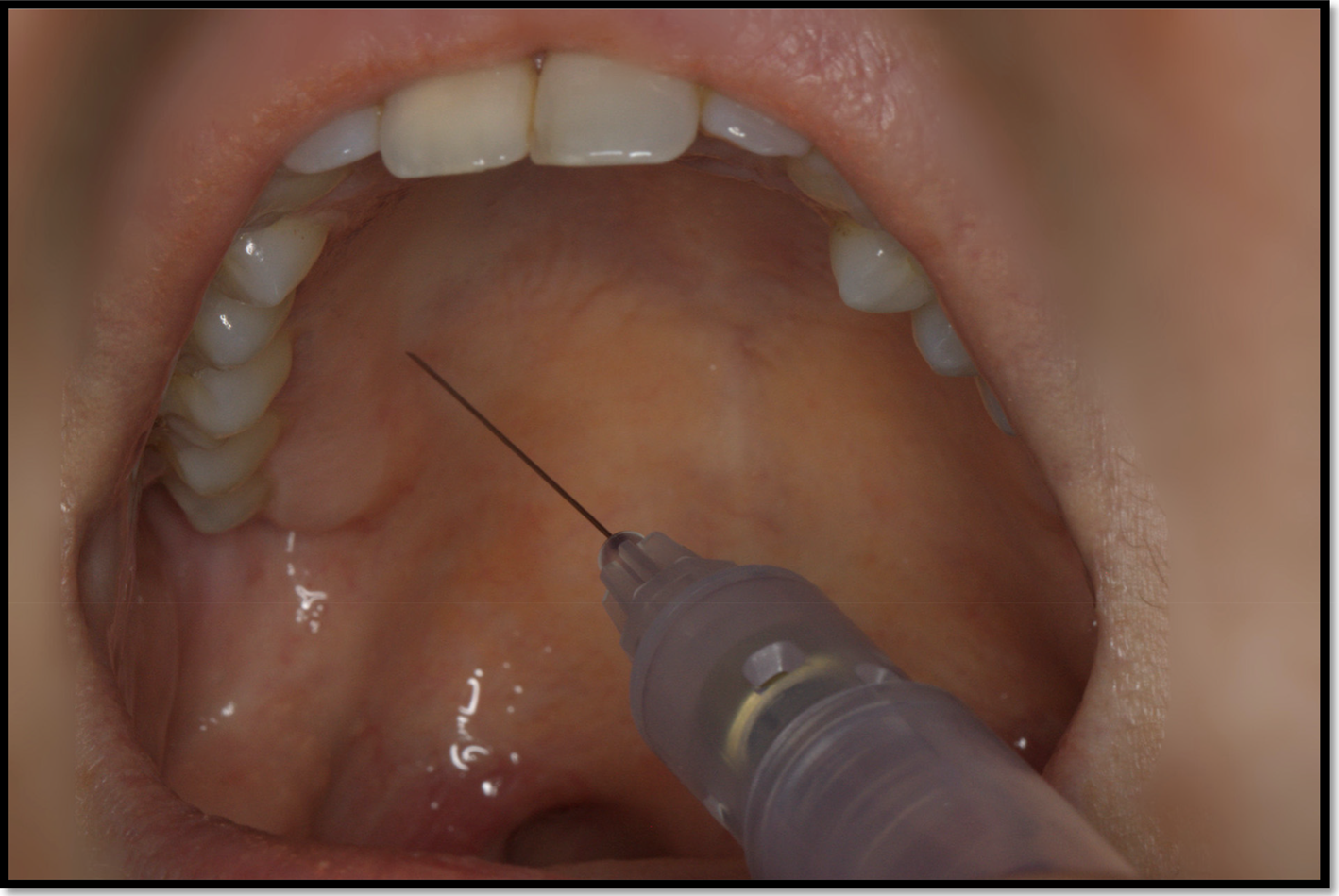
Fig. 6. Maxillary nerve block showing greater palatine foramen approach.
Maxillary nerve block via transoral lateral pterygoid plate
Technique
Close assessment of the intra-oral anatomy is pivotal as this block is relatively deep and therefore blind. Ultrasound guidance has been described in cadaveric studies but is not utilised by the authors.Reference Kampitak, Tansatit and Shibata6
Palpation of the hamulus identifies the anterior-most extent of the lateral pterygoid plate. A 27-gauge, 35 mm dental needle is angled at 45 degrees prior to infiltration. The cheek is laterally retracted, and the patient encouraged to relax the mouth enough to create some mucosal slack, improving access to the buccal sulcus. The needle is inserted lateral to the hamulus in the deepest aspect of the posterosuperior buccal sulcus, aiming to infiltrate in a plane parallel to the lateral pterygoid plate. The pupil can be used as a surface landmark for the maxillary nerve and foramen rotundum. The needle should be inserted to the hilt to allow it to reach as close to the pterygopalatine fossa as possible. The resulting block provides entire midfacial anaesthesia and places the maxillary artery into vasospasm. This can occasionally cause midfacial blanching which is reversible (Figure 7).
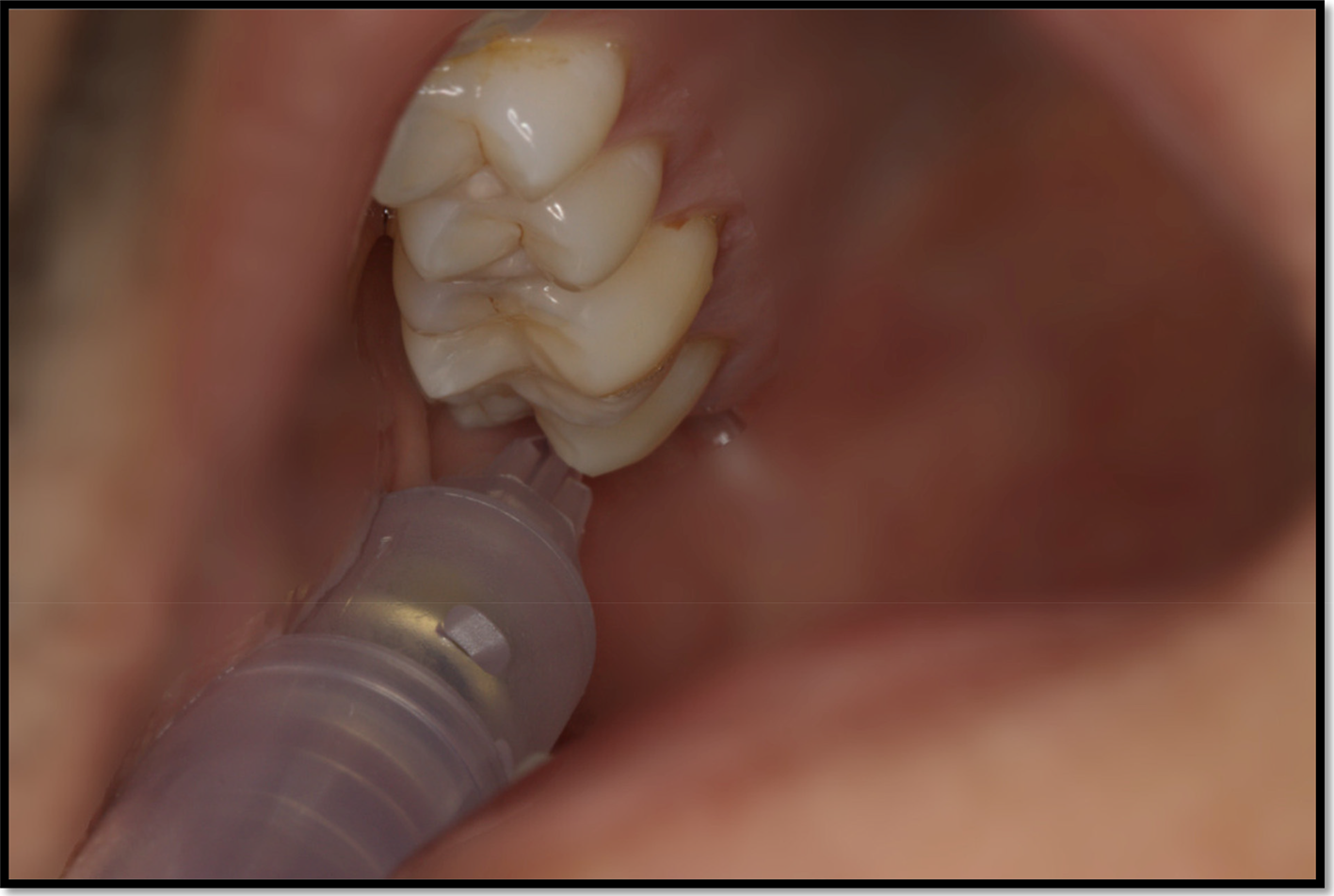
Fig. 7. Maxillary nerve block showing transoral lateral pterygoid plate approach
Discussion
Endoscopic sinonasal surgery is indispensable in managing a spectrum of conditions from intractable rhinosinusitis to complex neurosurgical pathology.Reference Dalziel, Stein, Round, Garside and Royle7 Originally, this procedure was performed under topical local anaesthesia but was typically limited to nasal polypectomy and septal surgery, leaving remaining nasal anatomy largely intact. Evolving surgical techniques permitted more extensive resection, necessitating general anaesthetic to achieve adequate airway protection, immobilise the surgical field and maximise patient comfort.Reference Lee, Kapur and Ramsden8 However, increasingly comorbid and ageing populations have more systemic risks of general anaesthesia such as myocardial infarction,Reference Devereaux, Xavier, Pogue, Guyatt, Sigamani and Garutti9 venous thromboembolism,Reference Pannucci, Bailey, Dreszer, Fisher Wachtman, Zumsteg and Jaber10 aspirationReference Cook, Woodall and Frerk11 and delirium.Reference Strom, Rasmussen and Sieber12 Local anaesthetic endoscopic sinus surgery may be of particular worth in patients with multiple cardiorespiratory comorbidities who are not fit for general anaesthetic and would otherwise be denied a surgical management option.
Endotracheal intubation itself is not without complication, ranging from a mild sore throat,Reference McHardy and Chung13 minor bleedingReference Kalingarayar, Nandhakumar, Subramanian and Namboothiri14 and dental damageReference Vogel, Stubinger, Kaufmann, Krastl and Filippi15 to laryngotracheal injuryReference Mota, de Cavalho and Brito16 and pneumothoraces.Reference Berg, Mafee, Campos and Applebaum17 Moreover, direct laryngeal stimulation during endotracheal intubation promotes a sympathetic response contributing to haemodynamic instability.Reference Stoelting18 Thus, the principle advantage of local anaesthetic techniques is in enabling substantive surgery to be performed without positive pressure ventilation or airway instrumentation as the patient maintains their own airway.Reference Jourdy and Kacker19
The increasing prevalence of congestive cardiac failureReference Roger20 and obesityReference Davies21 has consequently increased rates of orthopnoea, rendering many patients physiologically unable to lie flat for procedures. Non-intubated patients can be positioned more upright; for example, the reverse Trendelenburg position provides 15° of head elevation.Reference Gan, Habib, Rajwani and Javer22,Reference Ghanem and Elmalt23 This increases venous drainage of the head and neck as blood pools in the lower extremities.Reference Knight and Mahajan24 Every 2.5 cm elevation above the level of the heart corresponds with a 2 mmHg reduction in mean arterial blood pressure.Reference Enderby25 Accordingly, more upright positioning together with the vasoconstrictive properties of local anaesthetic improves the surgical view.Reference Hathorn, Habib, Manji and Javer26 In turn, this reduces operative time by decreasing rod cleaning and suctioning.Reference Lee, Kapur and Ramsden8
Adverse events in endonasal sinus surgery remain rare, but significant,Reference Krings, Kallogjeri, Wineland, Nepple, Piccirillo and Getz27 including cerebrospinal fluid leak, haemorrhage, orbital trauma, epiphora, optic nerve damage and meningitis.Reference Cumberworth, Sudderick and Mackay28 Under local anaesthesia, patients remain conscious throughout and are therefore able to signal any pain or discomfort, which theoretically minimises complications like orbital breach.Reference Lee, Kapur and Ramsden8,Reference Jourdy and Kacker19,Reference Fedok, Ferraro, Kingsley and Fornadley29 However, local anaesthetic endoscopic sinus surgery does not universally reduce the risk of intra-operative complications.Reference Hosemann and Draf30
Vascular supply to the nasal cavities is extensive and anastomotic. Haemorrhage substantially disrupts visibility during endoscopic sinus surgery,Reference Milonski, Zielinska-Blizniewska, Golusinski, Urbaniak, Sobanski and Olszewski31 potentiating the risk of orbital, vascular or intracranial damage.Reference Tan and Poopalalingam32 Hypotension is deliberately achieved during general anaesthetic. The mean arterial blood pressure is loweredReference Simpson33 in order to reduce intra-operative blood loss by up to 141 ml,Reference Elsharnouby and Elsharnouby34 thereby improving the surgical visual field.Reference Wormald, Athanasiadis, Rees and Robinson35 Although rare, intentional hypotension is not without consequence and theoretically may engender cerebral thrombosis, renal hypoperfusion and myocardial infarction.Reference Ghanem and Elmalt23,Reference Choi and Samman36,Reference Nishimura, Suzuki, Hatazawa, Nishimura, Shirane and Yasui37 The techniques outlined in this paper recommend the initial use of Lignospan (2 per cent lidocaine + 1:80 000 adrenaline). In addition to providing topical anaesthesia, this decongestant acts as a potent vasoconstrictor which aids mucosal decongestion and reduces haemorrhage, mitigating the hypotensive benefits seen in general anaesthesia.Reference Yang, Li, Jil, Wang, Sun and Wang38 Caution must be exercised as systemic absorption can result in hypotension,Reference Yang, Wang, Wang, Sun, Wang and Zuo39–Reference Phillips, Hutchinson, Bayly and Hollway41 hypertension,Reference Tanaka and Nishikawa42 tachycardiaReference Yang, Li, Jil, Wang, Sun and Wang38 and arrythmiasReference Thomas, Behbehani, Coyle and Denson43,Reference Sia, Sarro, Lepri and Bartoli44 depending on the anaesthetic agent selected. However, Cohen-Kerem et al.Reference Cohen-Kerem, Brown, Villasenor and Witterick45 demonstrated systemic absorption to be rare, and haemodynamic observations remained within normal range. Furthermore, although adrenaline theoretically reduces tissue perfusion,Reference Wilhelmi, Blackwell, Miller, Mancoll, Dardano and Tran46 the study by Hafner et al. of 10 000 patients undergoing ear and nasal surgery reported no cases of tissue necrosis.Reference Hafner, Rocken and Breuninger47 Procedures performed under local anaesthetic may induce fear, stress and pain, with consequent catecholamine release.Reference Guimaraes, Lopes Motta, Bergamaschi, Araújo, Andrade and Figueiró48 In turn, systemic stress hormones can cause hypertension and arrhythmias.Reference Godzieba, Smektała, Jedrzejewski and Sporniak-Tutak49,Reference Meyer50
In addition to providing nasal anaesthesia, local vasoconstriction, mucosal decongestion and enhanced haemostasis, endonasal surgery performed under local anaesthetic permits early patient mobilisation and long-lasting post-operative analgesia.Reference Yang, Li, Jil, Wang, Sun and Wang38,Reference Caner, Olgun, Gultekin and Aydar51–Reference Lee, Yoo, Yon, Kim, Kim and Lee53 The initial discomfort associated with local anaesthetic blocks in the awake patient can be mitigated through slow infiltration and use of a fine 27-gauge needle.Reference Jourdy and Kacker19,Reference Metzinger, Bailey, Boyce and Lyons54 Procedures performed under local anaesthetic permit shorter total operative and recovery timesReference Jourdy and Kacker19,Reference Ghanem and Elmalt23 and help release anaesthetic capacity for other operating theatres.Reference Caner, Olgun, Gultekin and Aydar51 Fedok et al.Reference Fedok, Ferraro, Kingsley and Fornadley29 reported local anaesthetic procedures reduced total operative time by up to 22 per cent when compared with general anaesthetic. This was particularly noted for shorter, less extensive procedures (such as anterior ethmoid and maxillary sinus surgery), where the anaesthetic component forms a larger proportion of the total operative time. Although the absolute time saved was only 17.5 minutes, cumulative benefit by process of marginal gains may confer practical, clinical significance.
Overall, the substantial reduction in recovery time for local anaesthetic procedures proves more critical to patient flow and hospital efficiency than the slight reduction in operative duration. Patients recovering from general anaesthetic require higher-intensity, first-stage recovery which is more expensive and labour intensive. Faster recovery combined with reduced admission rate and lack of anaesthetist therefore reduces the procedure costs of local anaesthetic.Reference Jourdy and Kacker19,Reference Ghanem and Elmalt23 Patient preference is perhaps even more important; Caner et al. found 89 per cent of patients would choose to reselect future procedures to be performed under local anaesthetic.Reference Caner, Olgun, Gultekin and Aydar51 A dedicated time-and-motion study looking at local anaesthetic endoscopic sinus surgery may help quantify the relative cost-benefits over and above operating under sedation or general anaesthetic.
Endoscopic sinonasal surgery performed under local anaesthetic presents surgical challenges for analgesia, airway protection and immobilisation. Total nociceptive anaesthesia requires good knowledge of local anatomy, and some advocate the use of titrated sedation (such as midazolam, fentanyl, remifentanil or propofol infusion).Reference Lee, Kapur and Ramsden8,Reference Fedok, Ferraro, Kingsley and Fornadley29,Reference Buyukkocak, Ozcan, Daphan, Apan and Koc55,Reference Scamman, Klein and Choi56 When used, sedation does provide the advantage of retrograde amnesia.Reference Lee, Kapur and Ramsden8 However, caution should be advised as this experience can be disorientating and requires a dedicated sedation-trained healthcare professional. Airway evaluation must be scrupulous if sedation is planned, especially if an anaesthetist will not be present. Indeed, some endoscopic procedures performed under sedation have reported fatalities.Reference Thompson, Wright, Murray, Ritchie, Burton and Stonebridge57
Other papers describing local anaesthetic techniques for endonasal surgery focus predominantly on topical mucosal anaesthesia, as opposed to regional nerve blockade, to achieve nasal anaesthesia. For example, Lee et al.Reference Lee, Kapur and Ramsden8 describe topical application of 25 per cent cocaine paste to progressively anaesthetise nasal mucosa. Although topical anaesthesia permits some endonasal procedures, including uncinectomy and exploration of sphenoid sinuses, it does not offer the formal regional block, as described in this paper. A variety of studies have assessed the role of local anaesthetic blocks with concomitant general anaesthesia.Reference Cho, Drover, Nekhendzy, Butwick, Collins and Hwang58–61 For example, Shamil et al.Reference Shamil, Rouhani, Basetti, Bast, Hopkins and Surda62 demonstrated a statistically significant reduction in post-operative pain following anterior ethmoidal and sphenopalatine ganglion blocks with 0.5 per cent Bupivicaine and 1:200 000 adrenaline. Crucially, all patients underwent general anaesthetic prior to endoscopic sinus surgery. Techniques outlined for the sphenopalatine ganglion block reflect our maxillary nerve block via the greater palatine foramen approach, whereas the anterior ethmoidal nerve block only blocks the anterior lateral nasal branch of the nerve. Although Jespersen et al. assessed the analgesic effects of a sphenopalatine ganglion block in patients receiving epidural blood patches, they successfully demonstrated that this technique can be plausibly performed under local anaesthetic.Reference Jespersen, Jaeger, Ægidius, Fabritius, Duch and Rye63 Sphenopalatine artery ligation can be performed under local anaesthetic using a maxillary nerve block via greater palatine foramen approach.Reference Jonas, Viani and Walsh64 Thus, for appropriately selected patient cohorts, the techniques outlined in this paper should provide sufficient analgesia to obviate the need for general anaesthesia or sedation as required by Lee et al.Reference Lee, Kapur and Ramsden8
• Endoscopic sinus surgery can be performed under local anaesthetic using modified dental techniques
• Local anaesthetic blocks can target nasopalatine, greater palatine, sphenopalatine and maxillary nerves
• Benefits of local anaesthetic techniques include increased safety and efficacy with limited surgical risk
A combination of shrewd patient selection and good local anaesthetic technique should hopefully negate the need for sedation. Stoical patients may better tolerate local anaesthetic endoscopic sinus surgery if they have had previous experience of dental procedures or surgery performed under local anaesthetic. Tolerance of endoscopic nasal examination in an out-patient setting may indicate likelihood of successful local anaesthetic endoscopic sinus surgery. Patients should be co-operative, following precise instruction and remaining awake for the duration of the procedure. If applicable, pre-operative counselling should inform patients of the potential risk of conversion to general anaesthetic. However, Lee et al. found conversion was only required in 1 of 554 patients undergoing local anaesthetic endoscopic sinus surgery.
Conclusion
This contemporary review of local anaesthetic midfacial nerve blocks presents an alternative option for suitable patients undergoing endoscopic sinus surgery. Although such techniques present surgical challenges for analgesia, airway protection and immobilisation, these are potentially offset by increased cost-effectiveness, reduced operative duration, shortened in-patient stay and improved patient satisfaction and safety. Ultimately, such techniques may be extended to additional nasal procedures and contribute to enhanced patient recovery and optimal utilisation of the operating theatre, increasing satisfaction for patients, surgeons and healthcare managers alike.
The authors recommend careful patient selection to facilitate local anaesthetic endoscopic sinus surgery when initially undertaking the practice and suggest liaison with dentally qualified colleagues or maxillofacial surgeons to familiarise themselves with intra-oral anaesthesia if this is an unfamiliar practice. Peripheral venous cannulation is an essential component in ensuring safety in the unlikely event of resuscitation and the authors would advise surgeons to have oxygen and monitoring available and an anaesthetist on standby for patients with multiple comorbidities.
Competing interests
None declared













