Introduction
The formation of a fistula between the external acoustic meatus and the ductal system of the parotid gland may lead to infection of either structure. The rarity and non-specific presentation of this anomaly can lead to misdiagnosis and inadequate treatment. In patients with salivary fistula, the main complaint mimics chronic otitis externa. Salivary fistulae as a result of trauma or surgery are relatively common. Congenital salivary fistulae in the external ear, on the other hand, are extremely rare, being first reported by Sharma and Dawkins in 1984.Reference Sharma and Dawkins1
Case report
A 44-year-old woman was referred by her general practitioner to the ENT clinic with a one-year history of intermittent, right-sided otorrhoea and otalgia of the right ear. She had a previous history of a spontaneous left perilymph fistula without cholesteatoma, which had been repaired 12 years prior to the current presentation via an exploratory tympanotomy. She had also been seen three years previously for facial pain on her right side, and had been diagnosed with temporomandibular joint dysfunction.
On examination, the patient was found to have infected, keratinous debris in the right external acoustic meatus. Her cranial nerves were clinically intact. Examination of her nose, neck and oropharynx was unremarkable.
Pure tone audiometry showed normal hearing thresholds bilaterally, with type A tympanograms. The patient could only tolerate a limited amount of microsuction. A microbiological swab of her otorrhoea discharge, taken by her general practitioner prior to referral, grew a heavy growth of Pseudomonas aeruginosa.
The patient was commenced on 0.3 per cent ciprofloxacin ophthalmic solution for use in her right external ear canal, and was advised to avoid the entry of water into the ear.
By her next review, the patient's otalgia had improved considerably. However, she now noticed that her otorrhoea was exacerbated whilst eating. Re-examination of her tympanic membrane was unremarkable on the right, with a moist external acoustic meatus but no signs of infection.
A sample of the patient's otorrhoea was collected for analysis in a sterile container.
A sialogram was also performed (Figure 1). The right parotid duct ostium was found to be tight, requiring dilatation before being cannulated with a small Rabinov catheter. Contrast was injected, with good filling of the extra- and intraglandular duct system. A tract of approximately 1.25 cm of contrast was seen extending posteromedially. Exact anatomical delineation was limited due to the appearance of overlying bony structures. At the end of the procedure, a small amount of contrast was noted in the right external acoustic meatus, confirming salivary otorrhoea. There was no evidence of duct dilatation or stricture.

Fig. 1 Dynamic sialogram image (oblique) using an angulated image intensifier, demonstrating parotid ductal system and fistula (arrow). TMJ = temporomandibular joint
A computed tomography (CT) scan of the right temporal bone was performed immediately after the sialogram (Figures 2 and 3). This demonstrated a 2 mm bony defect in the medial bony external acoustic meatus along the anterior meatal wall posterior to the right temporomandibular joint. Small amounts of contrast could be seen tracking behind the mandibular condyle into the defect, with contrast also present in the proximal external acoustic meatus. The features were consistent with a patent foramen tympanicum, also known as foramen of Huschke, with a further submillimetre fissure medial to this foramen.

Fig. 2 Coronal computed tomography scan demonstrating the bony defect in the bony inferior external acoustic meatus (arrow).
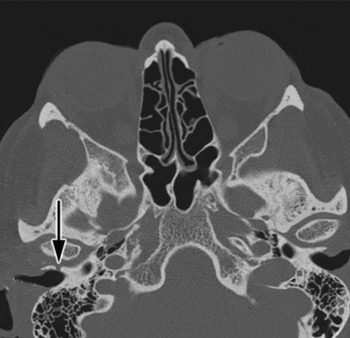
Fig. 3 Axial computed tomography scan demonstrating the bony defect in the bony external acoustic meatus anteriorly on the right (arrow).
The collected otorrhoea sample tested positive for amylase.
Unfortunately, due to the patient having an implantable cardiac defibrillator, she was unsuitable for magnetic resonance imaging (MRI) study. After a discussion of her options, the patient decided to undergo elective closure of the sialo-aural fistula under general anaesthetic.
This was performed via a parotidectomy approach. Peri-operatively, Bonney's blue dye was injected into the patient's right Stenson's duct. The dye could not be identified in the external acoustic meatus. A superficial parotidectomy incision provided good access for dissection to the anterior canal wall. Facial nerve monitoring was used throughout the procedure. The fistula was identified and ligated with 4-0 Vicryl sutures then divided (Figure 4). The skin incision was closed using subcuticular 4-0 Vicryl Rapide sutures, with a vacuum drain left for one day post-operatively.

Fig. 4 Intra-operative photographs demonstrating identification of the facial nerve (a) and of the parotid fistula (b) injected with Bonney's blue dye shown across an artery clip.
The patient made an uneventful and successful post-operative recovery and was discharged the following day.
On review in the clinic two weeks later, the patient reported complete cessation of her otorrhoea since the procedure. She was still experiencing some right-sided pain around the temporomandibular joint (TMJ), but this had also reduced substantially since the procedure. Her facial nerve was clinically intact.
Discussion
The foramen of Huschke, also known as the foramen tympanicum, is an anatomical variation in the tympanic part of the temporal bone. When present, it is located at the anteroinferior aspect of the external acoustic meatus, posteromedial to the TMJ.
The branchial apparatus, a derivative of the foregut, develops during the second week in utero and consists of five paired pharyngeal arches, separated internally by four endodermal pouches and externally by four ectodermal clefts. Abnormalities of the first branchial cleft can occur at any site from the external acoustic meatus to the angle of the mandible, including the parotid gland. During the third month in utero, the anteroinferior surface of the tympanic plate of the temporal bone is deficient, this deficiency is known as the foramen of Huschke. Closure during development is achieved by fibrous tissue, giving the meatus its ring shape.Reference Ars2 However, this bony defect may persist throughout life, resulting in cystic lesions and fistulae.
A review of 377 cadaveric temporal bones reported that the prevalence of a persistent foramen of Huschke is about 7 per cent.Reference Wang, Bingham, Hawke, Kwok and Li3 A study of 130 patients found high resolution spiral CT scanning to be a highly sensitive method of recognising a persistent foramen of Huschke; 4.6 per cent of the patients scanned demonstrated the abnormality, and the median depth of defect in the temporal bone was 1 mm.Reference Moreno, Chilvarquer, Hayek and Seraidarian4 Whilst a persistent foramen of Huschke is common, the reported prevalence represents the smallest defect in a spectrum of possible abnormalities. There are only four reported cases of associated parotid fistula, termed ‘patent foramen of Huschke’ by Sharma and Dawkins.Reference Sharma and Dawkins1, Reference Yetiser and Tosun5–Reference Rushton and Pemberton7
Several sites of fistula and sinus formation have been described in the literature, including the skin of the neck, the TMJ, a branchial cyst and a preauricular sinus.Reference Triglia, Nicollas, Ducroz, Koltai and Garabedian8–Reference Wittekindt, Schondorf, Stennert and Jungehülsing10 It is even possible for a salivary tumour to track through such a fistula into the external acoustic canal.Reference Rabinov, Alavi, Canalis and Lee11
A fistula between the TMJ and the external acoustic meatus is the most frequent type of fistula seen with a persistent foramen of Huschke, first described by Hawke et al. in 1988.Reference Hawke, Kwok, Shankar and Wang12 Patients with this anomaly usually present with TMJ dysfunction. In such cases, herniation of TMJ synovial tissue or a polypoid mass of granulation resembling a tumour in the ear meatus suggests the diagnosis.Reference Ali and Rubinstein13 It is possible that contamination of the fistula contents can lead to retrograde infection of the parotid gland. In a patient with a pre-existing bony defect and chronic external ear infection, a fistula can also develop along a path of least resistance to communicate with the parotid gland or duct system.
Management of persistent foramen of Huschke has been invariably surgical, following discovery after failed medical management. Initial investigation with a sialogram of the suspected gland may demonstrate the fistula. Further, high resolution imaging (such as CT to demonstrate bony anomalies and/or contrast-enhanced MRI to demonstrate the fistulous tract through the soft tissues) is a prudent step when planning elective repair of the defect.
Good exposure with superficial parotidectomy combined with excision of any sialocoele has been a successfully employed option.Reference Yetiser and Tosun5, Reference Langer and Begall6 If the pathology is recognised early enough then resection of the fistula in combination with closure of the bony defect can be sufficient, providing chronic infection is not present. Other management options include pharmacological suppression of salivation, irradiation and tympanic neurectomy.Reference Langer and Begall6 These options have been discussed in the context of a patient unsuitable for general anaesthesia.
This report presents a rare manifestation of a fistula between the parotid gland and the ear meatus via a patent Huschke's foramen. Diagnosis of such congenital defects is difficult. They should be suspected in patients with a history of gustatory otorrhoea, and in cases of chronic otorrhoea resistant to medical therapy in which no middle-ear disease process is apparent. Early diagnosis and treatment are needed to avoid recurrent infection of the external acoustic meatus and parotid gland. Adequate surgical treatment for symptomatic patients requires a conventional parotid approach with identification and protection of the facial nerve, as described in this report.
• This report presents a rare manifestation of a fistula between the parotid gland and the external auditory canal via a patent Huschke's foramen
• Diagnosis of such congenital defects is difficult. They should be suspected in patients with a history of gustatory otorrhoea, and in cases of chronic otorrhoea resistant to medical therapy in which no middle-ear disease process is apparent
• Adequate surgical treatment for symptomatic patients requires a conventional parotid approach, with identification and protection of the facial nerve
Acknowledgements
We thank the Lister Hospital Medical Photography and Medical Records Departments.






