Introduction
Nasal obstruction is a symptom that reduces the quality of life, and patients with nasal obstruction frequently consult an otorhinolaryngologist.Reference Han, Stringer, Rosenfeld, Archer, Baker and Brown1.2 The most common causes of nasal obstruction that can be treated surgically are nasal septal deviation and inferior turbinate hypertrophy. Nasal septal deviation has a prevalence ranging from 19 per cent to 65 per cent because of different definition criteria.Reference Smith, Edwards, Saini and Norton3,Reference Stallman, Lobo and Som4 Septoplasty is a surgical procedure used to treat nasal septal deviation. Inferior turbinate hypertrophy can be caused by increased venous sinusoidal vascularity or turbinate bone hypertrophy.Reference Farmer and Eccles5 In addition to surgical methods, medical treatments are indicated for inferior turbinate hypertrophy.Reference Farmer and Eccles5 Radiofrequency ablation is one of the most common surgical approaches for treating mucosal hypertrophy of the inferior turbinate. It is often performed in combination with septoplasty by many otorhinolaryngologists.Reference Devseren, Ecevit, Erdag and Ceryan6
Nasal obstruction that can be documented objectively might not much disturb the patient, while nasal obstruction that cannot be documented objectively might present as subjective symptoms in the patient.Reference Güvenç and Ecevit7,Reference Onerci Celebi, Araz Server, Yigit and Longur8 The Nasal Obstruction Symptom Evaluation scale, 22-item Sino-Nasal Outcome Test (SNOT-22), Rhinosinusitis Quality of Life Survey and Chronic Sinusitis Survey are the most commonly used subjective methods,Reference Güvenç and Ecevit7 while acoustic rhinometry and peak nasal inspiratory flow (PNIF) measurements are the most commonly used objective methods for evaluating nasal obstruction.Reference Starling-Schwanz, Peake, Salome, Toelle, Ng and Marks9
Septal deviation is usually accompanied by inferior turbinate hypertrophy, which may or may not be compensatory. Although many studies have shown the effect of conchal reduction on the success of septoplasty in patients with septal deviation, there is still no consensus.Reference Han, Stringer, Rosenfeld, Archer, Baker and Brown1,Reference van Egmond, Rovers, Tillema and van Neerbeek10 As mentioned, many parameters are used to evaluate nasal obstruction. However, few studies have demonstrated the effect of turbinate surgery on the quality of life of patients undergoing septoplasty using objective methods.Reference van Egmond, Rovers, Tillema and van Neerbeek10 The present study aimed to assess the effect of conchal reduction on the success of septoplasty in patients with septal deviation and conchal hypertrophy using objective and subjective methods.
Materials and methods
Study design
The present study was a single-centre, parallel-group, randomised, controlled study. Ethics committee approval was obtained from the University of Health Sciences Istanbul Training and Research Hospital Local Ethics Committee (approval number: 9/05/2015-663). Written consent forms were obtained from all patients included in the study.
Participants
Patients aged 18–45 years who presented to the ENT clinic with a complaint of nasal obstruction and who were diagnosed with septal deviation and inferior turbinate hypertrophy were included in the study. Routine ENT examinations were performed for all patients. Patients whose nasal obstruction was found to be caused by septal deviation, based on performing rhinoscopy and endoscopic nasal examinations, were indicated for septoplasty.Reference Han, Stringer, Rosenfeld, Archer, Baker and Brown1 A total of 128 patients were assessed for eligibility. The allocation ratio was 1:1 for the two groups. For allocation of the participants, a computer-generated list of random numbers was used.
Patients who underwent open septoplasty were excluded from the study. Moreover, patients who still had conchal hypertrophy after decongestion were excluded from the study because of the possibility of conchal bone compartment hypertrophy. In addition, patients were excluded from the study if they: had undergone revision nasal surgical procedures; had a history of any nasal surgery; had additional nasal problems, such as nasal valve deficiency or nasal polyposis; had a history of allergic rhinitis; had symptoms suggestive of allergic rhinitis, such as an itchy nose or nasal serous drainage; had respiratory problems, such as asthma or chronic pulmonary diseases, and were unable to perform nasal tests; or had systemic diseases or were receiving systemic medical treatments (e.g. beta blockers for hypertension).
Interventions
Patients with both septal deviation and turbinate hypertrophy were randomly divided into two groups. The patients in group A underwent septoplasty with inferior turbinate radiofrequency ablation in the same session, while those in group B underwent septoplasty alone. All the operations were performed by one of three surgeons. A radiofrequency generator (Celon Lab ENT; Celon AG Medical Instruments, Berlin, Germany) with a hand-held disposable bipolar electrode was used for the inferior concha ablations, at 15 W.
All patients in both groups were asked to complete the Nasal Obstruction Symptom Evaluation scale and SNOT-22 before and three months after surgery. Acoustic rhinometry and PNIF measurements were also performed before and three months after surgery.
Before the acoustic rhinometry and PNIF measurements were performed, all patients underwent a nasal examination to eliminate any secretions or foreign bodies. Acoustic rhinometry and PNIF measurements were performed at 10 minute intervals. No decongestant agent was applied, in order to maintain the inferior turbinate mucosal status.
The PNIF measurement was performed using a Youlten PNIF meter (Clement Clarke International, Harlow, UK). Each patient was made to sit and rest for 15 minutes, following which they cautiously blew their nose. The PNIF values are expressed in litres per minute.
Acoustic rhinometry was performed 10 minutes after the PNIF measurement. Acoustic rhinometry was performed using an acoustic rhinometry device (RhinoScan (Manual v. 2.6 ed. 1.1); RhinoMetrics, Smørum, Denmark), which produces acoustic signals in the form of interrupted pulses, in accordance with the criteria set and recommended by the Acoustic Rhinometry Standardization Committee.Reference Vogt, Bachmann-Harildstad, Lintermann, Nechyporenko, Peters and Wernecke11 For each nostril, at least three measurement curves were obtained. Curves that exceeded a standard deviation (SD) of 2 per cent (selected as the acceptable level in curves generated during acoustic measurements) were excluded. The average values of the three obtained curves were considered. The scales – automatically determined by the device for the measurement curves – were as follows: the mean cross-sectional areas 1 and 2 were considered at a distance of 0.00–2.2 cm and 2.20–5.40 cm, respectively, from the nasal entrance. Cross-sectional areas are expressed in centimetres squared, while distances and volumes are expressed in centimetres and centimetres cubed, respectively.
Statistical analysis
Descriptive statistics are presented as: means and SDs; medians, and ranges; and frequencies and ratios. The distribution of variables was assessed using the Kolmogorov–Smirnov test. Independent quantitative data were analysed using the Mann–Whitney U test, while dependent quantitative data were analysed using the Wilcoxon test. The chi-square test was used for analysing independent qualitative data. SPSS® software version 22.0 was used for statistical analysis.
Results
One patient refused to participate. One patient had undergone open surgery. Two patients who still had conchal hypertrophy after decongestion were excluded from the study. Five patients were undergoing revision nasal surgical procedures; 3 patients had additional nasal problems, such as nasal valve deficiency or nasal polyposis; and 10 patients had a history of allergic rhinitis or had symptoms suggestive of allergic rhinitis, such as an itchy nose or nasal serous drainage. Two patients had asthma, and four patients had systemic disease.
In total, 100 patients were eligible for inclusion in the present study. Of these, 10 patients were excluded because of post-operative complications, such as nasal synechia, septal haematoma, septal perforation and epistaxis (6 patients from group A (septoplasty plus inferior turbinate radiofrequency) and 4 patients from group B (septoplasty alone)). Moreover, 16 patients could not be reached for the three-month follow up (8 patients from group A and 8 patients from group B).
Thus, the study was completed with 74 patients (Figure 1). Group A comprised 36 patients (13 females and 23 males), with a median age of 31.5 years (mean ± SD = 33.1 ± 10.7 years). Group B comprised 38 patients (11 females and 27 males), with a median age of 39.0 years (mean ± SD = 38.7 ± 12.7 years). There were no significant differences between the groups in terms of female-to-male ratio or mean age (p = 0.511 and 0.06, respectively).
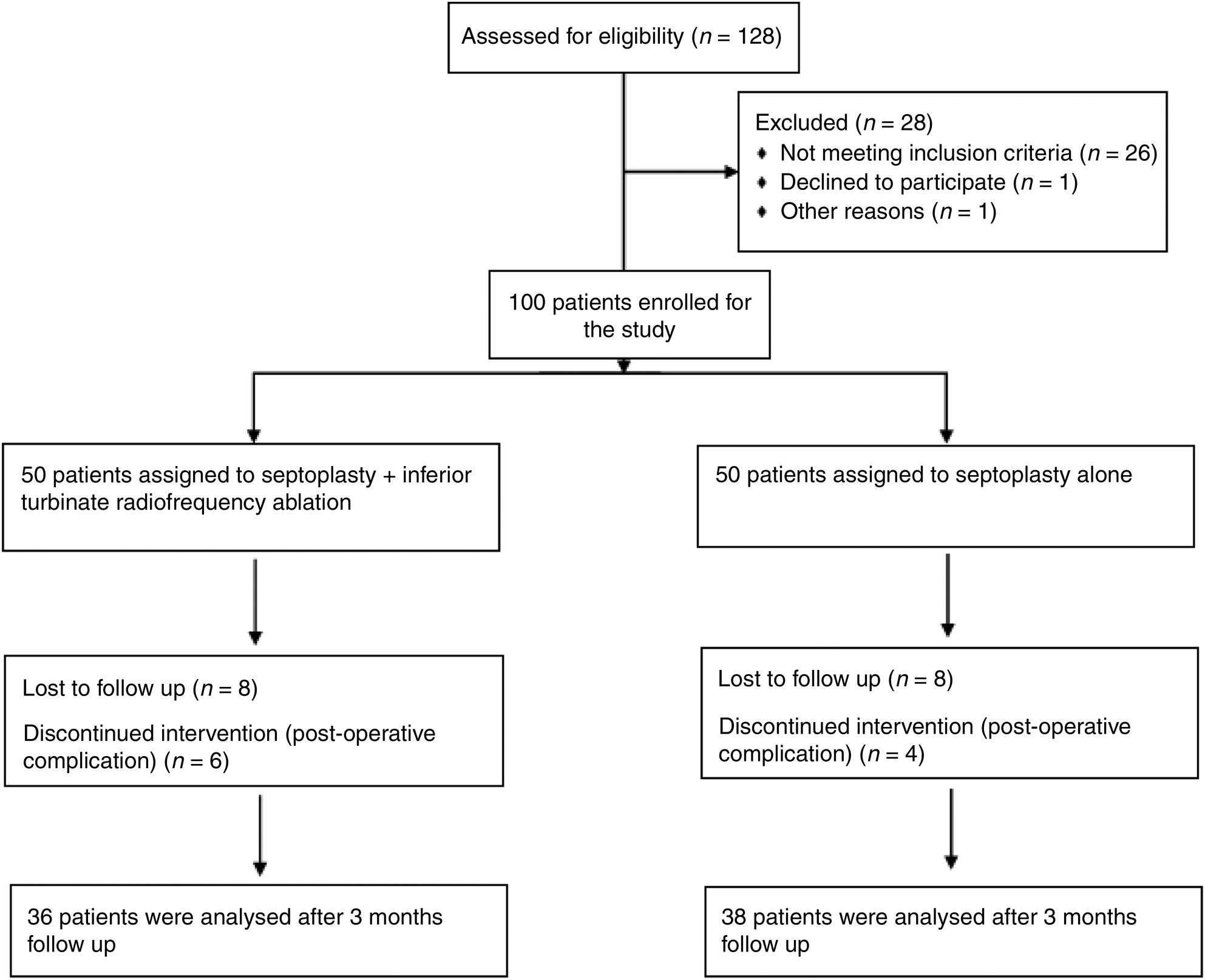
Fig. 1. Study flow diagram.
Acoustic rhinometry values
Left and right mean cross-sectional area 1 values increased after surgery in both groups; however, there were no significant differences between the groups (p = 0.396 and 0.750, respectively). Similarly, left and right mean cross-sectional area 2 values increased after surgery in both groups; however, there were no significant differences between the groups (p = 0.737 and 0.381, respectively).
Peak nasal inspiratory flow values
Post-operative PNIF values significantly increased in both groups. There was no significant difference between the groups (p = 0.991).
The data of the objective evaluation methods are shown in Table 1.
Table 1. Acoustic rhinometry and peak nasal inspiratory flow results

Data represent mean ± standard deviation values, unless indicated otherwise. *Mann–Whitney U test. †Wilcoxon test. ‡Indicates significant difference. MCA = mean cross-sectional area; pre-op = pre-operative; post-op = post-operative; PNIF = peak nasal inspiratory flow
Survey results
There were no differences between the groups in terms of the pre-operative survey scores (SNOT-22 and Nasal Obstruction Symptom Evaluation) (Table 2).
Table 2. Survey results

Data represent mean ± standard deviation values, unless indicated otherwise. *Mann–Whitney U test. †Wilcoxon test. ‡Indicates significant difference. SNOT-22 = Sino-Nasal Outcome Test-22; pre-op = pre-operative; post-op = post-operative; NOSE = Nasal Obstruction Symptom Evaluation scale
The post-operative survey scores showed a significant decrease in both groups.
The pre-operative Nasal Obstruction Symptom Evaluation scores did not differ significantly between the groups. Although the post-operative Nasal Obstruction Symptom Evaluation scores were significantly higher in group B than in group A, the change in scores (before vs after the surgery) did not differ significantly between the groups.
All patients in both groups showed a significant improvement in acoustic rhinometry and PNIF values, and in Nasal Obstruction Symptom Evaluation and SNOT-22 scores after the surgery. However, there were no significant differences between the groups. In other words, the addition of inferior turbinate radiofrequency ablation to septoplasty did not have significantly better outcomes than septoplasty alone.
We also interpreted the results of subjective and objective methods to be concordant; however, we did not perform any statistical analysis to verify this.
Discussion
In the present study, we randomly performed either septoplasty alone or septoplasty combined with inferior turbinate radiofrequency ablation in patients diagnosed with septal deviation and conchal hypertrophy who presented with a complaint of nasal obstruction. Objective and subjective methods revealed improvements for both groups after surgery. However, these improvements did not differ significantly between the two groups.
It is generally accepted that surgical reduction of the hypertrophic inferior nasal turbinate combined with septoplasty improves nasal obstruction.Reference Han, Stringer, Rosenfeld, Archer, Baker and Brown1,Reference Grymer, Illum and Hilberg12,Reference Illum13 Many studies have assessed the efficacy of combining inferior turbinate surgery with septoplasty. However, most studies have focused on nasal obstruction and evaluated nasal obstruction using more than one method. Given the difficulties encountered in measuring nasal obstruction, a subjective finding, the results of studies based on measurements using a single method may be inconsistent. There are multiple objective methods, such as acoustic rhinometry and PNIF measurements, and many subjective methods, such as the Nasal Obstruction Symptom Evaluation and SNOT-22, for evaluating nasal obstruction. In the present study, we evaluated nasal obstruction using both objective and subjective methods.
Stölzel et al. evaluated the effects of inferior turbinate surgery using SNOT-22 and anterior rhinomanometry.Reference Stölzel, Bandelier, Szczepek, Olze and Dommerich14 They found turbinate surgery to be effective. However, they did not compare the findings with those of patients who did not undergo inferior turbinate surgery; they only compared among patients who underwent turbinate surgery.Reference Stölzel, Bandelier, Szczepek, Olze and Dommerich14
Nilsen et al. reported improvements in nasal obstruction, runny nose, snoring, mouth breathing and SNOT-22 scores in all patients who underwent either septoplasty alone, septoplasty combined with radiofrequency ablation, or radiofrequency ablation alone.Reference Nilsen, Helvik, Thorstensen and Bugten15 They noted greater improvements in nasal obstruction symptoms in patients who underwent septoplasty combined with conchal reduction. In that study, nasal obstruction symptoms were evaluated using a visual analogue scale (VAS).Reference Nilsen, Helvik, Thorstensen and Bugten15 A VAS was not used in the present study. However, there was no difference between the groups in terms of improvements in nasal obstruction assessed using objective methods.
When evaluating patients who have undergone surgical procedures for nasal obstruction, the severity and area of obstruction and recovery can be more clearly assessed using objective methods. Nilsen et al. evaluated the efficiency of septoplasty and radiofrequency ablation by performing acoustic rhinometry and PNIF measurements.Reference Nilsen, Thorstensen, Helvik, Nordgaard and Bugten16 They reported improvements in both anterior and posterior areas in the septoplasty group, but only in the posterior area in the radiofrequency ablation group. Moreover, they found that PNIF values improved in all patient groups and the nasal obstruction was corrected even in different regions.Reference Nilsen, Thorstensen, Helvik, Nordgaard and Bugten16
In another study involving 80 patients, acoustic rhinometry revealed an improvement in nasal breathing after additional reduction of the hypertrophic inferior turbinate.Reference Grymer, Illum and Hilberg12 In that study, after five years of follow up, no significant differences were found between the patient groups with and without additional reduction of the hypertrophic inferior turbinate, as assessed using questionnaires (n = 50) or acoustic rhinometry (n = 37).Reference Illum13
• This study assessed whether inferior turbinate reduction combined with septoplasty improved patients’ outcomes
• Outcomes were assessed using acoustic rhinometry, peak nasal inspiratory flow (PNIF), Sino-Nasal Outcome Test-22 (SNOT-22) and Nasal Obstruction Symptom Evaluation
• Adding inferior turbinate radiofrequency reduction to septoplasty did not benefit patients more than septoplasty alone
• Both septoplasty and septoplasty plus turbinate radiofrequency improved patients’ outcomes for nasal obstruction
• Findings for acoustic rhinometry, PNIF, and SNOT-22 and Nasal Obstruction Symptom Evaluation scales were compatible with each other
Nunez and Bradley found no differences between the patient groups using anterior rhinomanometry or questionnaires (26 patients).Reference Nunez and Bradley17 de Moura et al. investigated the effects of excision of one-third of the inferior turbinates in rhinoseptoplasty patients using quality of life surveys, and reported no significant differences between the groups.Reference de Moura, Migliavacca, Lima, Dolci, Becker and Feijó18
In contrast, Devseren et al. noted a significant improvement at six months after the surgery in a group of patients who underwent additional reduction of the compensatory hypertrophic inferior turbinate.Reference Devseren, Ecevit, Erdag and Ceryan6 In that study, the submucous resection technique was used. Acoustic rhinometry and a VAS were used to measure the outcomes.Reference Devseren, Ecevit, Erdag and Ceryan6
In a meta-analysis examining many studies on septoplasty and turbinate surgery, van Egmond et al. emphasised that limited studies have compared septoplasty combined with turbinate surgery with septoplasty alone.Reference van Egmond, Rovers, Tillema and van Neerbeek10 Moreover, they stated that post-operative improvements were generally observed, but the results had methodological flaws. They also emphasised the insufficiency of studies comparing septoplasty and medical treatment.Reference van Egmond, Rovers, Tillema and van Neerbeek10
In the present study, we found that conchal surgery did not provide additional improvement in patients with septal deviation. Medical treatment may be preferred over conchal reduction for conchal pathologies in patients with septoplasty indications. In this way, additional complications, such as crusting caused by turbinate surgery and an increased risk of synechiae, can be avoided. In another study by van Egmond et al., patients who underwent septoplasty and/or conchal surgery were compared with patients who were treated with non-surgical medical therapy.Reference van Egmond, Rovers, Hannink, Hendriks and van Heerbeek19 The authors reported surgery to be more effective than medical therapy. However, in that study, the superiority of conchal surgery over medical treatment in patients with septal deviation was not clearly demonstrated.Reference van Egmond, Rovers, Hannink, Hendriks and van Heerbeek19 Further studies in which medical therapy is preferred are required to support this view.
The present study revealed no significant differences in patient outcomes associated with the addition of inferior turbinate radiofrequency ablation to septoplasty. This might be because of randomised patient selection for turbinate intervention, as the patients in both groups had similar scores before the surgery as well.
In our study, both groups benefitted from surgical intervention and both surgery types were successful. Objective evaluations demonstrated that the addition of inferior turbinate radio frequency to septoplasty did not provide any additional benefit. When it comes to subjective assessments, although there seems to be no difference between post-operative groups in terms of SNOT scores (p = 0.051, reflecting ‘borderline insignificance’), there was a significant difference between post-operative groups in the Nasal Obstruction Symptom Evaluation scores. However, the p-value for the latter was insignificant when the differences between pre- and post-operative changes within each group were compared. When we examine the results regardless of the p-value, the change score for group A (septoplasty plus inferior turbinate radiofrequency) was higher than that for group B (septoplasty alone), for both questionnaires. Perhaps more accurate results can be obtained if the sample size is increased.
Conchal hypertrophy was assessed only by examinations performed before and after decongestant application during rhinoscopy. Performing objective assessments after decongestion is one of the limitations of the present study. Furthermore, although a 3-month follow up is sufficient according to some publications, the absence of a long-term follow-up period of 6–12 months can be considered a limitation.
Conclusion
Inferior turbinate ablation combined with septoplasty does not provide any more benefit to the objective and subjective outcomes of patients than septoplasty alone.
Competing interests
None declared





