Introduction
Leishmaniasis is a disease complex caused by protozoa parasites of the Leishmania genus, which affects more than 12 million people worldwide. It presents an annual incidence of 1.5–2.0 million new cases, with 380 million people at risk of contracting the infection (WHO, 2018). The clinical manifestations of this disease complex are varied, reaching single cutaneous lesions caused by cutaneous leishmaniasis until the fatal visceral infection caused by visceral leishmaniasis (VL) (Torres-Guerrero et al., Reference Torres-Guerrero, Quintanilla-Cedillo, Ruiz-Esmenjaud and Arenas2017); and the occurrence of symptoms depends primarily on the immunological status of the infected hosts and the infecting parasite species (Tajebe et al., Reference Tajebe, Getahun, Adem, Hailu, Lemma, Fikre, Raynes, Tamiru, Mulugeta, Diro, Toulza, Shkedy, Ayele, Modolell, Munder, Müller, Takele and Kropf2017). No vaccination protocol is available to prevent human disease, and treatment presents problems due to toxicity, high cost and/or emergence of parasite resistance (Srivastava et al., Reference Srivastava, Shankar, Mishra and Singh2016; Ponte-Sucre et al., Reference Ponte-Sucre, Gamarro, Dujardin, Barrett, López-Vélez, García-Hernández, Pountain, Mwenechanya and Papadopoulou2017; Kaye et al., Reference Kaye, Cruz, Picado, Van Bocxlaer and Croft2020). In this context, a safe, rapid and precise diagnosis of leishmaniasis could allow one to identify the patients and promptly treat them in an initial clinical phase of disease, as well as reduce the side effects of the available drugs (Sakkas et al., Reference Sakkas, Gartzonika and Levidiotou2016). Symptomatic VL causes such symptoms as fever, splenomegaly, hepatomegaly, weight loss, anaemia and pancytopoenia, among others. In addition, it is nearly always fatal if acute and left untreated (Coutinho et al., Reference Coutinho, Santos, Ribeiro, Oliveira, Dantas, Santos and Tauhata2017); therefore, early diagnosis can prevent mortality. Similarly, there is an estimated incidence of 35 million people living with human immunodeficiency virus (HIV) in the world. It is well-known that Leishmania can cause an opportunistic infection among HIV-infected patients in areas where both diseases coexist (Luz et al., Reference Luz, Naves, Carvalho, Meira, Dias and Fontes2018). The immunosuppression caused by the virus may reactivate latent parasite infection in asymptomatic patients (Lindoso et al., Reference Lindoso, Moreira, Cunha and Queiroz2018). Moreover, the impact of coinfection hampers the diagnosis of the diseases, as well as the therapeutic response against them (Alvar et al., Reference Alvar, Aparicio, Aseffa, Den Boer, Cañavate, Dedet, Gradoni, Ter Horst, López-Vélez and Moreno2008; Cota et al., Reference Cota, Sousa and Rabello2011).
Parasitological methods are considered the gold standard for VL diagnoses. However, their sensitivity is variable, since parasites, or their genetic content, need to be present in the analysed biological samples (Ruiter et al., Reference Ruiter, Van Der Veer, Leeflang, Deborggraeve, Lucas and Adams2014). On the contrary, immunological methods, such as enzyme-linked immunosorbent assay (ELISA) and direct agglutination tests (DATs), have also been used for VL diagnoses (Thakur et al., Reference Thakur, Joshi and Kaur2020). However, in the VL/HIV coinfection cases, the sensitivity has been hampered, limiting the diagnostic value, since only about 40% of the coinfected patients are diagnosed, as compared to the 90–95% of the cases detected in immunocompetent patients (Srividya et al., Reference Srividya, Kulshrestha, Singh and Salotra2012; Silva et al., Reference Silva, Brandão, Colovati, Sousa, Lima, Dorta, Ribeiro-Dias, Costa, Costa and Oliveira2018). In this context, and due to the scarcity of sensitive markers to diagnose VL/HIV-coinfected patients, new studies to find novel and more suitable diagnostic antigens should be performed (Santos-Gomes et al., Reference Santos-Gomes, Gomes-Pereira, Campino, Araújo and Abranches2000; Kumar et al., Reference Kumar, Pai, Tripathi, Pandey and Sundar2002; Cota et al., Reference Cota, Sousa, Demarqui and Rabello2012). Under such conditions, in addition to testing recombinant proteins and/or B-cell chimeras for the VL diagnosis, other types of antigens, such as synthetic peptides, could also be considered, as they are simpler, more specific, more stable, and cheaper to produce, when compared to the recombinant proteins (Carvalho et al., Reference Carvalho, Mendes, Coelho, Duarte and Menezes-Souza2018; Rodrigues et al., Reference Rodrigues, Santos, Miyazaki, Martins, Ludolf, Kursancew, Ramos, Dias, Oliveira, Vieira, Roatt, Machado-de-Ávila, Gonçalves, Menezes-Souza, Coelho and Duarte2019).
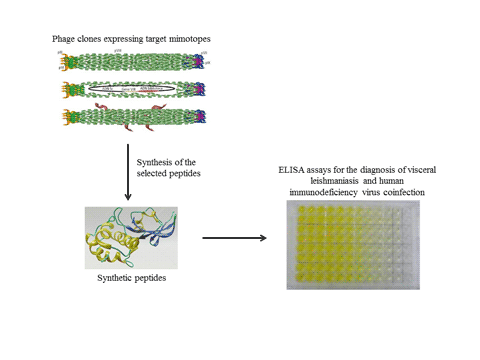
Phage display is a proteomic technology, considering that phage-surface-exposed epitopes, called mimotopes, recognize specific ligands (Almagro et al., Reference Almagro, Pedraza-Escalona, Arrieta and Pérez-Tapia2019). Large repertoires of random peptide sequences in the libraries offer the advantage that a high number of sequences can be screened in relatively short-experimental procedures (Kuhn et al., Reference Kuhn, Fühner, Unkauf, Moreira, Frenzel, Miethe and Hust2016). The biopanning cycles consist of isolating phage clones that bind specifically to a target molecule and then identifying their insert through sequencing (Manoutcharian, Reference Manoutcharian2005). This technique has been used to identify mimotopes, with applications as new diagnostic markers, vaccine candidates and/or immunotherapeutic targets against leishmaniasis (Costa et al., Reference Costa, Lima, Chávez-Fumagalli, Menezes-Souza, Martins, Duarte, Lage, Lopes, Lage, Ribeiro, Andrade, Magalhães-Soares, Soto, Tavares, Goulart and Coelho2014, Reference Costa, Chávez-Fumagalli, Martins, Duarte, Lage, Lima, Pereira, Soto, Tavares, Goulart and Coelho2015, Reference Costa, Salles, Santos, Ramos, Lima, Lima, Portela, Chávez-Fumagalli, Duarte, Menezes-Souza, Machado-de-Ávila, Silveira, Magalhães-Soares, Goulart and Coelho2017; Toledo-Machado et al., Reference Toledo-Machado, Avila, Nguyen, Granier, Bueno, Carneiro, Menezes-Souza, Carneiro, Chávez-Olórtegui and Fujiwara2015a; Link et al., Reference Link, Alban, Soccol, Pereira and Soccol2017). Costa et al. (Reference Costa, Lima, Chávez-Fumagalli, Menezes-Souza, Martins, Duarte, Lage, Lopes, Lage, Ribeiro, Andrade, Magalhães-Soares, Soto, Tavares, Goulart and Coelho2014) identified eight mimotopes, which are reactive against antibodies purified from VL dogs, and tested them for canine VL diagnosis, with results showing a 100% sensitivity, specificity and accuracy in the ELISA experiments. In another study, two mimotopes, called B10 and C01, as well as their synthetic peptides, were tested for the diagnosis of canine and human VL, and the results showed high sensitivity and specificity values to diagnose the diseases (Costa et al., Reference Costa, Salles, Santos, Ramos, Lima, Lima, Portela, Chávez-Fumagalli, Duarte, Menezes-Souza, Machado-de-Ávila, Silveira, Magalhães-Soares, Goulart and Coelho2017). Therefore, in the current study, phage display technology was used to select antigens to be evaluated for the diagnosis of VL and VL/HIV coinfection. Biopanning cycles using negative and positive selection processes were performed, and 43 phage clones were selected by antibodies in sera from VL and VL/HIV patients, but not by those from healthy subjects and HIV-infected patients; these were then isolated and sequenced. Results showed nine valid and non-repetitive sequences, and the epitopes were produced as synthetic peptides and evaluated in ELISA experiments against a human serological panel. In this context, the current study described, for the first time, the application of phage display technology, using sera from healthy subjects, as well as of VL, HIV and VL/HIV-coinfected patients, to select novel antigens to be used in the diagnosis of VL and VL/HIV coinfection.
Materials and methods
Parasites and antigen preparation
Leishmania infantum (MOM/BR/1970/BH46) parasites were grown at 24 °C in Schneider's medium (Sigma, St. Louis, MO, USA), together with 20% heat-inactivated fetal bovine serum (Sigma), 20 mm l-glutamine, 200 U mL−1 penicillin and 100 μg mL−1 streptomycin at pH 7.4. The soluble Leishmania antigenic extract (SLA) was prepared from stationary-phase promastigotes according to that described elsewhere (Coelho et al., Reference Coelho, Tavares, Carvalho, Chaves, Teixeira, Rodrigues, Charest, Matlashewski, Gazzinelli and Fernandes2003). For this, 109 stationary promastigotes were washed three times in cold sterile phosphate-buffered saline (PBS 1×) and subjected to six cycles of freezing (−196°C) and thawing (37°C), followed by ultrasonication (Ultrasonic processor, GEX600) with five cycles of 30 s at 38 MHz. The suspension was then centrifuged at 8000 g for 30 min at 4°C, the supernatant containing SLA was collected, and the protein concentration was estimated by the Bradford method (Bradford, Reference Bradford1976). Aliquots (500 μL, each) were prepared and stored at −80°C until use.
Ethics statement and serum samples
Serum samples of VL (n = 30), VL/HIV-coinfected (n = 25) and HIV-infected (n = 20) patients were used. Leishmania infection was confirmed by the polymerase chain reaction technique to identify L. infantum kDNA in spleen or bone marrow aspirates (Cota et al., Reference Cota, Sousa, Nogueira, Gomes, Oliveira, Assis, Mendonça, Pinto, Saliba and Rabello2013). HIV diagnosis was based on clinical evaluation and blood collection to determine the CD4+ T-cell count to determine the viral load in the patients. Samples were also collected from healthy individuals living in an endemic region of VL (n = 25), who presented no clinical signal of disease and showed negative serological results (Kalazar Detect™ Rapid Test Kit). Sera from Chagas disease patients (n = 15), diagnosed by haemoculture, Chagatest® recombinant ELISA v.4.0 kit and/or Chagatest® haemagglutination inhibition (Wiener Lab., Rosario, Argentina), as well as from leprosy (n = 10), tuberculosis (n = 10) and malaria (n = 10) patients were used in the serological assays.
Biopanning cycles using negative and positive selection processes
A Ph.D. library (Ph.D.®-C7C library, New England BioLabs, USA) was used to select conformational epitopes by phage display, according to that described elsewhere (Costa et al., Reference Costa, Lima, Chávez-Fumagalli, Menezes-Souza, Martins, Duarte, Lage, Lopes, Lage, Ribeiro, Andrade, Magalhães-Soares, Soto, Tavares, Goulart and Coelho2014). Serum pools of VL (n = 10), HIV (n = 10) and VL/HIV-coinfected (n = 10) patients, in addition to the sera from healthy subjects (n = 10), were also used. For this, 1012 viral particles of the library were diluted in 250 μL of 50 mm Tris–HCl (pH 7.5), 150 mm NaCl and 0.1% Tween 20 buffer (TBS-T). The phages were incubated for 30 min at room temperature with microspheres coupled to the healthy subject sera, which were magnetically captured in order to perform the negative selection process. The non-ligated phages were recovered and transferred to a new tube, which was also subjected to negative selection using HIV-infected patient sera. Phages in the supernatant were recovered and positive selection processes were performed by incubating them first with VL patient sera and, subsequently, with VL/HIV-coinfected patient sera. The supernatant was removed, and the bound phages were washed five times in 1 mL TBS-T buffer and eluted in 500 μL of 0.2 m glycine buffer, pH 2.0. Next, 75 μL of 1 m Tris-base (pH 9.0) was added to neutralize the acidic pH of the solution. After the biopanning cycles, 43 clones were individually chosen for a sterile culture microplate (96-well microtest TM plate, BD Falcon TM clear, USA) in LB medium. A sequencing reaction was performed by capillary electrophoresis on the ABI 3130 equipment with the BigDye v 3.1 and POP7 polymer (Myleus Biotechnology®, Belo Horizonte), and sequence scanner software (Applied Biosystems) was used for analyses of AB1 output files. Of the 43 selected clones, nine valid and non-repeated amino acid sequences were identified.
Bioinformatics assays
The analyses were performed with the 7-mer peptide sequence and the amino acid sequences (AC-XXXXXXX-CGGGS) contained in the fusion with the pIII phage capsid protein, as described elsewhere (Alves et al., Reference Alves, Fujimura, Morais and Goulart2014). The identified epitopes were analysed by Expasy (http://web.expasy.org/translate/) and Basic Local Alignment Search Tool (http://blast.ncbi.nlm.nih.gov/Blast.cgi) servers against Leishmania proteins of the Protein Database (PDB), and the domain regions were validated using the protein family database (http://pfam.xfam.org/). The conformational alignment was performed with PepSurf software (http://pepitope.tau.ac.il/), and results were based on the values of combination (match), incompatibility (mismatch) and the absence of the corresponding amino acids (in the match) between the aligned peptides, which were filtered according to the greatest similarity presented to identify the possible host proteins.
ELISA experiments
For the ELISA experiments, previous titration curves were performed to determine the most appropriate conditions for the serological assays. In this context, antigen concentrations of 1.25 μg per well for Pep5, Pep6, Pep7 and Pep9; of 2.50 μg per well for Pep1, Pep4 and Pep8 and of 5.0 μg per well for Pep2 and Pep3, were used. Leishmania infantum SLA was used at a concentration of 1.0 μg per well. Microtitre immunoassay plates (Jetbiofil®, Belo Horizonte) received the antigens diluted in a 100 μL coating buffer (50 mm carbonate buffer) at pH 9.6 for 16 h at 4°C. Free-binding sites were blocked with a blocking solution (250 μL per well), consisting of PBS 1× and 0.05% Tween 20 (PBS-T) plus 5% non-fat dry milk solution, for 1 h at 37°C. Plates were washed and incubated with 100 μL serum samples (diluted 1:100 for Pep5 and SLA or 1:200 for the other peptides) for 1 h at 37°C, at which time they were washed with PBS-T. Next, the anti-human immunoglobulin G (IgG) peroxidase-conjugated antibody (Sigma, St. Louis, USA) was added (diluted 1:5000 for Pep1, Pep3, Pep5, Pep7, Pep8, Pep9 and SLA or 1:10 000 for Pep2, Pep4 and Pep6) for 1 h at 37°C. Plates were then washed with PBS-T, and reactions were developed using 100 μL of a solution consisting of 2 μL H2O2, 2 mg ortho-phenylenediamine and 10 mL citrate-phosphate buffer (pH 5.0) for 30 min in the dark. Reactions were then stopped by adding 25 μL 2 N H2SO4, and optical density (OD) values were read in an ELISA microplate reader (Molecular Devices, Spectra Max Plus, Canada) at 492 nm.
Prognostic evaluation after VL treatment
The synthetic peptides that presented better sensitivity and specificity values in the previous ELISA experiments were tested against serum samples of VL patients (n = 8), which were collected before and 6 months after treatment, performed using pentavalent antimonials (Sanofi Aventis Farmacêutica Ltda., Suzano, São Paulo, Brazil). All patients were subjected to the same therapeutic regimen, using these pharmaceutical drugs at a dose of 20 mg Sb5+ per kg for 30 days. None of the patients suffered from any other infections or had any pre-existing disease. Additionally, when they completed the treatment, no sign or symptom of VL was observed, and patients presented no parasite content in their spleen and/or bone marrow aspirates.
Statistical analysis
Results were entered into Microsoft Excel (version 10.0) spreadsheets and analysed using GraphPad Prism™ (version 6.0 for Windows). Receiver operating characteristic (ROC) curves were constructed to obtain the cut-off values, as well as sensitivity (Se), specificity (Sp) and area under the curve (AUC) of the antigens. The one-way analysis of variance, followed by Bonferroni's post-test, was used for comparisons between groups. Differences were significant with P < 0.05.
Results
Selection of the best phage-exposed epitopes by phage display
Negative and positive selection processes were performed by phage display using IgG antibodies purified from serum samples of healthy subjects or VL, HIV-infected and VL/HIV-coinfected patients, aiming to select phage-exposed epitopes that were reactive with VL and VL/HIV sera. Results showed that 43 phage clones were selected and their DNA sequences were deduced by the Expasy server, when nine valid and non-repetitive sequences were identified. These peptide sequences were commercially synthetized with the AC-XXXXXXX-CGGGS conformation (Table 1), aiming to increase the quality of interaction in the ELISA plates.
Table 1. Amino acid sequences from identified and selected epitopes by phage display

The sequences of the nine identified and selected phage-exposed epitopes are shown underlined between the ‘AC-’ and ‘-CGGGS’ linkers of the capsid molecule.
Diagnostic evaluation of the selected phage-exposed epitopes tested as synthetic peptides
Immunological assays were performed using the nine synthetic peptides (Pep1, Pep2, Pep3, Pep4, Pep5, Pep6, Pep7, Pep8 and Pep9) against a human serological panel. Leishmania infantum SLA was used as the control. Results indicating the individual OD values against each peptide and SLA are shown (Fig. 1). Data suggest that Pep2, Pep3 and Pep4 were recognized by all VL and VL/HIV-coinfected patient sera, since the OD values were above the respective cut-off values. The other peptides and SLA showed a moderate performance, with OD values of VL and VL/HIV patients presenting variable reactivity against such antigens. ROC curves were constructed to determine the AUC values, which were of 1.0 for Pep2, Pep3 and Pep4, and ranged from 0.70 to 0.82 for the other peptides, as well as 0.82 for SLA (Table 2). The sensitivity and specificity were also calculated, and sensitivity and specificity values were both of 100% for Pep2, Pep3 and Pep4, while the sensitivity varied from 50.9 to 80.0% for the other peptides, and specificity values ranged from 60.0 to 95.6% (Table 3). Using SLA, the sensitivity and specificity values were of 92.7 and 62.2%, respectively.

Fig. 1. Serological evaluation of the antigens for VL and VL/HIV coinfection. ELISA experiments were performed using 145 serum samples that were collected from VL (HVL; n = 30), VL and HIV (HVL/HIV; n = 25) coinfected, HIV-infected (HIV; n = 20), malaria (MAL; n = 10), Chagas disease (CD; n = 15), tuberculosis (TB; n = 10) and leprosy (HD; n = 10) patients. Samples from healthy individuals living in an endemic region (HC; n = 25) were also used. Reactions against the individual peptides and Leishmania infantum SLA are shown here. The cut-off values (dotted lines) for positive (VL and VL/HIV samples) and negative (other samples) discrimination were determined by calculating ROC curves. Pep1, peptide 1; Pep2, peptide 2; Pep3, peptide 3; Pep4, peptide 4; Pep5, peptide 5; Pep6, peptide 6; Pep7, peptide 7; Pep8, peptide 8; Pep9, peptide 9; SLA, Leishmania antigenic extract.
Table 2. Performance of the diagnostic antigens

Pep1: peptide 1; Pep2: peptide 2; Pep3: peptide 3; Pep4: peptide 4; Pep5: peptide 5; Pep6: peptide 6; Pep7: peptide 7; Pep8: peptide 8; Pep9: peptide 9; SLA: Leishmania antigenic extract.
The AUC values of each peptide and SLA were calculated after the ELISA experiments, using serum samples from VL (n = 30), VL/HIV-coinfected (n = 25) and HIV-infected (n = 20) patients. In addition, samples from healthy individuals living in an endemic region of VL (n = 25), as well as from those diagnosed with Chagas disease (n = 15), leprosy (n = 10), tuberculosis (n = 10) and malaria (n = 10), were collected. The confidence interval (95% CI) and P values were calculated, and the results are shown here.
Table 3. Diagnostic evaluation of the synthetic peptides and SLA for VL and HIV coinfection

NC, not calculated; Pep1, peptide 1; Pep2, peptide 2; Pep3, peptide 3; Pep4, peptide 4; Pep5, peptide 5; Pep6, peptide 6; Pep7, peptide 7; Pep8, peptide 8; Pep9, peptide 9; SLA, Leishmania antigenic extract.
Serum samples of patients with VL (n = 30), VL/HIV-coinfected (n = 25), HIV-infected (n = 20), Chagas disease (n = 15), leprosy (n = 10), tuberculosis (n = 10) and malaria (n = 10) were used. Samples from healthy individuals living in an endemic region of VL (n = 25) were also used in the ELISA experiments to calculate the sensitivity (Se), specificity (Sp), confidence interval (95% CI), positive predictive value (PPV), negative predictive value (NPV), likelihood ratio (LR) and Youden index (Y).
Bioinformatics assays
A three-dimensional (3D) alignment of the nine identified epitopes against L. infantum proteins was performed using PepSurf software (http://pepitope.tau.ac.il/), and results showed that three proteins had a high probability to contain these conformational sequences: trypanothione reductase (ID: 2JK6_A), with Pep1, Pep2, Pep3, Pep4 and Pep7; glyoxalase II (ID: 2P18_A), with Pep4 and Pep5 and tyrosine aminotransferase (ID: 4IX8_A), with Pep1, Pep2, Pep6 and Pep9 (Table 4). In addition, Pep8 did not present significant similarity with any L. infantum protein. In this context, a schematic representation of the location of Pep2, Pep3 and Pep4 in the amino acid sequence of the trypanothione reductase protein is also shown (Fig. 2).

Fig. 2. 3D representation of the L. infantum trypanothione reductase protein and location of Pep2, Pep3 and Pep4. The Pepitope server was used to predict the location of the epitopes in the protein's 3D structure. The amino acid sequences of Pep2 (A), Pep3 (B) and Pep4 (C) are numbered and shown. The equivalent amino acids are represented in white (match), the incompatibilities are shown in yellow (mismatch) and gaps where the absence of amino acids was verified are shown in pink (in match). A list containing the amino acids that make up the selected peptide is shown on the left (cluster).
Table 4. Identification of the Leishmania infantum proteins containing the conformational epitopes selected by phage display

Pep1, peptide 1; Pep2, peptide 2; Pep3, peptide 3; Pep4, peptide 4; Pep5, peptide 5; Pep6, peptide 6; Pep7, peptide 7; Pep9, peptide 9.
Bioinformatics assays were performed to identify parasite proteins where the conformational epitopes could be located. Results are shown here, where the protein name and identity, as well as the selected peptide, are indicated. Pep8 showed no similarity with any L. infantum protein sequence.
Prognostic evaluation of the selected epitopes
With serological data showing better diagnostic performance for Pep2, Pep3 and Pep4, these antigens were also tested in VL patient sera before and 6 months after treatment. Results showed that the anti-peptide serological reactivity declined by significant levels after the patient's treatment, as compared to the values found before treatment (Fig. 3). By contrast, using SLA as an antigen, a similar humoral reactivity was observed when samples collected before and after treatment were tested, thus suggesting that such an antigenic preparation is not suitable as a prognostic marker for VL.

Fig. 3. Post-therapeutic serological follow-up in VL patients. ELISA experiments were conducted using Pep2, Pep3 and Pep4 against serum samples collected from VL patients (n = 8) before and 6 months after treatment, as well as against L. infantum SLA. Levels of IgG antibodies were measured and the individual OD values are shown. The white and grey circles indicate the mean plus standard deviation of the OD values of the samples collected before and after treatment, respectively (A). In addition, the ratio between antibody levels before and after treatment was also calculated and data are shown (B). *** indicates a statistically significant difference in relation to the SLA antigen (P < 0.0001). Pep2: peptide 2; Pep3: peptide 3; Pep4: peptide 4; SLA: Leishmania antigenic extract.
Discussion
The VL/HIV coinfection is endemic in several countries around the world, and diagnostic tests used to identify such cases are not suitable, since low sensitivity tends to be found in coinfected patient samples (Cota et al., Reference Cota, Sousa, Demarqui and Rabello2012; Silva et al., Reference Silva, Brandão, Colovati, Sousa, Lima, Dorta, Ribeiro-Dias, Costa, Costa and Oliveira2018). In this context, there is a need to identify more sensitive antigens to be used in the diagnosis of VL and VL/HIV coinfection. Phage display is an in vitro selection strategy in which a peptide, protein or antibody is fused to a coat protein of phage capsid, which is displayed together with a fusion protein on the exogenous surface of the capsid (Alfaleh et al., Reference Alfaleh, Alsaab, Mahmoud, Alkayyal, Jones, Mahler and Hashem2020). This technique has been applied to identify novel vaccine candidates and/or diagnostic targets against a variety of diseases, such as leishmaniasis (Costa et al., Reference Costa, Lima, Chávez-Fumagalli, Menezes-Souza, Martins, Duarte, Lage, Lopes, Lage, Ribeiro, Andrade, Magalhães-Soares, Soto, Tavares, Goulart and Coelho2014; Toledo-Machado et al., Reference Toledo-Machado, Avila, Nguyen, Granier, Bueno, Carneiro, Menezes-Souza, Carneiro, Chávez-Olórtegui and Fujiwara2015a, Reference Toledo-Machado, Bueno, Menezes-Souza, Machado-de-Avila, Nguyen, Granier, Bartholomeu, Chávez-Olórtegui and Fujiwara2015b; Carvalho et al., Reference Carvalho, Costa, Lage, Ramos, Santos, Ribeiro, Dias, Salles, Lima, Carvalho, Dias, Alves, Franklin, Silva, Duarte, Menezes-Souza, Roatt, Chávez-Fumagalli, Goulart, Teixeira and Coelho2019). In this context, in the current study, the phage display technology applying a subtractive selection strategy was performed, aiming to identify new diagnostic targets for VL and VL/HIV coinfection.
VL is an opportunistic infection in HIV-infected patients, and this coinfection presents a relevant clinical role in endemic regions, since patients usually present higher duration time for the onset of VL, as well as a lower therapeutic response against disease (Lindoso et al., Reference Lindoso, Moreira, Cunha and Queiroz2018). In addition, a dysfunction of T-cell and B-cell responses hampers the antibody production, causing lower sensitivity in the diagnostic tests (Silva et al., Reference Silva, Brandão, Colovati, Sousa, Lima, Dorta, Ribeiro-Dias, Costa, Costa and Oliveira2018). Few studies have evaluated these tests for VL/HIV patients, mainly due to the lack of a gold standard. Cota et al. (Reference Cota, Sousa, Demarqui and Rabello2012) showed that the DAT and immunoblotting presented a sensitivity of 81.0 and 84.0%, respectively, to diagnose VL/HIV, which were better when compared to the use of ELISA and immunofluorescence antibody tests. Kassa et al. (Reference Kassa, Abdellati, Cnops, Bremer-Hinckel, Yeshanew, Hailemichael, Vogt, Adriaensen, Mertens, Diro, Van Griensven and Van den Bossche2020) evaluated the diagnostic efficacy of distinct commercial tests in HIV-coinfected Ethiopian patients. The authors showed that the sensitivity decreased in the VL/HIV-coinfected group, with some tests being more affected than others, thus suggesting that the performance of these commercial diagnostic kits is variable and sub-optimal, and that improvement in their sensitivity and specificity will lead to a better diagnostic efficacy.
Compared to the use of recombinant proteins, synthetic peptides can increase the diagnostic performance in immunological assays, since cross-reactivity with other undesired epitopes will be lower due to their exclusion. In addition, peptides can maintain the relative spatial structure and biological activity with high specificity, low false-negative rates and an easy clinical application (Meloen et al., Reference Meloen, Puijk, Langeveld, Langedijk and Timmerman2003). Therefore, such antigens have represented a valuable contribution to laboratory diagnoses of distinct diseases, such as leishmaniasis (Costa et al., Reference Costa, Penido, Santos, Doro, Freitas, Michalick, Grimaldi, Gazzinelli and Fernandes2012, Reference Costa, Salles, Santos, Ramos, Lima, Lima, Portela, Chávez-Fumagalli, Duarte, Menezes-Souza, Machado-de-Ávila, Silveira, Magalhães-Soares, Goulart and Coelho2017). The epitopes selected by phage display are of conformational nature (Xin et al., Reference Xin, Jinyan, Shengfa, Yuanyuan and Hongbing2014), which consists of discontinuous amino acids present in a target antigen, which in turn combine with the antigen binding site of the antibody molecule, and then simulate the characteristics of an epitope. A whole protein, in addition to containing desired epitopes (Gazarian et al., Reference Gazarian, Rowlay, Gazarian, Vazquez-Buchelli and Hernández-Gonzáles2012), may also contain cross-reactivity epitopes for diagnosis, inhibitory epitopes and/or auto-antigen epitopes, hampering the specificity of the tests (Faria et al., Reference Faria, Veloso, Coura-Vital, Reis, Damasceno, Gazzinelli and Andrade2015). In this sense, the use of well-defined epitopes, such as synthetic peptides, could be beneficial to improving the sensitivity and specificity of the diagnosis of VL and VL/HIV coinfection.
Serological results obtained here showed that three of the nine selected epitopes, Pep2, Pep3 and Pep4, presented 100% sensitivity and specificity to diagnose VL and VL/HIV coinfection. Otherwise, SLA presented sensitivity and specificity values of 92.7 and 62.2%, respectively, suggesting a lower diagnostic performance as compared to these selected peptides. In one study, a promastigote crude antigenic preparation was able to identify 80% of VL patient sera by means of ELISA experiments, although high cross-reactivity was observed when patient samples presenting malaria and Chagas disease were used (Fargeas et al., Reference Fargeas, Hommel, Maingon, Dourado, Monsigny and Mayer1996). The authors also tested single peptides, and found better sensitivity and specificity values than the crude antigenic preparation, leading to the suggestion that the combination of peptides could result in higher diagnostic accuracy for VL. However, in this study, samples from VL/HIV-coinfected patients were not tested. Other more recent studies evaluating synthetic peptides as antigens for the VL diagnosis did not test this type of serum class in their serological panels (Costa et al., Reference Costa, Salles, Santos, Ramos, Lima, Lima, Portela, Chávez-Fumagalli, Duarte, Menezes-Souza, Machado-de-Ávila, Silveira, Magalhães-Soares, Goulart and Coelho2017; Ejazi et al., Reference Ejazi, Bhattacharyya, Choudhury, Ghosh, Sabur, Pandey, Das, Das, Rahaman, Goswami and Ali2018; Machado et al., Reference Machado, Ramos, Oliveira-da-Silva, Santos, Ludolf, Tavares, Costa, Lage, Steiner, Chaves, Chávez-Fumagalli, Magalhães-Soares, Silveira, Napoles, Tupinambás, Duarte, Machado-de-Ávila, Bueno, Fujiwara, Moreira, Rocha, Caligiorne and Coelho2020). In this context, data presented here using the Pep2, Pep3 and Pep4 suggest that such antigens present a high efficacy in the diagnosis of VL, as well as in VL/HIV coinfection cases, and could be used in future studies to diagnose both clinical conditions.
A 3D alignment performed in the amino acid sequences of the selected phage exposed with Leishmania proteins showed the identification of the L. infantum trypanothione reductase protein as the target possibly containing the three epitopes that presented the best serological response for VL and VL/HIV coinfection. This protein is an essential enzyme and is of the Trypanasomatidae family, which has been validated as a drug target in Leishmania and Trypanosoma, since its downregulation causes strong impairment in the parasite's infectivity (Battista et al., Reference Battista, Colotti, Ilari and Fiorillo2020). In addition, such drugs as antimonials interfere with trypanothione metabolism and inhibit the trypanothione reductase, suggesting that this protein could be a therapeutic option for the treatment against such diseases (Ilari et al., Reference Ilari, Genovese, Fiorillo, Battista, De Ionna, Fiorillo and Colotti2018). Moreover, a significant amino acid sequence homology of trypanothione reductase proteins from different sources makes it a valuable target for developing a single, broad spectrum drug active against all Trypanosomatides (Beig et al., Reference Beig, Oellien, Garo, Noack, Krauth-Siegel and Selzer2015), in addition to the fact that they are specific to the Trypanasomatidae family, showing low similarity to human protein sequences, making then suitable candidates for the diagnosis of these diseases (Holloway et al., Reference Holloway, Charman, Fairlamb, Brun, Kaiser, Kostewicz, Novello, Parisot, Richardson, Street, Watson and Baell2009).
Limitations of this study include the absence of a higher serological panel, as well as the use of other diagnostic platforms that incorporate the best selected peptides, such as those used in immunochromatographics. However, this study can be considered the first to employ the phage display technology and antibodies from VL, HIV-infected and VL/HIV-coinfected patients to select novel diagnostic targets, such as synthetic peptides, and test them for the serodiagnosis of VL and VL/HIV coinfection.
Author contributions
Conceived and designed the experiments: EAFC, FFR, LRG, PTA, VGF, ACSD, FL and GSVT. Performed the experiments: FFR, FL, ASM, TTOS, IAPG, ACSD, PTA, VGF, RSB, JAOS, TARR, DPL, VTM and CSF. Analysed the data: EAFC, FFR, LRG, FL, GSVT and MACF. Contributed reagents/materials/analysis tools: ATC, NSG, UT, MOCR, GFC, RTF and LLB. Wrote the paper: EAFC, LRG and FFR.
Financial support
This work was supported by grant MR/R005850/1 from the Medical Research Council (VAccine deveLopment for complex Intracellular neglecteD pAThogEns – VALIDATE), UK, and grant APQ-408675/2018-7 from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Brazil. The authors also thank the Brazilian agencies Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), CNPq and the Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) for the student scholarships.
Conflict of interest
The authors hereby declare that they have no conflicts of interest.
Ethical standards
The Human Research Ethics Committee from the Federal University of Minas Gerais (UFMG; Belo Horizonte, Minas Gerais, Brazil) approved the study, logged under protocol number CAAE-32343114.9.0000.5149. All patients have agreed to participate in the study, and those who chose not to participate had the same attention and medical care provided as did the enrolled participants, all of whom received the same treatment, follow-up and necessary care.