Introduction
Chronic tympanic membrane perforation with mucosal chronic otitis media is a common disease encountered in otology clinics. This disease can result in conductive hearing loss, tinnitus and middle-ear infection. Myringoplasty is a common otological procedure for treating mucosal chronic otitis media. However, there is controversy regarding the operation timing.
Most groups have suggested that ear discharge at the time of surgery results in middle-ear infection, a higher graft failure rate and adverse effects on hearing outcome, and recommend that myringoplasty be performed only when the ear has been dry for at least three months.Reference Zwierz, Haber, Sinkiewicz, Kalińczak-Górna, Tyra and Mierzwiński1–Reference Uyar, Keleş, Koç, Oztürk and Arbağ3 TosReference Tos4 and ArmstrongReference Armstrong5 reported that the results of myringoplasty were better for dry ears than for ears with discharge. Uyar et al.Reference Uyar, Keleş, Koç, Oztürk and Arbağ3 recommended medical management initially for ears with discharge, and advised that tympanoplasty only be performed when the ears have been dry for three months. Gersdorff et al.Reference Gersdorff, Garin, Decat and Juantegui2 suggested that if the ear remains wet, mastoidectomy should be combined with myringoplasty.
By contrast, some groups have proposed that ear discharge has little effect on surgical success, and that the presence of otorrhoea at the time of surgery is unrelated to the graft take rate.Reference Tan, Santa Maria, Eikelboom, Anandacoomaraswamy and Atlas6–Reference Fukuchi, Cerchiari, Garcia, Rezende and Rapoport8 A few groups have even reported that the graft success rate was higher in wet than in dry ears.Reference Caylan, Titiz, Falcioni, De Donato, Russo and Taibah9 Mishiro et al.Reference Mishiro, Sakagami, Kondoh, Kitahara and Kakutani7 reported that mastoidectomy can be avoided in patients undergoing tympanoplasty for perforated chronic otitis media, even if the ear is infected.
Nevertheless, early comparative studies of myringoplasty in dry and wet ears were mainly performed in paediatric patients,Reference Zwierz, Haber, Sinkiewicz, Kalińczak-Górna, Tyra and Mierzwiński1–Reference Tan, Santa Maria, Eikelboom, Anandacoomaraswamy and Atlas6 and there have been few reports on adults. The major differences between adults and children are the incomplete Eustachian tube development and impact of adenoidal hypertrophy in children.
Eustachian tube dysfunction has been reported to result in a higher graft failure rate.Reference Tos4,Reference Çayir and Kayabaşi10 In addition, ear discharge in chronic otitis media cases may continue for months to years, with increasing hearing impairment, and some patients may develop new infections of the middle ear while waiting for the ear to become dry, even experiencing fungal otitis externa. Early closure of the perforation and recovery of the normal physiological function of the middle ear would help to reduce the risks of exogenous infection and allergen stimulation, and improve Eustachian tube function. This study was performed to compare the graft success rate and hearing gain between wet and dry ears after endoscopic cartilage myringoplasty performed to treat mucosal-type chronic otitis media.
Materials and methods
The study protocol was reviewed and approved by the Institutional Ethical Review Board of Yiwu Central Hospital. Informed consent was obtained from all participants.
This case series study was carried out between January 2012 and December 2015. The patients were selected from the department of otolaryngology after proper history taking and examination.
The inclusion criteria were as follows: (1) chronic perforation with mucosal chronic otitis media, with or without mucoid or mucopurulent discharge or oedematous middle-ear mucosa; (2) temporal bone computed tomography (CT) demonstrated good pneumatisation of mastoid bone, or soft density shadows in the mastoid and tympanic antrum; and (3) no suspicion of ossicular chain defect, and conductive hearing loss no greater than 40 dB at any frequency.
The exclusion criteria were as follows: (1) paediatric patient; (2) ossicular chain abnormalities; (3) previous mastoidectomy; (4) cholesteatoma detected using CT or magnetic resonance imaging and diffusion-weighted imaging when necessary, or found on intra-operative exploration; and (5) the presence of fungal otitis externa.
Patients were divided into dry ear and wet ear groups based on the status of middle-ear mucosa. Ears with mucoid or mucopurulent discharge or oedematous middle-ear mucosa were defined as having wet ears; otherwise, the ears were defined as dry. Perforations were categorised according to the proportion of the perforation relative to the whole eardrum, as follows: small – up to one-third of the tympanic membrane area; medium – between one-third and two-thirds of the tympanic membrane area; or large – more than two-thirds of the tympanic membrane area.
The pure tone average was calculated as the mean of the pure tone hearing thresholds at 0.5, 1, 2 and 4 kHz. The air–bone gap was defined as the mean of the differences between the air conduction thresholds and the bone conduction thresholds at 0.5, 1, 2 and 4 kHz, calculated pre-operatively and at three months post-operatively.
Surgical techniques
The patients were placed in the supine position, with their head inclined 30° upward and turned slightly toward the opposite side. Video equipment was placed on the opposite side of the surgeon. During endoscopic cartilage myringoplasty, the operative field was draped using a fenestrated sheet. The perforation edges were visualised and de-epithelialised with an angled pick under a 0° rigid endoscope.
A cartilage graft with a one-sided perichondrium was harvested through a 1 cm incision medial to the free border of the tragus. The perichondrium was separated and moulded into a cuff shape. The cartilage portion of the graft was fashioned to be slightly larger than the perforation. The cuff of perichondrium was maintained around, and was slightly larger than, the cartilage graft. The tragal cartilage portion of the graft was not thinned out.
Under endoscopy, the middle ear was washed using 1 per cent povidone iodine solution and 0.9 per cent saline solution, and ofloxacin ear drops were administered. Any oedematous middle-ear mucosa was not removed. The middle ear was tightly packed with biodegradable NasoPore® dressing (soaked in antibiotic ointment and dexamethasone) to the level of the perforation. The tubal orifice was supported to prevent medialisation due to the pressure exerted by sniffing.
The cartilage graft was pushed through the perforation to allow occlusion, similar to an inlay graft, with a medial layer of perichondrium. In a few perforations, a notch was made in the cartilage to accommodate the exposed malleus handle, but not the perichondrium. The perichondrial cuff was placed over the edges of the perforation and malleus handle.
The external auditory canal was first packed with NasoPore, followed by gauze soaked with antibiotic ointment, until the tragus incision was reached. The tragus incision was not sutured, and a small dressing was applied to cover the auricle.
Post-operative follow up
All patients were prescribed two weeks’ oral antibiotics (to prevent post-operative infection). Each patient was scheduled for regular follow-up visits at two and three weeks, and at one, three and six months, post-operatively. Endoscopy was performed at all visits.
The packing gauze soaked in antibiotic ointment at the opening of the external auditory canal was removed at 14 days post-operatively, and biodegradable NasoPore fragments were aspirated from the external auditory canal at 3 weeks post-operatively, thus allowing visualisation of the graft.
Pure tone audiograms were recorded at six months post-operatively. The primary outcome was the graft success rate at six months post-operatively. Persistent discharge, residual perforation and re-perforation of the graft at six months post-operatively were considered indicators of graft failure. The secondary outcome was hearing gain.
Statistical analysis
Statistical analyses were performed using SPSS software, version 20 (IBM, Armonk, New York, USA). The data are expressed as means (with standard deviations) and percentages. The chi-square test was used for the comparison of groups and recovery rates. Data normality was examined using the Kolmogorov–Smirnov test. The Wilcoxon's and Mann–Whitney U tests were used for non-parametric variables, whereas independent and paired samples t-tests were used for parametric variables. In all analyses, p < 0.05 was taken to indicate statistical significance.
Results
Demographic data
A total of 107 patients with unilateral chronic perforation with chronic otitis media were included in this study. Sixty-seven of the patients were female and 40 were male. The left ear was affected in 58 patients and the right ear in 49 patients (107 ears). Seventy-eight patients had dry ears and 29 patients had wet ears. The patients’ mean age and sex, and the duration, size and position of perforations, were matched among the two groups (Table 1). Of the 29 patients with wet ears, 11 had mucoid discharge and 18 had mucopurulent discharge.
Table 1. Demographic data for dry ear and wet ear groups

SD = standard deviation. *Chi-square test; †t-test
Graft take rate
At six months, the graft success rates were 85.9 per cent (67 out of 78) in dry ear cases and 86.2 per cent (25 out of 29) in wet ear cases; this difference was not significant (p = 0.583). Of the 78 dry ears, 6 had residual perforations, 2 had displaced grafts, and 3 ears failed to heal because of middle-ear infection or fungal otitis externa. Of the 29 wet ears, all 11 with mucoid discharge healed completely, representing a success rate of 100 per cent (Figures 1 and 2). Of the 18 patients with mucopurulent discharge, 2 ears failed to heal because of middle-ear infection or fungal otitis externa, and the cartilage graft collapsed in 2 ears resulting in a gap between the cartilage graft and residual eardrum. The graft success rate was 77.8 per cent in patients with mucopurulent discharge.
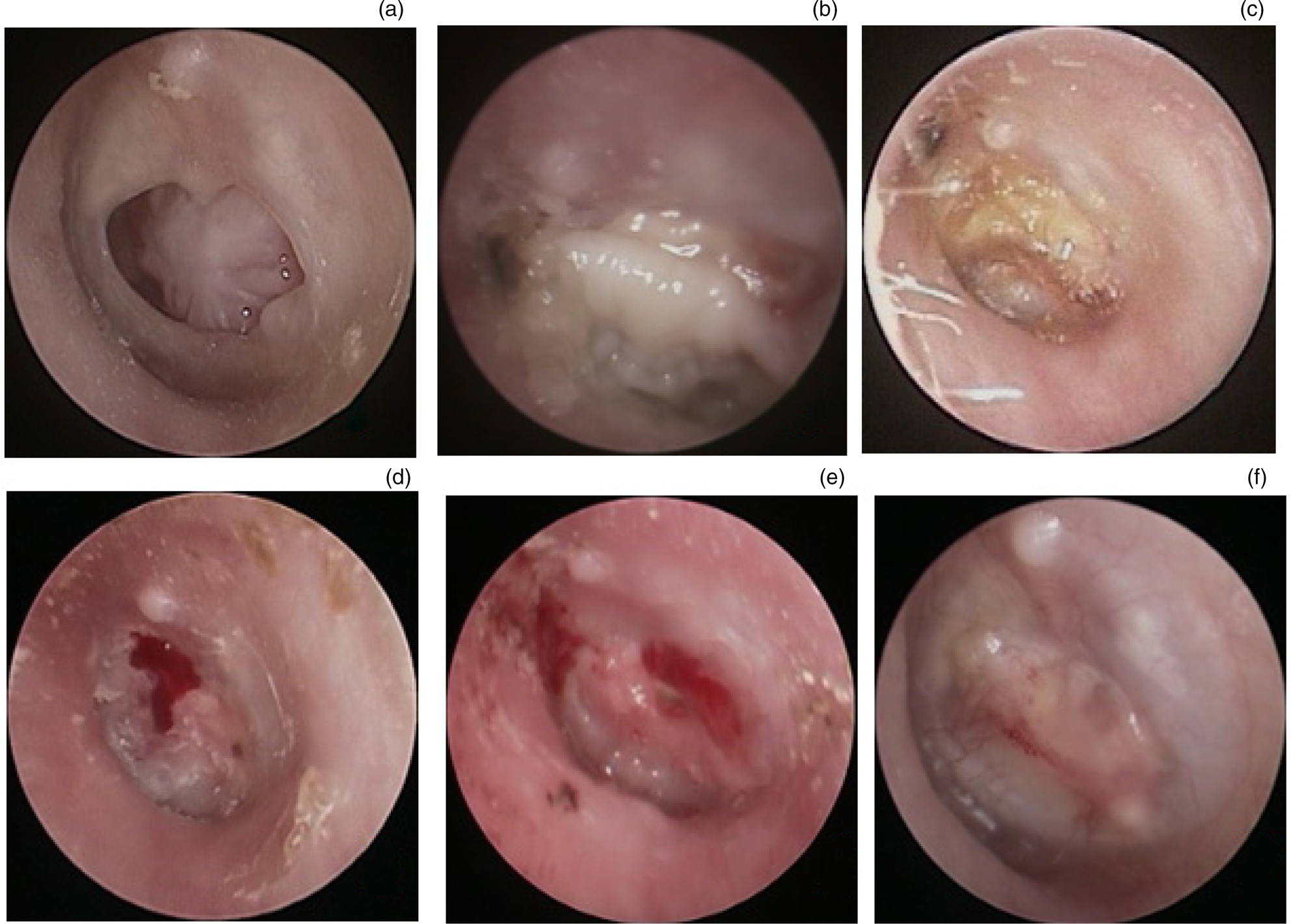
Fig. 1. A 37-year-old female with a left-sided, mucoid, wet tympanic membrane perforation: (a) pre-operation; (b) at 1 month post-operatively; (c) at 2 months post-operatively; (d) at 3 months post-operatively; (e) at 4 months post-operatively; and (f) at 6 months post-operatively.

Fig. 2. A 62-year-old male with left-sided, mucoid, wet tympanic membrane perforations: (a) pre-operation; (b) at 1 month post-operatively; and (c) at 3 months post-operatively.
Hearing gain
In the dry ear group, the mean pre-operative air–bone gap was 30.84 ± 6.81 dB, whereas the mean post-operative air–bone gap was 17.22 ± 9.10 dB; this difference was statistically significant (p < 0.001) (Table 2). In the wet ear group, the mean pre-operative air–bone gap was 29.81 ± 9.61 dB, whereas the mean post-operative air–bone gap was 18.14 ± 9.75 dB; this difference was also statistically significant (p < 0.001). The mean post-operative hearing improvement in the dry ear group was 13.41 ± 8.34 dB, and that in the wet ear group was 12.95 ± 9.73 dB; the difference between the two groups was not statistically significant (p = 0.472).
Table 2. Pre- and post-operative air–bone gap data for dry ear and wet ear groups

Pre-op = pre-operatively; SD = standard deviation; post-op = post-operatively
Complications
There were no complications such as sensorineural hearing loss, taste alteration, facial nerve palsy, vertigo or tinnitus, and no problems with the tragal incision during the follow-up period.
Graft displacement occurred in two of the dry ears. Of the 18 patients with mucopurulent discharge, the cartilage graft collapsed in 2 ears (Figure 3), and retraction of the tympanic membrane occurred in 1 ear. However, of the 11 ears with mucoid discharge, 3 remained wet at 4 weeks post-operatively and became dry after 1 month of anti-allergic treatment (loratadine tablets).
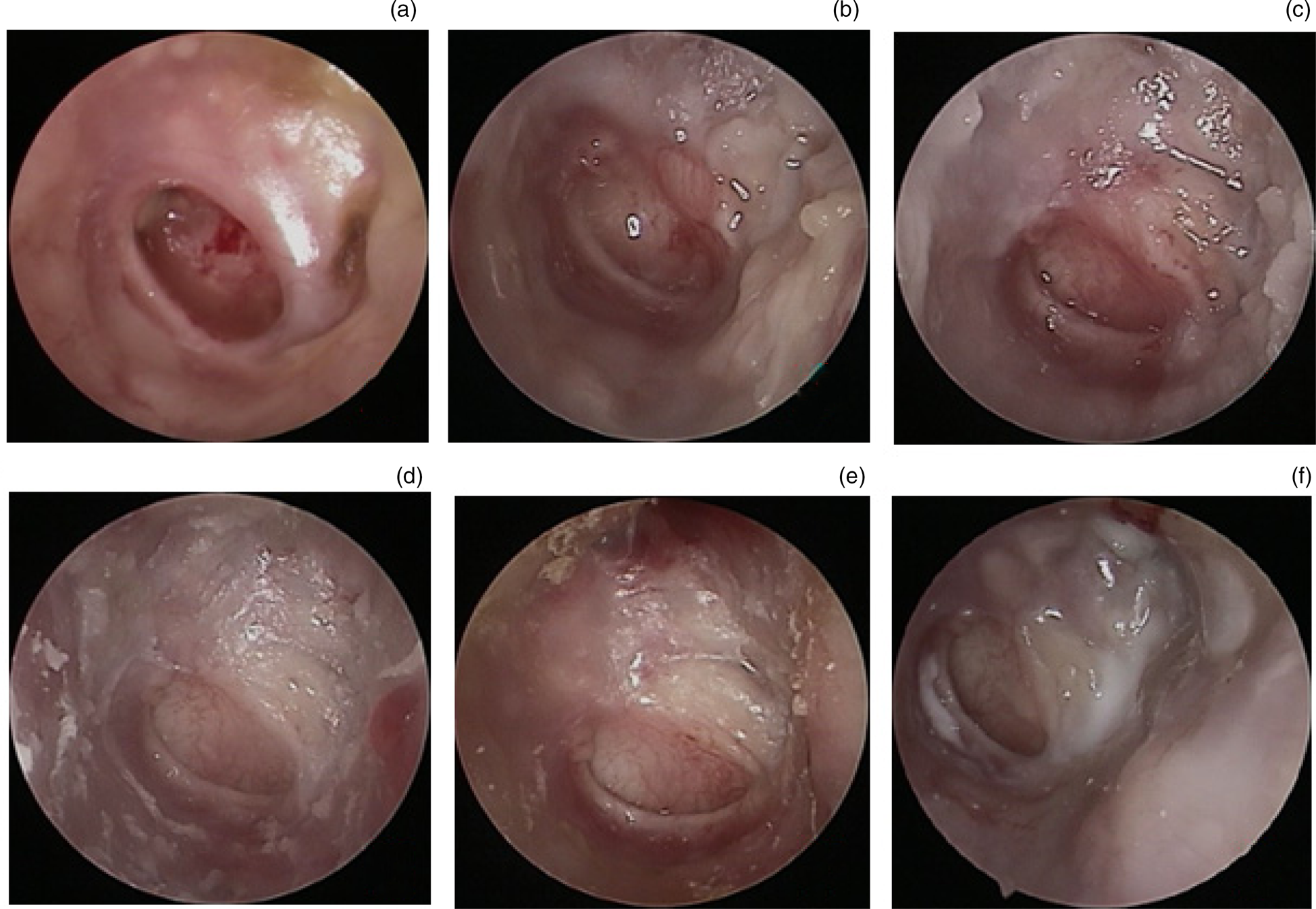
Fig. 3. A 77-year-old female with a left-sided, mucopurulent tympanic membrane perforation: (a) pre-operation; (b) at 1 month post-operatively; (c) at 2 months post-operatively; (d) at 3 months post-operatively; (e) at 4 months post-operatively; and (f) at 6 months post-operatively.
Discussion
There has long been debate regarding the appropriate status of middle-ear mucosa for the treatment of tympanic membrane perforation with chronic otitis media using myringoplasty. Most groups have suggested that ears need to be dry for at least three months or that mastoidectomy should be performed simultaneously.Reference Zwierz, Haber, Sinkiewicz, Kalińczak-Górna, Tyra and Mierzwiński1–Reference Uyar, Keleş, Koç, Oztürk and Arbağ3 However, these studies concentrated mainly on paediatric cases, and the observations may have been the result of incomplete Eustachian tube development in children. Wet middle ears in children may have further aggravated Eustachian tube dysfunction, and thereby increased rates of graft extrusion.
Nevertheless, other groups have reported that the inflammatory status of the middle ear did not affect graft success rate, and the presence of discharge at the time of surgery had no effect on graft success rate either.Reference Tan, Santa Maria, Eikelboom, Anandacoomaraswamy and Atlas6–Reference Fukuchi, Cerchiari, Garcia, Rezende and Rapoport8 These groups have suggested that mastoidectomy can be avoided during tympanoplasty performed to treat perforated chronic otitis media, even in cases in which the ear is infected. Two recent studies by Onofre et al.Reference Onofre, Ha, Yang, Lee, Lee and Yoo11 and He et al.Reference He, Shou, Hsieh, Wang, Wang and Han12 revealed that the post-operative re-perforation rate was not positively related to the presence of soft tissue in the antrum. By contrast, a few groups have suggested that wet ears increased the graft success rate.Reference Caylan, Titiz, Falcioni, De Donato, Russo and Taibah9
In this study, the graft success rate was not significantly different between the dry ear and wet ear groups (85.9 per cent (67 out of 78) vs 86.2 per cent (25 out of 29), respectively, p = 0.583) at the six-month follow up. In addition, there was no significant difference in hearing improvement between the two groups. This study further demonstrated that the status of the middle-ear mucosa did not affect the post-operative outcome of endoscopic cartilage myringoplasty.
• Whether the ear was wet or dry did not affect graft success rate or hearing gain following endoscopic cartilage myringoplasty
• Ears exhibiting mucopurulent discharge were associated with increased myringoplasty failure and graft collapse
• Ears exhibiting mucoid discharge were associated with a higher graft success rate
• The use of anti-allergic agents may prevent the occurrence of post-operative wet ears
• Mucopurulent discharge may trigger cartilage graft collapse and tympanic membrane retraction
In a study of 268 ears over a 10-year period, Mills et al.Reference Mills, Thiel and Mills13 reported no significant difference in closure rate between actively discharging (either intermittent or persistent) and inactive ears. Overall, the healing rate of chronic perforation was similar to that when acute tympanic membrane perforation was repaired. In the past, treatment of acute perforation mainly involved spontaneous healing via keeping the ear dry and prohibiting the use of ear drops. Although some recent studies indicated that the healing of wet perforations was faster than that of the dry perforations,Reference Lou, Tang and Yang14,Reference Lou and Lou15 the topical application of ear drops was reported to accelerate eardrum healing and to improve the healing rate.Reference Lou, Lou, Tang and Xiao16 We feel that early eardrum repair, and clearing of the foci of infection and irreversible granulation tissue, may maintain the normal physiological function of the middle ear and return pathological middle-ear mucosa to the normal state.
Although some studies have suggested that wet ear status does not affect, and can even increase, the graft success rate, the definition and assessment of a wet ear were not clarified in most previous studies. Whether the ear with mucoid or mucopurulent discharge had a better success rate was unclear. Shankar et al.Reference Shankar, Virk, Gupta, Gupta, Bal and Bansal17 reported that whether the discharge was mucoid or mucopurulent had no influence on graft uptake success rate; however, the sample size of the mucoid discharge group was significantly larger than that of the mucopurulent group (28 vs 7 ears, respectively). In addition, there is no objective way of quantifying the degree of mucosal disease. We found intra-operatively that the disease was localised in some patients, but involved the whole middle ear in others; some patients also exhibited mild thickening of the mucosa, whereas others exhibited partial obliteration of the middle-ear space. Two studies, by Nagle et al.Reference Nagle, Jagade, Gandhi and Pawar18 and Sharma,Reference Sharma, Mishra and Patel19 only included patients with mucoid discharge.
The current study included patients with mucoid and mucopurulent discharge; the results revealed that the success rate for ears with mucoid discharge was 100 per cent and that for mucopurulent discharge was 77.8 per cent. The success rate for ears with mucoid discharge (100 per cent) was significantly higher than that for dry ears (85.9 per cent) and ears with mucopurulent discharge (77.8 per cent). It is possible that the nature of discharge may affect the graft failure rate. A prospective study by Kotecha et al. reviewing 1070 individuals revealed that failure rates in patients with dry ears, or ears with mucoid, serous or purulent discharge, were 17.7 per cent, 17.1 per cent, 11.8 per cent and 17.2 per cent, respectively.Reference Kotecha, Fowler and Topham20 In a study of traumatic tympanic membrane perforation, cases with serosanguinous discharge exhibited a significantly improved closure rate and shorter time to closure compared to cases with dry perforation.Reference Lou, Tang and Yang14
It is possible that ears with mucopurulent discharge had a relatively increased graft failure rate. The presence of pre-operative infection and intra-operative remnant foci of infection would increase the possibility of graft infection post-operatively. Infection is a common cause of graft failure. In this study, although we only included wet ears with mucopurulent discharge continuing for at least two weeks (so-called ‘subacute infection’), the post-operative infection rate in patients with mucopurulent discharge was higher than that in the dry ear group (11 per cent (2 out of 18) vs 3.8 per cent (3 out of 78), respectively). Noh and LeeReference Noh and Lee21 reported that any pre-operative negative cultures may be false negatives, and post-operative discharge was significantly more prevalent among patients with wet middle-ear mucosa pre-operatively than among those with dry ears.
In addition, mucopurulent discharge can accelerate the liquidation of support material, thereby causing loss of support and the collapse of graft material, resulting in a gap between the cartilage graft and residual eardrum. Cartilage graft collapse was observed in 2 ears among 18 patients with mucopurulent discharge, whereas no cartilage grafts collapsed in the dry ear group in this study. Mucopurulent discharge can also cause the proliferation of granulation tissue in the middle-ear mucosa, thus obstructing the aeration function of the middle ear, resulting in retraction of the tympanic membrane. Of the 11 ears with mucoid discharge in this study, 3 remained wet at four weeks post-operatively and became dry after anti-allergic treatment for one month.
Post-operative ear discharge may have resulted from non-infective causes, such as allergies or Eustachian tube dysfunction in the cases with pre-operative wet middle-ear mucosa. Thus, the assessment of the nature of the discharge is highly subjective, and there is a risk that the findings will be influenced by observer bias.
Although mucopurulent discharge was not a contraindication for endoscopic myringoplasty, caution is required when performing surgery in patients with an acute infection of the middle ear. However, for mucopurulent discharge with subacute infection, the unhealthy granulation tissue of the middle ear and foci of infection should be cleared, thus preserving the swollen mucosa. Additionally, intra-operative washing with saline and antibiotic solutions should be performed, thereby maintaining the aeration function between the Eustachian tube, middle ear and antrum. The support material soaked in dexamethasone was placed in the middle ear during surgery, whereas antibiotics and anti-allergic agents were used after surgery.
This study was limited by the unbalanced sample sizes of the two groups. In particular, only 11 patients had mucoid discharge, which could have affected the data analysis. In addition, this was not a randomised study. Finally, an objective assessment of the nature of each case of discharge was difficult.
Acknowledgement
This study was supported by the Science and Technology Agency of Yiwu City, China (grant number: 2018–3–76).
Competing interests
None declared







