Syncope is a common problem in children and adolescents. Reference Friedman and Alexander1 Syncope is defined as transient loss of consciousness due to cerebral hypoperfusion, characterised by a rapid onset, short duration, and spontaneous complete recovery. Reference Brignole, Moya and de Lange2 The vast majority of paediatric syncope is caused by neurally mediated hypotension leading to vasovagal syncope. The last one is characterised by systemic hypotension resulting in inadequate cerebral blood flow from a reflex-mediated combination of inappropriate vasodilatation and bradycardia. Reference Anderson, Willis, Lancaster, Leonard and Thomas3 Paediatric patients with vasovagal syncope have lower health-related quality of life in comparison to healthy children. Reference Grimaldi Capitello, Fiorilli, Placidi, Vallone, Drago and Gentile4,Reference Kovalchuk5 A searching and better understanding of new pathophysiological mechanisms of vasovagal syncope development is essential if the correct diagnostic and treatment strategies are to be implemented.
Achieving an optimal status of folate is an urgent priority because of its established role in the prevention of neural tube defects and a potential protective role in cardiovascular disease. Reference Viswanathan, Treiman, Kish-Doto, Middleton, Coker-Schwimmer and Nicholson6,Reference Kerr, Livingstone and Bates7 Particularly folate (vitamin B9), pyridoxine (vitamin B6), and cobalamin (vitamin B12) contribute essentially to the maintenance of a healthy nervous system. Their importance is highlighted by many neurological diseases related to deficiencies in one or more of these vitamins, but they can improve certain neurological conditions even without a (proven) deficiency. Reference Calderón-Ospina and Nava-Mesa8 The shared metabolism between folate and vitamin B12 suggests that deficiencies in one vitamin may alter the metabolism of the other. Reference Moretti and Caruso9 This is perhaps related to the roles that vitamin B12 plays in myelination, or in the synthesis of methionine from homocysteine in combination with folic acid. Reference Black10
Some studies have shown a relationship between folate, vitamin B12, homocysteine and various diseases such as epilepsy, cognitive disorders, neurodegenerative diseases, autism spectrum disorder, schizophrenia, affective disorder, depression, and attention deficit hyperactivity disorders. Reference Nawaz, Khattak, Khan, Nangyal, Sabri and Shakir11–Reference Altun, Şahin, Belge Kurutaş and Güngör13 These observations can be explained by the important role of pyridoxine, folate, vitamin B12, and homocysteine in the carbon transfer metabolism that is necessary for the production of serotonin, other monamine neurotransmitters, and catecholamines. Reference Altun, Şahin, Belge Kurutaş and Güngör13 Several reports have indicated that through various molecular mechanisms, hyperhomocysteinaemia is toxic for the brain. Reference Moretti and Caruso9,Reference Boldyrev, Bryushkova, Mashkina and Vladychenskaya14 Hyperhomocysteinaemia also causes cardiovascular diseases due to effects on autonomic nerve function, increased oxidative stress, promotion of inflammation, proliferation of smooth muscle cells, and injury to vascular endothelium. Reference Ganguly and Alam15,Reference Pushpakumar, Kundu and Sen16
Several studies point out that vitamin B-12 deficiency may affect the sympathetic regulation of blood vessels and the autonomic nervous system, similar to the situation observed in vasovagal syncope. Reference Sanya, Tutaj, Brown, Goel, Neundörfer and Hilz17,Reference Kayali and Gökcebay18 Dysfunction of the sympathetic nervous system has been considered to be the main factor in vasovagal syncope and postural tachycardia syndrome. Reference Lambert and Lambert19 People who have vitamin B12 deficiency may present with neurological symptoms, pre-syncope and falling attacks. This may or may not occur without B-12 associated anaemia. Reference Ganjehei, Massumi, Razavi and Wilson20,Reference Usalp, Kemal and Yüksek21 Supplementation of Vitamin B12 in deficient patients presenting with suspected vasovagal syncope resulted in significant improvement in symptoms at 1 and 6 months of follow-up. Reference Parekh, Sastry, Narasimhan and Arora22
To the best of our knowledge, there has been no study that has shown a potential relationship between serum pyridoxine, folate, cobalamin, and homocysteine levels and vasovagal syncope in children. The aim of the current study was, therefore, to investigate serum pyridoxine, folate, cobalamin, and homocysteine levels in children presenting with vasovagal syncope and to analyse the correlation between them and main clinical parameters of vasovagal syncope to evaluate role of B vitamins and hyperhomocysteinaemia in the pathogenesis of vasovagal syncope. Such findings can be useful for searching a new management strategy for children with the diagnosis of vasovagal syncope.
Materials and methods
We studied 40 children, ages 8–17 years with a history of vasovagal syncope. For the diagnosis of vasovagal syncope was used diagnostic criteria of European Society of Cardiology (2018). Reference Brignole, Moya and de Lange2 Children enrolled in the study had to meet the following inclusion criteria: (1) as minimum 1 event of vasovagal syncope during last month, (2) normal response during active standing test, (3) absence of structural heart diseases and electrocardiography findings suggesting arrhythmic syncope, (4) absence of electroencephalography signs of epilepsy, (5) absence of any other evident aetiology for syncope, and (6) no concomitant acute or chronic disease including hypertension, overweight or obesity, anaemia, hypothyroidism, and renal dysfunction. The control group consisted of 24 healthy volunteers. All the children, including the control group, met the following inclusion criteria: absence of history of syncope, normal physical examination data, normal routine blood and urine analyses, absence of acute or chronic organic diseases including hypertension, overweight or obesity, anaemia, seizure, hypothyroidism, and renal dysfunction. This study was approved by the Ethics Committee of the Ivan Horbachevsky Ternopil National Medical University, and all participants gave their written informed consent before participation.
The main demographic and clinical characteristics of vasovagal syncope and control groups are presented in Table 1. There was no difference between the patient and control groups in terms of age or gender distribution. Vasovagal syncope and control groups were similar to each other according to body mass index, blood pressure, hemoglobin, and red blood count. It has helped to eliminate the influence of overweight, obesity, hypertension, and anaemia at the serum pyridoxine, folate, cobalamin, and homocysteine levels in research groups of children.
Table 1. Demographic, clinical and biochemical characteristics of patients

All parameters were presented as mean ± standard deviation except parameters cases and males/females which were denoted as numbers and percentages. Mann–Whitney U test was used for continuous variables, and chi-square test was used for categorical variables.
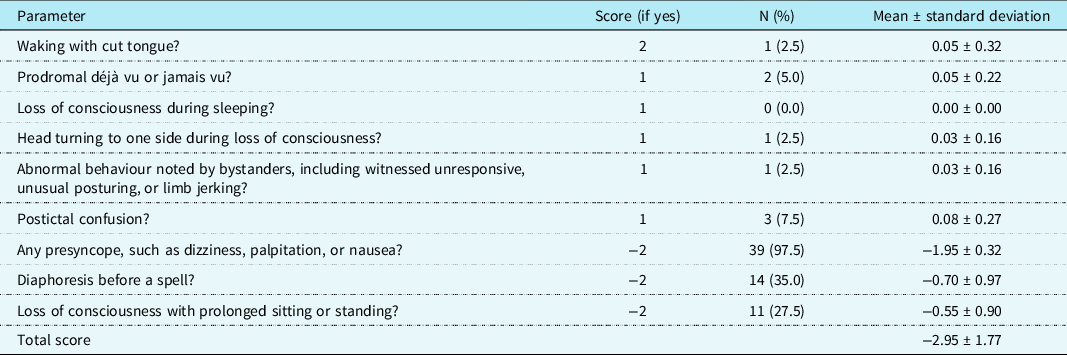
The patient’s history was carefully taken from all children presenting with vasovagal syncope: age at the first syncope; factors that preceded primary syncope; frequency, stereotypes, and serial syncope; trigger factors; methods to prevent syncope; clinical manifestations of the pre syncope, syncope, and post syncope symptoms; paraepileptic phenomena; hereditary factors. Calgary Syncope Seizure Score (Table 2) and Modified Calgary Syncope Seizure Score (Table 3) were used to differential diagnosis between vasovagal syncope, cardiac syncope, and epilepsy in paediatric patients. Reference Zou, Wang and Zhu23 Active standing test was used for all patients for excluding of orthostatic hypotension and postural orthostatic tachycardia syndrome. Reference Tanaka, Fujita and Takenaka24
Table 2. Prevalence of Calgary Syncope Seizure Score parameters in children with vasovagal syncope.

Table 3. Prevalence of Modified Calgary Syncope Seizure Score parameters in children with vasovagal syncope.
Heart rhythm recordings were conducted for 24-hour both in the patient and control groups using a 3-channel rhythm Holter monitorisation device (SDM3, Ukraine). After automated QRS detection and classification, very careful, direct visual confirmation of beat types and then verification of the edge values of the tachogram was performed manually. Ectopic beats and signal artifacts were corrected by interpolation with the previous and following R-R intervals. After editing, the beats files were analysed for indices of heart rate variability: standard deviations of the averages of the R-R intervals in all 5-min segments of R-R intervals (SDANN); the root of the 24-hours square; the proportion of adjacent normal R-R intervals <50 ms; the total power; very-low-frequency power; the low-frequency index; the high-frequency index; and low-frequency/ high-frequency ratio.
At the same day was conducted 24-hour Ambulatory Blood Pressure Monitoring. Studies were performed with a BAT41–2 device (Ukraine) using a protocol of European Society of Hypertension (2014). Reference Parati, Stergiou and O’Brien25 Automatic measurements were taken every 15 minutes during the day and every 30 minutes during the night.
Blood samples were taken from the study participants between 08.00 and 11.00. A sample with 5 ml of venous blood was obtained from the forearm of each subject and centrifuged at 3000 rpm for 3–5 min within 30 min. All of the samples were frozen at −80°C for 20 months until analysed. In our study, the serum levels of pyridoxine, folate, cobalamin, and homocysteine were measured by a quantitative sandwich enzyme immunoassay technique (ELISA) using a commercial kit (Monobind, USA) according to the manufacturer’s instructions at the scientific and clinical laboratory of Ivan Horbachevsky Ternopil National Medical University.
Optimal vitamin B6 status was defined as serum pyridoxal 5’-phosphate concentration >7,41 µg/L (>30 nmol/L). Serum pyridoxal 5’-phosphate level 7.41–4.94 µg/L (30–20 nmol/L) was estimated as suboptimal vitamin B6 status, and serum pyridoxal 5’-phosphate level <4,94 µg/L (<20 nmol/L) was estimated as vitamin B6 deficiency. Reference Stover and Field26
Optimal folate status was evaluated as serum folate >4.5 µg/L. Suboptimal folate status was confirmed at the folate serum concentration 3–4.5 µg/L. The concentration suggested for defining folate deficiency based on metabolic indicator was <3 µg/L for serum folate. Reference Devalia, Hamilton and Molloy27
The determination of optimal vitamin B12 status was based on its serum level >300 ng/L. Suboptimal vitamin B12 status was defined as serum cobalamin level 200–300 ng/L. Reference Öner, Guven, Tavli, Mese, Yilmazer and Demirpence28 Vitamin B12 deficiency was estimated as serum cobalamin concentration was <200 ng/L. Reference Devalia, Hamilton and Molloy27
Hyperhomocysteinaemia was defined as serum homocysteine above the 95th percentile for the respective age of healthy children and adolescents. Reference Huemer, Vonblon and Födinger29
All statistics were analysed using the SPSS 12.0 package programme. The study data were expressed using descriptive statistics (mean ± standard deviation, number, percentage). The vasovagal syncope and control groups were compared using the chi-square test for categorical variables and the Mann–Whitney U test for continuous variables. Relationships between variables were examined using Spearman linear correlation analysis. For all analyses, a p value <0.05 was considered statistically significant.
Results
Serum pyridoxine and cobalamin levels were significantly lower in the vasovagal syncope group than in the control group (Table 1). By contrast, there were no significant difference between the two groups regarding folate. However, a high serum homocysteine level was found in children with vasovagal syncope compared with healthy children.
The number of patients with suboptimal status of vitamins B6 and vitamin B12 was significantly higher among children with vasovagal syncope (Table 4). There was no significant difference between healthy and vasovagal syncope patients regarding vitamin B6, folate, and vitamin B12 deficiency. The prevalence of hyperhomocysteinaemia was significantly higher in the vasovagal syncope group than in the control group.
Table 4. Vitamin B6, folic acid, B12, and homocysteine status in examined patients.
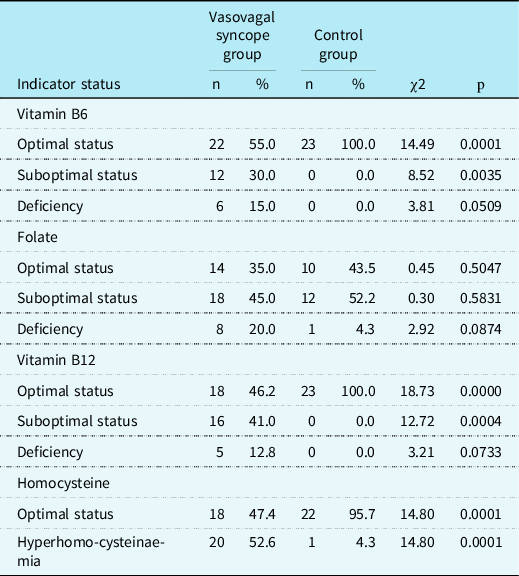
Values are presented as numbers and percentages. Chi-square test was used.
Serum pyridoxine levels were positively correlated with the sex and average QTc interval during 24-hours Holter monitoring in the group of vasovagal syncope (Table 5). Serum folate levels were negatively correlated with the duration of the last syncope and the duration of the last post syncope symptoms. By contrast, serum cobalamin concentrations were negatively correlated with the duration of the last post syncope symptoms. We additionally investigated correlations between serum homocysteine levels and average PQ interval and average QTc interval during 24-hours Holter monitoring. There was no relationship between serum levels of vitamin B6, folic acid, vitamin B12, and homocysteine and indices of heart rate variability (SDANN, root of the 24-hours square, the proportion of adjacent normal R-R intervals <50 ms, total power, very-low-frequency, low frequency, high frequency, low-frequency/high-frequency ratio).
Table 5. Correlation matrix of main clinical parameters of vasovagal syncope and serum levels of vitamin B6, folic acid, vitamin B12, and homocysteine (n = 40).
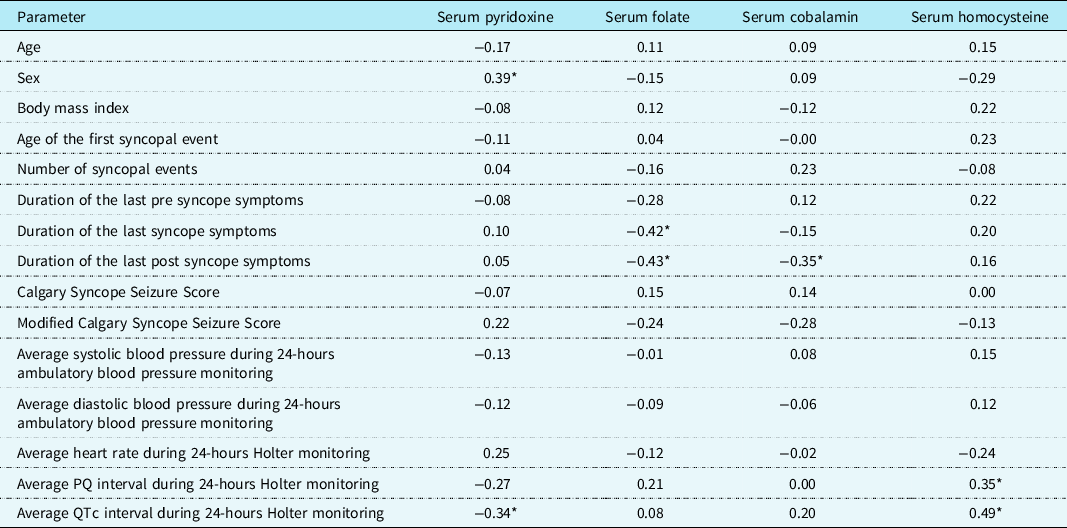
Values are the Spearman’s correlation coefficient.
*Statistically significant correlations (p < 0.05).
Discussion
B vitamins play special and essential roles both in the central nervous system and the peripheral nervous system. It is well known that the diet and thus the supply of nutrients strongly affect normal functioning of central nervous system and the peripheral nervous system. In particular, vitamin B6, B9, and B12 are essential for maintaining the health of the nervous system. Reference Calderón-Ospina and Nava-Mesa8,Reference Black10 Interaction between pyridoxine and cobalamin in the methionine cycle, as well as their participation in the citric acid cycle with other B vitamins, suggests that these vitamins are linked from a biochemical point of view. Reference Moretti and Caruso9,Reference Huemer, Vonblon and Födinger29 Evidence suggests that a significant proportion of the population suffers from deficiencies and insufficiencies of one or more of these neurotropic B vitamins. Reference Stover and Field26–Reference Huemer, Vonblon and Födinger29
The implementation of mandatory folic acid fortification in the United States has been shown to be effective in increasing the biomarker status of folate and, more importantly, has resulted in a substantial reduction in the prevalence of neural tube defects and stroke-related mortality via the homocysteine-lowering effect of folic acid. Reference Choi, Yates, Veysey, Heo and Lucock30 In one meta-analysis of 13 randomised controlled trials of generally good quality, among over 65,000 people living in countries without mandatory folic acid fortification in food, was found that addition of folic acid was associated with a 15% relative risk reduction in future stroke risk. Folic acid alone or combination of folic acid and minimal cyanocobalamin (≤0.05 mg/day) was associated with a 25% lower risks of future stroke. Reference Hsu, Chiu and Hong31
Folate and the metabolically related B vitamins are an important priority throughout life, but few studies have examined their status through childhood and adolescence. In one of them was observed progressive decreases in the status of pyridoxine, folate, cobalamin, with corresponding increases in homocysteine concentrations in British children aged 4–18 years. Although higher homocysteine concentrations were generally associated with lower vitamin B status, the boys were found to have higher homocysteine concentrations compared with girls from age 15 years, despite having a higher biomarker status of the relevant B vitamins. Reference Kerr, Livingstone and Bates7
Vasovagal syncope is the most common cause of syncope across all age groups. Nonetheless, despite its clinical importance and considerable research effort over many years, the pathophysiology of vasovagal syncope remains incompletely understood. Dysfunction of the sympathetic nervous system has been considered to be the main factorr in vasovagal syncope. Reference Lambert and Lambert19 Numerous studies have been undertaken in an attempt to improve insight into the evolution of syncope episodes, and many of these studies have examined neurohormonal changes that occur during the vasovagal syncope events. Reference Jardine, Wieling, Brignole, Lenders, Sutton and Stewart32,Reference Benditt, van Dijk, Krishnappa, Adkisson and Sakaguchi33 Therefore, investigating the pathogenesis of vasovagal syncope and finding effective treatments are necessary.
The present study indicates that serum pyridoxine and cobalamin levels are significantly lower in children with vasovagal syncope while in comparing with healthy ones. There was also statistically higher prevalence of suboptimal status of vitamin B6 and vitamin B12 in children with vasovagal syncope. Despite this, vitamin B6 and vitamin B12 deficiency was not significantly more common in patients with vasovagal syncope than in healthy children.
Our findings are partially comparable with other studies. In one of them, vitamin B12 level was significantly lower in the patients with vasovagal syncope, and authors postulated that vitamin B12 deficiency in patients with postural tachycardia syndrome may lead to sympathetic nervous system baroreceptor dysfunction. Reference Öner, Guven, Tavli, Mese, Yilmazer and Demirpence28 In the other one study, serum vitamin B12 was significantly lower, and prevalence of vitamin B12 deficiency was significantly higher in postural tachycardia syndrome group than in the vasodepressor group. Reference Pektas, Koken and Koca34 Vitamin B12 acts as a co-factor for three enzymes: (1) phentolamine N-methyltransferase which is needed for the conversion of noradrenaline to adrenaline, (2) catecholamine-O-methyltransferase which is required for the degradation of catecholamines, (3) methylmalonyl coenzyme A mutase which catalyses the conversion of methylmalonyl coenzyme A to succinyl coenzyme A in myelin synthesis. Reference Finkelstein, Layden and Stover35 Vitamin B12 deficiency causes reduction in myelinisation, deceleration in nerve conduction, and elevation in serum concentrations of noradrenaline. These factors may contribute to the impairment of autonomic functions which are involved in the pathogenesis of vasovagal syncope. Reference Pektas, Koken and Koca34 Parekh et al. evaluated 35 patients presenting with vasovagal syncope and vitamin B12 deficiency. Supplementation of Vitamin B12 in these patients resulted in significant improvement in symptoms at 1 and 6 months of follow-up. Authors suggested that vitamin B12 deficiency may be linked to vasovagal syncope, and all patients with suspected vasovagal syncope should have their Vitamin B12 levels tested and supplementation given if found to be deficient. Reference Parekh, Sastry, Narasimhan and Arora22
We also have found a negative relationship between serum pyridoxine level and average QTc interval during 24-hours Holter monitoring (r = −0.34, p < 0.05). Kim et al showed that prolonged QTc interval may be considered to be a biomarker for detecting alterations in sympathovagal balance, especially cardiovagal dysfunction in orthostatic hypotension. Reference Kim, Hong, Park, Cho, Park and Kim36 Diedrich et al. used the trimethaphan infusion for interrupting neurotransmission at the level of autonomic ganglia to determine its effect on the QT interval. Autonomic blockade prolongs QT interval in normal subjects to a similar duration as in pure autonomic failure patients. Furthermore, blocking residual autonomic tone in pure autonomic failure patients is associated with a further increase in QT interval length. Reference Diedrich, Jordan, Shannon, Robertson and Biaggioni37 Regarding the vitamin B12, its serum level was correlated negatively with the duration of the last post syncope symptoms (r = −0.35, p < 0.05). The results suggesting that pyridoxine and cobalamin may be involved in the pathogenesis of vasovagal syncope.
This is the first study evaluating serum vitamin B6 level in children presenting with vasovagal syncope. It is well known that vitamin B6 has been associated with over 140 coenzymatic functions. Although its role goes far beyond, it is particularly well known for its important function in the synthesis of neurotransmitters like dopamine from L-3,4-dihydroxyphenylalanine, serotonin from 5-hydroxytryptophan, and gamma-aminobutyric acid from glutamate. Reference Parra, Stahl and Hellmann38,Reference Spinneker, Sola, Lemmen, Castillo, Pietrzik and Gonzalez-Gross39 According to its function for the previously mentioned neurotransmitters, pyridoxine affects the adrenergic, the serotonergic, and the glutamatergic system. Some authors hypotheses that enhanced serotonin responsiveness with clomipramine leading to a presumed greater sympatholytic effect supports a mechanistic role for serotonin in the central pathways leading to vasovagal syncope initiation. Reference Allen, Neergheen and Oppenheim40 Pyridoxine can also be attributed to a neuroprotective role that appears to be mainly linked with its ability to regulate the glutamatergic system and thus gamma-aminobutyric acid and glutamate levels. Since gamma-aminobutyric acid serves as the major inhibitory neurotransmitter, it seems obvious that gamma-aminobutyric acid deficiency can lead to serious consequences, such as syncope and seizures. Reference Calderón-Ospina and Nava-Mesa8,Reference Spinneker, Sola, Lemmen, Castillo, Pietrzik and Gonzalez-Gross39
It should be emphasised that there was no significant difference in folate level and its deficiency between children with vasovagal syncope and healthy individuals in our study. However, decreased levels of folic acid were closely associated with longer duration of syncope (r = −0.42, p < 0.05) and post syncope symptoms (r = −0.43, p < 0.05). There are a limited data regarding serum folic acid level in patients with vasovagal syncope. Oner et al. examined 125 children with neutrally mediated syncope, and 50 healthy children did not find any difference in serum folate level between them. Reference Öner, Guven, Tavli, Mese, Yilmazer and Demirpence28 It is now generally recognised that folate deficiency is rare in the Western world due to folate fortification of wheat flour. Reference Choi, Yates, Veysey, Heo and Lucock30 There is no folic acid fortification programme in Ukraine. This may be the cause of the prevalence of folate suboptimal status and deficiency in 52.2% and 4.3% of healthy children in our study.
In this study, the serum homocysteine level in children with vasovagal syncope was found to be significantly higher than that of the control group. Serum homocysteine level was positively correlated with the average PQ interval (r = 0.35, p < 0.05) and average QTc interval (r = 0.49, p < 0.05) during 24-hours Holter monitoring. Nevertheless, we did not find any relationship between serum levels of vitamin B6, folic acid, vitamin B12, and homocysteine and indices of heart rate variability (SDANN, root of the 24-hours square, the proportion of adjacent normal R-R intervals <50 ms, total power, very-low-frequency, low frequency, high frequency, and low frequency/high frequency ratio). Changes in PR interval, QTc interval, and heart rate variability in younger population can be attributed to incomplete autonomic nervous system maturation. Reference Jug, Bradić, Levicki and Benčić41–Reference Li, He and Li43 The physiology of the autonomic nervous system maturation has not been entirely elucidated yet and potentially relates to both mechanical and neural alterations with ageing. Syncope results from the increased vagal tone, which can also reflect in atrioventricular node activation. The shortening of the PR interval duration is the result of sympathetic activation, despite prolongation of the PR interval duration is the result of parasympathetic activation. Only several papers associate these alterations with the etiopathogenesis of syncope. Reference Jug, Bradić, Levicki and Benčić41
To the best of our knowledge, this is the first study to have evaluated the relationship between the serum homocysteine level and children with vasovagal syncope. Li et al. reported that plasma homocysteine levels were significantly higher in children with postural tachycardia syndrome and that the levels were closely associated with the severity of postural tachycardia syndrome, we inferred that homocysteine might be involved in the mechanism of postural tachycardia syndrome by increasing baroreflex sensitivity. Reference Azzini, Ruggeri and Polito44 Our findings suggest that the change in dietary habits and pyridoxine, folate, cobalamin supplementation may be a therapeutic target in lowering homocysteine level in children with vasovagal syncope. The future studies are required. Equally important is the study of how such recommendations will affect the general well-being of children and be effective in preventing recurrent episodes of vasovagal syncope.
The metabolism of homocysteine is influenced by B vitamins, and homocysteine-lowering vitamin treatments have been proposed. However, clinical trials have not reached a consensus about the effectiveness of vitamin supplementation on the reduction of homocysteine levels and improvement of pathological condition, suggesting that other dietary and non-dietary factors are involved in high homocysteine levels.45 The importance of novel experimental designs focusing on intraindividual variability as a complement to the typical case control experimental designs and the study of interactions between different factors should be emphasised.
However, there were some limitations to this study, the most important of which were the small size of the sample. Further investigation is needed to confirm the significance of these findings. We did not investigate a possible genetic basis for the differences in the serum homocysteine and vitamin B levels such as gene polymorphisms associated with methylenetetrahydrofolate reductase and other homocysteine metabolism. In further studies, whether vitamins B6, B9, B12 supplementation will help improve vasovagal syncope symptoms can be investigated.
In conclusion, serum pyridoxine and cobalamin levels were reasonably low in patients with vasovagal syncope. Although there was no significant change in folate levels between syncope and healthy children, we detected low folate level association with longer duration of syncope and post syncope symptoms. Finally, there was increased serum homocysteine level in patients with vasovagal syncope. The results suggested that pyridoxine, folate, cobalamin, and homocysteine may be involved in the pathogenesis of vasovagal syncope. This might provide a new approach for effective treatment of paediatric vasovagal syncope, requiring further study.
Acknowledgements
The authors would like to thank the children and parents who took part in the study.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees of Ivan Horbachevsky Ternopil National Medical University.








