Introduction
Cognitive behavioural theory and research have played a prominent role in the development of disorder-specific models and treatments for eating disorders (Fairburn et al., Reference Fairburn, Cooper and Shafran2003). Most international clinical guidelines for eating disorders recommend cognitive behavioural therapy as the first-choice treatment for the majority of individuals with an eating disorder (Hilbert et al., Reference Hilbert, Hoek and Schmidt2017). Although cognitive behavioural interventions are considered to be relatively effective in treating eating disorders, there are still many individuals who do not fully recover (Keel and Brown, Reference Keel and Brown2010; Linardon et al., Reference Linardon, Wade, de la Piedad Garcia and Brennan2017; Tatham, Reference Tatham2011). New treatment approaches should therefore be considered in order to enhance treatment outcomes. Cognitive behavioural interventions for eating disorders focus mainly on verbal cognitions and behaviourally based experiments when addressing dysfunctional cognitions and behaviour, while less attention is paid to cognitions in the form of mental imagery (Cooper, Reference Cooper and Stopa2009). Mental imagery is the phenomenon of accessing perceptual information from memory (Kosslyn et al., Reference Kosslyn, Ganis and Thompson2001). These mental representations and the associated sensory modalities are activated without a direct external stimulus (Pearson et al., Reference Pearson, Naselaris, Holmes and Kosslyn2015). Mental images can involve multiple sensory modalities – for example, visual, auditory, gustatory (taste), olfactory (smell), cutaneous (touch), organic (internal body) and kinesthetic (movement; White et al., Reference White, Ashton and Brown1977) and can be described in terms as ‘seeing with the mind’s eye’, ‘hearing with the mind’s ear’, and so forth (Kosslyn et al., Reference Kosslyn, Ganis and Thompson2001). Mental images feel more real than verbal thoughts, and have an important impact on emotions (Holmes and Mathews, Reference Holmes and Mathews2010; Mathews et al., Reference Mathews, Ridgeway and Holmes2013). Due to its effect on emotions, as well as subsequent behaviour, mental imagery may play a critical role in the maintenance of psychopathology (Brewin et al., Reference Brewin, Gregory, Lipton and Burgess2010; Holmes and Mathews, Reference Holmes and Mathews2010).
Instances where mental images are experienced involuntarily are referred to as either intrusive or spontaneous mental images. Well-known examples of these mental images are flashbacks in which traumatic events are re-experienced: a key feature of post-traumatic stress disorder (PTSD; American Psychiatric Association, 2013). These flashbacks evoke great emotional distress. Several studies have shown that spontaneous mental imagery is also common in other mental disorders (Hackmann and Holmes, Reference Hackmann and Holmes2004), such as agoraphobia (Day et al., Reference Day, Holmes and Hackmann2004), social phobia (Hackmann et al., Reference Hackmann, Clark and McManus2000), hypochondria (Muse et al., Reference Muse, McManus, Hackmann, Williams and Williams2010), obsessive compulsive disorder (Speckens et al., Reference Speckens, Hackmann, Ehlers and Cuthbert2007), body dysmorphic disorder (Osman et al., Reference Osman, Cooper, Hackmann and Veale2004) and eating disorders (Hinrichsen et al., Reference Hinrichsen, Morrison, Waller and Schmidt2007; Kadriu et al., Reference Kadriu, Claes, Witteman, Norré, Vrieze and Krans2019; Somerville et al., Reference Somerville, Cooper and Hackmann2007). These images are often related to negative early memories in content and meaning, which may be a transdiagnostic phenomenon (Hackmann and Holmes, Reference Hackmann and Holmes2004; Kadriu et al., Reference Kadriu, Claes, Witteman, Norré, Vrieze and Krans2019). However, several studies have shown that the content and nature of these images may also be disorder specific. Individuals with eating disorders or eating disordered behaviour reported experiencing distressing mental images (e.g. related to appearance) when worrying about their eating, weight or shape (Kadriu et al., Reference Kadriu, Claes, Witteman, Norré, Vrieze and Krans2019; Somerville et al., Reference Somerville, Cooper and Hackmann2007), prior to self-induced vomiting (Hinrichsen et al., Reference Hinrichsen, Morrison, Waller and Schmidt2007), or prior to a binge or an episode of eating too much (Dugué et al., Reference Dugué, Keller, Tuschen-Caffier and Jacob2016).
Some of these studies compared spontaneous mental imagery between individuals with an eating disorder (or eating disordered behaviour) and healthy controls (Dugué et al., Reference Dugué, Keller, Tuschen-Caffier and Jacob2016; Kadriu et al., Reference Kadriu, Claes, Witteman, Norré, Vrieze and Krans2019; Somerville et al., Reference Somerville, Cooper and Hackmann2007). Overall, findings of studies comparing the occurrence of spontaneous mental imagery in individuals with eating disorders and healthy controls suggested that the occurrence of spontaneous mental images may be a normal phenomenon and that the occurrence itself does not have to be pathological. However, the characteristics of these spontaneous mental images appear to be problematic. Spontaneous mental images related to eating, weight or shape were more vivid, negative and anxiety provoking, and involved more sensory modalities in individuals with eating disorder than in dieting and non-dieting controls (Kadriu et al., Reference Kadriu, Claes, Witteman, Norré, Vrieze and Krans2019; Somerville et al., Reference Somerville, Cooper and Hackmann2007). Furthermore, spontaneous mental images of food were experienced as more distressing and were associated with a lower sense of control by individuals with binge eating behaviour than by healthy controls (Dugué et al., Reference Dugué, Keller, Tuschen-Caffier and Jacob2016). Finally, a characteristic of spontaneous mental images that has not yet been investigated in eating disorders, but is often mentioned by individuals with PTSD, is that the re-experiencing of traumatic events is often accompanied by a high sense of ‘nowness’ (i.e. the feeling that the events are happening in the ‘here and now’ rather than stemming from the past; Brewin, Reference Brewin2015). As PTSD is highly prevalent in individuals with an eating disorder (current prevalence rates range from 21 to 62%; Brewerton, Reference Brewerton2007), this feature may also be present in the spontaneous mental images of individuals with an eating disorder.
Research in psychopathology has focused more on intrusive images of past events than on future events. Research has shown that the same neural pathways and cognitive processes are activated when imagining the future as when remembering the past (Szpunar et al., Reference Szpunar, Spreng and Schacter2014). While a traumatic event can be ‘re-experienced’, imagined future events can be ‘pre-experienced’ (Schacter et al., Reference Schacter, Addis and Buckner2007). When involuntary, distressing mental images of events in the future come to mind unbidden, this is defined as intrusive prospective imagery (Deeprose and Holmes, Reference Deeprose and Holmes2010). It was been found that the emotional impact of intrusive prospective imagery is higher in individuals with bipolar disorder (Di Simplicio et al., Reference Di Simplicio, Renner, Blackwell, Mitchell, Stratford, Watson, Myers, Nobre, Lau-Zhu and Holmes2016; Holmes et al., Reference Holmes, Deeprose, Fairburn, Wallace-Hadrill, Bonsall, Geddes and Goodwin2011), schizophrenia (Malcolm et al., Reference Malcolm, Picchioni and Ellett2015), major depressive disorder and anxiety disorders (Morina et al., Reference Morina, Deeprose, Pusowski, Schmid and Holmes2011) in comparison with healthy controls. To our knowledge, the emotional impact of intrusive prospective imagery has never been investigated in eating disorders. As key eating disorder symptoms such as the fear of becoming fat or gaining weight (American Psychiatric Association, 2013) are oriented towards the future and more negative future-oriented cognitions are found in individuals with anorexia nervosa and bulimia nervosa when compared with healthy controls (Godley et al., Reference Godley, Tchanturia, MacLeod and Schmidt2001), it is important to investigate the occurrence and emotional impact of intrusive prospective imagery in eating disorders. Moreover, as prospective imagery may drive future behaviours (Libby et al., Reference Libby, Shaeffer, Eibach and Slemmer2007), this may also explain why individuals engage in eating disorder behaviours like restrictive eating, vomiting or fasting. Furthermore, the emotional impact of these intrusive prospective images has been found to be positively correlated with depression (Deeprose and Holmes, Reference Deeprose and Holmes2010) and risk of bipolar disorder (Deeprose et al., Reference Deeprose, Malik and Holmes2011), suggesting that the emotional impact of intrusive prospective imagery may be positively related to symptom severity.
The aim of the present study was to compare mental imagery between female individuals with an eating disorder and healthy controls. The first research question was whether there would be differences in the occurrence and characteristics of spontaneous mental images related to eating, weight and/or appearance of female individuals with eating disorders compared with those of healthy females. It was expected that there would be no differences in the percentages of participants that reported experiencing spontaneous mental images related to eating, weight and/or appearance. However, we expected that these spontaneous mental images in individuals with an eating disorder would involve more sensory modalities, be more vivid, negative and anxiety provoking, and be experienced with a lower sense of control and a greater sense of ‘nowness’ than those in healthy controls. The second research question was whether the emotional impact of intrusive prospective imagery and the number of negatively reported prospective images would be different in individuals with an eating disorder and healthy controls. We expected that the emotional impact of intrusive prospective imagery and the number of negative prospective images would be higher in individuals with an eating disorder compared with healthy controls. Finally, we explored whether intrusive prospective imagery was related to the severity of eating disorder symptoms, body mass index (BMI) and PTSD symptoms in individuals with an eating disorder. We expected that the emotional impact of the intrusive prospective mental imagery would be associated with more severe eating disorder psychopathology, a lower BMI and more PTSD symptoms.
Method
Participants and procedure
Twenty-nine women with an eating disorder, recruited at the beginning of treatment (in- and out-patients from a specialised eating disorder center), and 32 female healthy controls, recruited from the university, participated in the study. Inclusion criteria for the study for both groups were being female, 18 years or older, and a BMI of 25 or lower. Diagnoses were made by a multi-disciplinary team of experienced clinicians (i.e. psychologists and psychiatrists) specialised in eating disorders, using questions from two standardised semi-structured interviews: the Eating Disorder Examination (Fairburn and Cooper, Reference Fairburn, Cooper, Fairburn and Wilson1993; Jansen, Reference Jansen2000) and the Longitudinal Interval Follow-up Evaluation (Keller et al., Reference Keller, Lavori, Friedman, Nielsen, Endicott, McDonald-Scott and Andreasen1987; Krämer, Reference Krämer1996). Eligible healthy controls were first screened online by means of the Global Health Questionnaire-12 (GHQ-12; Goldberg and Williams, Reference Goldberg and Williams1988; see ‘Measures’ section) to check for current psychiatric symptoms. After that, the procedure for both groups was the same. After signing informed consent, the participants were interviewed individually and were asked to fill out three questionnaires, i.e. the Impact of Future Events Scale (IFES), the Eating Disorder Examination Questionnaire (EDE-Q), and the Self-Rating Inventory for PTSD (SRIP; see ‘Measures’ section). All participants were interviewed by members of the research group (K.H. and S.B.C.). Members of the research group were not blind to the group membership of the participants. The healthy controls received a small number of human research participant credits. The study was approved by the local university Medical Ethics Committee.
Measures
Demographical and clinical variables
Participants’ age (in years), highest educational level (low, medium or high), living situation (living alone/independently, living with partner/children, or living with parents), and eating disorder subtype were recorded.
Semi-structured interview for spontaneous mental imagery
To assess spontaneous mental imagery, a semi-structured interview for mental imagery (Day et al., Reference Day, Holmes and Hackmann2004; Hackmann et al., Reference Hackmann, Clark and McManus2000) was used. A minor adaptation was made to target spontaneous mental imagery in situations relating to eating, weight and/or appearance by asking participants if they had ever experienced mental images when worrying about eating, weight and/or appearance. Participants were given an explanation of what mental images involve, as the concept of an image may be considered as something that should be visual. If they reported that they had not experienced any such image, they were asked if they had a particular impression when they worried about eating, weight and/or appearance. Participants who reported having experienced mental imagery were asked to bring to mind one of these images. Participants rated the sensory modalities [i.e. visual, auditory, gustatory/olfactory, cutaneous and/or organic (inside the body)], vividness, controllability, the level of ‘nowness’ and provoked anxiety, and the level of provoked emotions (i.e. relaxed, happy, sad, scared, angry, humiliated, guilty, ashamed, disgust) of their spontaneous mental images on an 11-point scale ranging from 0 (not at all) to 10 (extremely). Scales that represented positive emotions (i.e. relaxed and happy) were reverse scored and a mean ‘negative emotional tone’ score was calculated.
Intrusive prospective imagery
The IFES (Deeprose et al., Reference Deeprose, Malik and Holmes2011) is based on a measurement for post-traumatic stress symptomatology, the Impact of Event Scale (Horowitz et al., Reference Horowitz, Wilner and Alvarez1979). The IFES is used to assess the impact of intrusive prospective, personally relevant imagery. Participants were asked to identify three events that may happen in the future which they had been thinking about over the previous 7 days. They were also asked whether these future events were positive or negative. Participants were then provided with statements about imagining the future and were asked to indicate how frequently each statement was true for them during the previous 7 days (item examples include ‘I thought about the future when I didn’t mean to’, ‘Pictures about the future popped into my mind’, and ‘Reminders of the future caused me to have physical reactions, such as sweating, faster breathing, or a racing heart’). The IFES Total Score is the sum of 24 items on a 5-point scale ranging from 0 (not at all) to 4 (extremely; range 0–96). The number of negative events per individual is summed to create ‘IFES Negative Events’, which is the total number of events rated by participants as negative (range 0–3). The IFES Total Score has been shown to have good internal consistency (α = .87) and adequate test–re-test reliability (r = .73; Deeprose et al., Reference Deeprose, Malik and Holmes2011).
Eating disorder psychopathology
Eating disorder psychopathology was assessed using the EDE-Q (Fairburn and Beglin, Reference Fairburn, Beglin and Fairburn2008). This is a 28-item self-report questionnaire assessing restraint, shape concerns, weight concerns, eating concerns and frequency of core eating disorder behaviours over the previous 28 days. A global score is calculated by averaging 22 items (range 0–6). The other six items assessed the frequencies of core eating disorder behaviours over the previous 28 days (i.e. frequency of binge eating, over-eating, self-induced vomiting, misuse of laxatives, fasting and excessive exercising). Good discriminative validity has been demonstrated between individuals with and without eating disorder (Aardoom et al., Reference Aardoom, Dingemans, Slof Op’t Landt and van Furth2012).
Body mass index
BMI (weight/height2) was based on self-reported weight (in kg) and height (in metres).
PTSD symptomatology
The SRIP (Hovens et al., Reference Hovens, Bramsen and van der Ploeg2002) is a 22-item Dutch self-report questionnaire assessing PTSD symptoms in the previous 4 weeks on a 5-point scale ranging from 1 (not at all) to 4 (extremely). Scores are summed to create a total score (range 22–88). A score of 52 or above is the threshold for probable PTSD. The SRIP has been shown to have excellent internal consistency (α varying from .90 to .94) and satisfactory test–re-test reliability (r varying from .60 to .97; Hovens et al., Reference Hovens, Bramsen, van der Ploeg and Reuling2000; Hovens et al., Reference Hovens, Bramsen and van der Ploeg2002).
General psychopathology
The GHQ-12 (Goldberg and Williams, Reference Goldberg and Williams1988) was used as a screening tool for general (non-psychotic) psychiatric morbidity in the healthy control group. Participants were asked whether they had recently experienced a particular symptom or behaviour. The 12 items are rated on a 4-point Likert scale and scored according to the GHQ scoring (0–0–1–1). Those who scored below 3 were selected for the study. The psychometric properties of the Dutch version of the questionnaire have been reported to be highly satisfactory (Koeter and Ormel, Reference Koeter and Ormel1991).
Data analysis
Independent samples t-tests or chi-square tests were used to investigate possible differences in socio-demographic and clinical characteristics between the groups. Differences between the groups were investigated using Mann-Whitney U-tests or Fisher’s exact tests in case assumptions for independent samples t-tests or chi-square tests were violated, respectively. Spontaneous mental images and impressions were collapsed into one category. To explore whether the emotional impact of intrusive prospective imagery was related to the severity of eating disorder symptoms, BMI and PTSD symptoms in individuals with an eating disorder, Pearson correlations were calculated. All data were analysed in SPSS Statistics version 22 (IBM Corporation, 2013).
Results
Demographic and clinical characteristics
The eating disorder group had a significantly higher age, a lower BMI, more PTSD symptoms (a higher SRIP total score), and more severe eating disorder psychopathology (a higher EDE-Q global score) than the healthy control group (see Table 1).
Table 1. Demographic and clinical characteristics of the eating disorder group and healthy control group
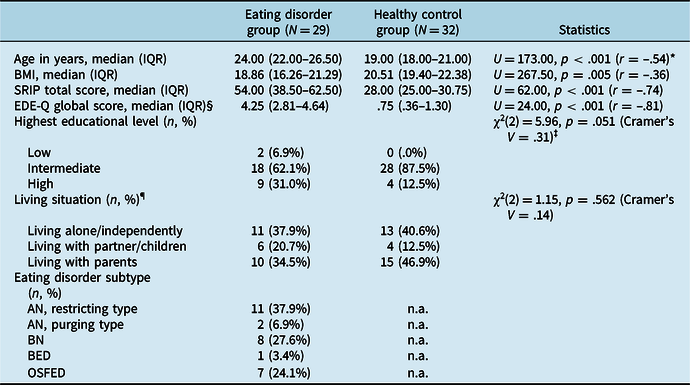
n.a., not applicable; BMI, body mass index; SRIP, Self-Rating Inventory for Posttraumatic Stress Disorder; EDE-Q, Eating Disorder Examination Questionnaire; AN, anorexia nervosa; BN, bulimia nervosa; BED, binge eating disorder; OSFED, other specified feeding or eating disorder. *Effect size r interpretation: .10 small, .30 medium and .50 large. ‡Effect size Cramer’s V interpretation (for d.f. = 2): .07 small, .21 medium and .35 large. §One missing data point in the eating disorder group. ¶Two missing data points in the eating disorder group.
Spontaneous mental imagery related to eating, weight and/or appearance
As expected, there was no significant difference between the two groups in the percentage of individuals experiencing spontaneous mental imagery related to eating, weight and/or appearance (Fisher’s exact test, p = .429, Cramer’s V = .14) Footnote 1 . Twenty-seven individuals with an eating disorder (93.1%) and 27 healthy controls (84.4%) reported experiencing spontaneous mental images. None of the descriptions of the images in the eating disorder or healthy control group met the A criterion of PTSD (actual or threatened death, serious injury or sexual violence; American Psychiatric Association, 2013). Most participants described an image of seeing oneself (e.g. ‘I see myself on a scale and I have gained weight’, ‘I see a fat obese woman’, ‘I see a high number on a scale’ or ‘I see thick thighs’). In the eating disorder group, the visual sensory modality was the most frequently reported modality (n = 27, 100.0%), followed by organic (n = 22, 81.5%), cutaneous (n = 8, 29.6%), auditory (n = 5, 18.5%) and gustatory/olfactory (n = 1, 3.7%; e.g. ‘I feel full’, ‘my belly feels swollen’, ‘I am very aware of my fat body’ or ‘I am not allowed to eat but I can smell and taste the food’). In the healthy control group, the organic sensory modality was the most commonly reported modality (n = 16, 59.3%), followed by the visual (n = 12, 44.4%), auditory (n = 4, 14.8%), gustatory/olfactory (n = 2, 7.4%) and cutaneous (n = 2, 7.4%).
In accordance with our expectations, the spontaneous mental images in the eating disorder group involved significantly more types of sensory modalities, were more vivid, more negative, and more anxiety provoking, and were experienced with a lower sense of control than those in the healthy control group. No significant differences were found between the eating disorder group and the healthy control group in terms of ‘nowness’ (see Table 2).
Table 2. Mean (SD) and medians (IQR) for the characteristics of spontaneous mental images/impressions in the eating disorder group and healthy control group

*Effect size r interpretation: .10 small, .30 medium and .50 large. ‡Effect size Cohen’s d interpretation: .20 small, .50 medium, .70 large.
Intrusive prospective imagery
As expected, the eating disorder group reported a greater emotional impact of intrusive prospective imagery (IFES Total Score; median = 46.00, IQR = 30.00–61.00) Footnote 2 than the healthy control group (median = 18.00, IQR = 13.25–26.75), U = 105.00, p < .001 (r = –.66) Footnote 3 . Also, the eating disorder group reported a higher number of negative events (IFES Negative Events; median = 2.00, IQR = 1.00–2.00) Footnote 4 than the healthy control group (median = 1.00, IQR = 1.00–1.75), U = 283.00, p = .016 (r = –.31).
A greater emotional impact of intrusive prospective imagery (as measured by the IFES Total Score) was associated with more severe PTSD symptoms (SRIP total score; r = .88, p < .001) and with more severe eating disorder psychopathology (EDE-Q global score; r = .70, p < .001). However, the emotional impact of intrusive prospective imagery (IFES Total Score) was not significantly related to BMI (r = –.02, p = .928).
Discussion
The general aim of the present study was to compare spontaneous mental imagery related to eating, weight and/or appearance and intrusive prospective imagery in women with an eating disorder with female healthy controls. As expected, both groups of women experienced spontaneous mental images when they worried about their eating, weight and/or appearance. However, the characteristics of these images (e.g. number of sensory modalities, vividness, emotional tone, degree to which they provoked anxiety and controllability) differed between the two groups. For example, we found that that spontaneous mental images related to eating, weight and/or appearance were more vivid, negative and anxiety provoking, and involved more sensory modalities in women with eating disorders compared with those in healthy controls. These findings are in line with studies by Kadriu et al. (Reference Kadriu, Claes, Witteman, Norré, Vrieze and Krans2019) and Somerville et al. (Reference Somerville, Cooper and Hackmann2007). Furthermore, individuals with an eating disorder experienced their spontaneous mental images with a lower sense of control than healthy controls, which is consistent with the findings of Dugué et al. (Reference Dugué, Keller, Tuschen-Caffier and Jacob2016), who compared individuals with a binge eating behaviour with healthy controls.
Contrary to our hypothesis, the spontaneous mental images in female individuals with an eating disorder were not experienced with a higher sense of ‘nowness’ compared with healthy controls. In other words, the feeling that the events within these images were happening in the ‘here and now’ rather than stemming from the past was not different between the groups. Moreover, levels of ‘nowness’ in both groups were low. A possible explanation for these findings is that a controlled research setting may have resulted in feeling more control over the images, and may therefore have resulted in low levels of ‘nowness’.
The second research question was whether individuals with an eating disorder differed from healthy controls with respect to the emotional impact of intrusive prospective imagery and the number of negative intrusive prospective mental images. As expected, a greater emotional impact of intrusive prospective imagery was found in individuals with an eating disorder than in healthy controls. These findings are in line with the results of studies that found a greater emotional impact of intrusive prospective imagery in individuals with bipolar disorder (Di Simplicio et al., Reference Di Simplicio, Renner, Blackwell, Mitchell, Stratford, Watson, Myers, Nobre, Lau-Zhu and Holmes2016; Holmes et al., Reference Holmes, Deeprose, Fairburn, Wallace-Hadrill, Bonsall, Geddes and Goodwin2011), schizophrenia (Malcolm et al., Reference Malcolm, Picchioni and Ellett2015), major depressive disorder and anxiety disorders (Morina et al., Reference Morina, Deeprose, Pusowski, Schmid and Holmes2011) in comparison with healthy controls. Intrusive prospective images were more negative in individuals with an eating disorder than in healthy controls. Similarly, Godley et al. (Reference Godley, Tchanturia, MacLeod and Schmidt2001) found more negative future-oriented cognitions in individuals with anorexia nervosa and bulimia nervosa when compared with healthy controls. To our knowledge, this is a new finding for individuals with an eating disorder, and a specific focus on imagery related to the future could be incorporated into treatment interventions.
Finally, we explored whether the emotional impact of prospective mental imagery in the eating disorder sample was related to the severity of eating disorder psychopathology, BMI and PTSD symptoms. Indeed, the severity of the eating disorder psychopathology and PTSD symptoms were strongly and positively correlated with the emotional impact of prospective intrusive imagery. Similarly, studies showed that the emotional impact of this intrusive prospective imagery was positively correlated with depression (Deeprose and Holmes, Reference Deeprose and Holmes2010) and risk of bipolar disorder (Deeprose et al., Reference Deeprose, Malik and Holmes2011), suggesting that the emotional impact of intrusive prospective imagery is positively related to symptom severity in women with an eating disorder. With this in mind, clinicians should ask specifically about the existence of prospective mental images as this may explain the severity of the eating disorder symptoms and PTSD symptoms in individuals with an eating disorder, which may hamper improvement. BMI was not found to be related to the emotional impact of intrusive prospective imagery, suggesting that the emotional impact of intrusive prospective imagery may be comparable in different eating disorder subtypes. However, more research is warranted.
With cognitive behavioural therapy, which has a major focus on verbal thoughts and behaviours, being the first-choice treatment in many guidelines, the importance of mental imagery in psychopathology is not always fully recognised or acknowledged (Hackmann and Holmes, Reference Hackmann and Holmes2004; Pearson et al., Reference Pearson, Naselaris, Holmes and Kosslyn2015). These verbal therapies do not seem to address the intrusiveness and the emotional impact of these images, but more research is needed. Compared with verbal representations, mental images are more emotionally arousing and appear more realistic (Holmes and Mathews, Reference Holmes and Mathews2010; Mathews et al., Reference Mathews, Ridgeway and Holmes2013). This underlines the importance of addressing these images via the use of imagery-based techniques [e.g. imagery rescripting and eye movement desensitisation and reprocessing (EMDR); Foa et al., Reference Foa, Rothbaum, Riggs and Murdock1991; Morina et al., Reference Morina, Lancee and Arntz2017; Shapiro, Reference Shapiro2002], in which the focus should not only be on the visual aspects of the spontaneous mental imagery, but also other sensory modalities of these images, such as the cutaneous and organic sensory modalities. These techniques could be incorporated in the standard cognitive behavioural therapy for eating disorders (Tatham, Reference Tatham2011). Imagery-based interventions have already demonstrated their effectiveness in treating PTSD and are the interventions of preference according to multiple guidelines for individuals with PTSD [National Institute of Health and Care Excellence (NICE), 2005]. Also, in other disorders, such as social phobia and personality disorders, imagery-based interventions appear to be of value (Arntz, Reference Arntz2012). In eating disorders, imagery-based interventions such as imagery rescripting (Cooper et al., Reference Cooper, Todd and Turner2007; NICE, 2005; Pennesi and Wade, Reference Pennesi and Wade2018) or EMDR (Bloomgarden and Calogero, Reference Bloomgarden and Calogero2008) seem to be promising in improving body image acceptance and self-compassion and in reducing levels of disordered eating, levels of distress about negative body image memories, and negative emotional self-belief ratings. The results of our study suggest that the imagery-based interventions should not focus exclusively on the past but also on the future to diminish the distress of prospective imagery.
One of the strengths of the present study is that this is the first study to investigate intrusive prospective imagery in individuals with an eating disorder. However, several limitations in the present study warrant attention and suggest directions for future research. First, due to the cross-sectional design of the current study, no conclusions can be drawn about causality of imagery and eating disorder and whether the presence of mental images may be a maintaining factor of eating disorder psychopathology. Second, individuals were recruited from a highly specialised (tertiary care) centre for eating disorders, which may explain the relatively large proportion of individuals with anorexia nervosa in the sample. It is unknown whether imagery is influenced by low BMI and/or malnutrition. Also, the prevalence of PTSD in individuals with an eating disorder may be higher compared with other care settings with less complex individuals. Third, interviewers were not blinded to the diagnostic status of the participants. Fourth, there was a significant difference between the two groups with respect to their highest educational level and their age. However, it is unknown whether imagery is related to, or influenced by, educational level and/or age. Fifth, height, weight, eating disorder and PTSD symptoms were based on self-reporting, which may have had an effect on their accuracy. Sixth, we had a small sample size, therefore we could not analyse different eating disorder subtypes separately. However, research has shown that individuals with eating disorders tend to migrate between the diagnostic categories of anorexia nervosa, bulimia nervosa and the atypical eating disorders. This temporal movement, together with the fact that anorexia nervosa, bulimia nervosa and the atypical eating disorders (including binge eating disorder) share the same eating disorder psychopathology, like overvaluation of shape and weight, suggests that common mechanisms are involved in the persistence eating disorder psychopathology (Fairburn et al., Reference Fairburn, Cooper and Shafran2003). Seventh, the total sample consisted only of women. Therefore, results cannot be generalised to men. Eighth, all participants were interviewed by members of the research group (K.H. and S.B.C.), who were not blind to the group membership of the participants. Additional research, particularly studies employing a longitudinal design, are needed to investigate the role of imagery in treatment, recovery and relapse. Future studies with a larger sample size are needed to explore which factors may explain the characteristics of imagery.
In conclusion, the current study suggested that both female individuals with an eating disorder and female healthy controls experienced spontaneous mental images when they worry about their eating, weight and/or appearance. However, the images of individuals with an eating disorder involve more sensory modalities, were more vivid, negative and anxiety provoking, and were experienced with a lower sense of control than those of healthy control women. Furthermore, individuals with an eating disorder reported more negative images with regard to personally relevant future events and a greater emotional impact of prospective intrusive imagery compared with healthy controls. Moreover, the emotional impact of prospective mental imagery was strongly related to eating disorder severity and PTSD symptoms. Our results suggest that maladaptive mental imagery in female individuals with an eating disorder may play a role in the development and/or maintenance of eating disorders and should be acknowledged and addressed in treatment. Future longitudinal studies and randomised controlled trials assessing the effectiveness of treatments targeting these images could help to elucidate the relationship between mental images and eating disorder psychopathology.
Acknowledgements
The authors would like to thank the participants in the study.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
Kim Hijne, Suzan Ben Chamach and Alexandra Dingemans have no conflicts of interest with respect to this publication.
Ethical statements
The study was approved by the Leiden University Medical Center Medical Ethics Committee in the Netherlands (number NL55254.058.15). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.





Comments
No Comments have been published for this article.