Marfan syndrome is a systemic connective tissue disorder that affects approximately 1 in 5000 individuals Reference Chiu, Wu and Chen1 and impacts multiple organ systems. The primary cause of death in these patients is a result of aortic disease. Reference Judge and Dietz2,Reference Groth, Stochholm and Hove3 The dilatation of the aortic root tends to be progressive in this disease and requires close observation by a cardiologist. Reference Radke and Baumgartner4,Reference Milleron, Arnoult and Delorme5 To avoid significant morbidity and mortality in these patients, medical therapy is often used to slow the progression of aortic root enlargement and delay the need for surgical intervention, though this remains an area of some controversy. Reference Gao, Chen and Gao6
There have been many studies on the effectiveness of medical therapy in patients with Marfan syndrome. In 2014, the Pediatric Heart Network randomised trial of losartan versus atenolol in Marfan syndrome patients showed no treatment differences in the rates of aortic root growth or clinical outcomes between the two treatment arms. Reference Lacro, Dietz and Sleeper7,Reference Lacro, Dietz and Sleeper8 Similarly, the losartan versus atenolol trial compared the efficacy of the two medications and found no difference. Reference Teixido-Tura, Forteza and Rodriguez- Palomares9 Malik et al found that while losartan and atenolol both significantly reduced aortic root growth, there was not a significant difference between the two, but the most significant reduction in the aortic root growth was with the use of a combination of beta blocker and angiotensin II receptor blocker. Reference Malik, Yandrapalli and Pemmasani10 Recent studies by Mullen et al. and Tierney et al found conflicting results for beta blockers versus angiotensin receptor blockers. Reference Mullen, Jin and Child11,Reference Tierney, Levine and Sleeper12
Recent data suggest that angiotensin receptor blockers and angiotensin-converting enzyme inhibitors may have different pharmacologic effects in different racial/ethnic populations. Specifically, studies have demonstrated decreased efficacy for the treatment of hypertension in African-American patients as compared to White patients. Reference Helmer, Slater and Smithgall13 Helmer et al reviewed the literature from 2000 to 2018 and concluded that angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers should not routinely be initiated as monotherapy in Black hypertensive patients. Reference Helmer, Slater and Smithgall13 In the Pediatric Heart Network study, 87% of the 608 patients were of non-Hispanic White origin, but differences in response to treatment with losartan (angiotensin II receptor blocker) versus atenolol (beta blocker) were not reported on the basis of race/ethnicity. Given the data suggesting differing blood pressure responses to these classes of medications based on race, the objective of our study was to determine whether racial/ethnic differences exist with regards to the pharmacologic effects of medical therapy for aortopathy in Marfan syndrome with losartan versus atenolol. We hypothesised that non-Hispanic Black patients taking atenolol would have greater benefit in their aortic root diameter indexed to body surface area (hereafter, aortic root z score) than non-Hispanic Black patients taking losartan.
Materials and methods
We performed a secondary analysis of public-use data released in 2018 from the Pediatric Heart Network randomised trial comparing losartan versus atenolol in children and young adults with Marfan syndrome. Reference Lacro, Dietz and Sleeper7,Reference Lacro, Dietz and Wruck14 Of note, there were not patient or population involvement in our study, as this was a secondary analysis of a public-use dataset. The original study included patients at 21 centres from January, 2007 to February, 2011 with a diagnosis of Marfan syndrome (defined by the Ghent criteria Reference De Paepe, Devereux and Deitz15 ). Patients were aged 6 months–25 years and had a maximum aortic root z score greater than 3.0 at study enrolment. The study excluded patients with aortic root diameter greater than 5.0 cm; history of aortic dissection; past or upcoming aortic root surgery; therapeutic rather than prophylactic use of an angiotensin-converting enzyme inhibitor, beta blocker, or calcium channel blocker; diagnosis of Loeys–Dietz or Shprintzen–Goldberg syndromes; prior adverse effects from or contraindication to treatment with an angiotensin II receptor blocker or beta blocker; inability to complete the study procedures. Reference Lacro, Dietz and Wruck14 Patients were randomised to losartan or atenolol treatment groups stratified by age and baseline aortic root z score of greater or less than 4.5. The patients were followed for 3 years and echocardiographic aortic parameters were measured at baseline and 6, 12, 24, and 36 months after randomisation by core echocardiography laboratory members who were unaware of treatment assignment and study visit number. Reference Lacro, Dietz and Wruck14
Atenolol dosing was started at 0.5 milligram per kilogram (mg/kg) and was increased based on haemodynamic response to a maximum of 4.0 mg/kg per day (up to 250 mg) with a goal of 20% or greater reduction in heart rate. Reference Lacro, Dietz and Sleeper7 The mean dose of atenolol was 2.7 ± 1.1 mg per kilogram per day; the mean absolute dose for young adults was 151 ± 75 mg of atenolol per day. Losartan dosing was started at 0.4 mg/kg and was increased to a goal dose of 1.4 mg/kg per day (maximum 100 mg), as recommended by the United States of America Food and Drug Administration for the treatment of hypertension. Reference Lacro, Dietz and Sleeper7 The mean dose of losartan was 1.3 ± 0.2 mg per kilogram per day; the mean absolute dose for young adults was 85 ± 14 mg of losartan per day.
In our analysis, we categorised the patients in the study population into groups by race/ethnicity into non-Hispanic Black, non-Hispanic White, or Hispanic. Due to limited numbers for patients classified as other or Asian, those data were not included. For our primary outcome, we compared the annual change in the aortic root enlargement by z score between treatment groups within each race/ethnicity strata over the 3-year study period after randomisation. Similarly, the secondary outcome of rate of change of the absolute diameter of the aortic root as well as the absolute diameter and z score of the ascending aorta were also compared between treatment groups for each race strata. We performed treatment group comparisons using Student’s t-test or Wilcoxon rank-sum test for continuous characteristics and chi-square tests for categorical characteristics. We modelled the annual rate of change of echocardiographic aortic parameters using mixed-effects linear regression to account for the longitudinal design, with the use of compound symmetry covariance structure. A similar analysis was performed to compare the rate of change in blood pressure by race/ethnicity. The baseline-adjusted rates of change in the two treatment groups were compared with the use of a test of the treatment-by-time interaction effect.
Results
Baseline characteristics
Of the 572 patients meeting inclusion criteria, 46 were non-Hispanic Black, 80 Hispanic, and 446 non-Hispanic White. There were similar distributions amongst the treatment groups by race/ethnicity and there were no statistically significant differences in baseline demographic or clinical characteristics (Table 1).
Table 1. Demographic and clinical characteristics at baseline (n = 572).

* Young adults were defined as male patients who were 16–25 years of age and female patients who were 15–25 years of age
Change in aortic root z score
We did not find statistically significant differences in change in aortic root enlargement z score for non-Hispanic Black or Hispanic patients, but amongst non-Hispanic White patients, we found a small but statistically significant benefit to treatment with atenolol. non-Hispanic Black patients had an annual z score change of –0.119 ± 0.056 with atenolol, compared to –0.196 ± 0.051 with losartan (p = 0.31), while Hispanics had an annual z score change of –0.128 ± 0.042 with atenolol, compared to –0.179 ± 0.037 with losartan (p = 0.36) (Table 2, Fig. 1). However, for change in aortic root enlargement by z score amongst non-Hispanic White patients, there was a slightly greater decrease in aortic root z score of –0.146 ± 0.015 for those on atenolol versus –0.090 ± 0.016 for those on losartan (p = 0.01) (Table 2, Fig 1).
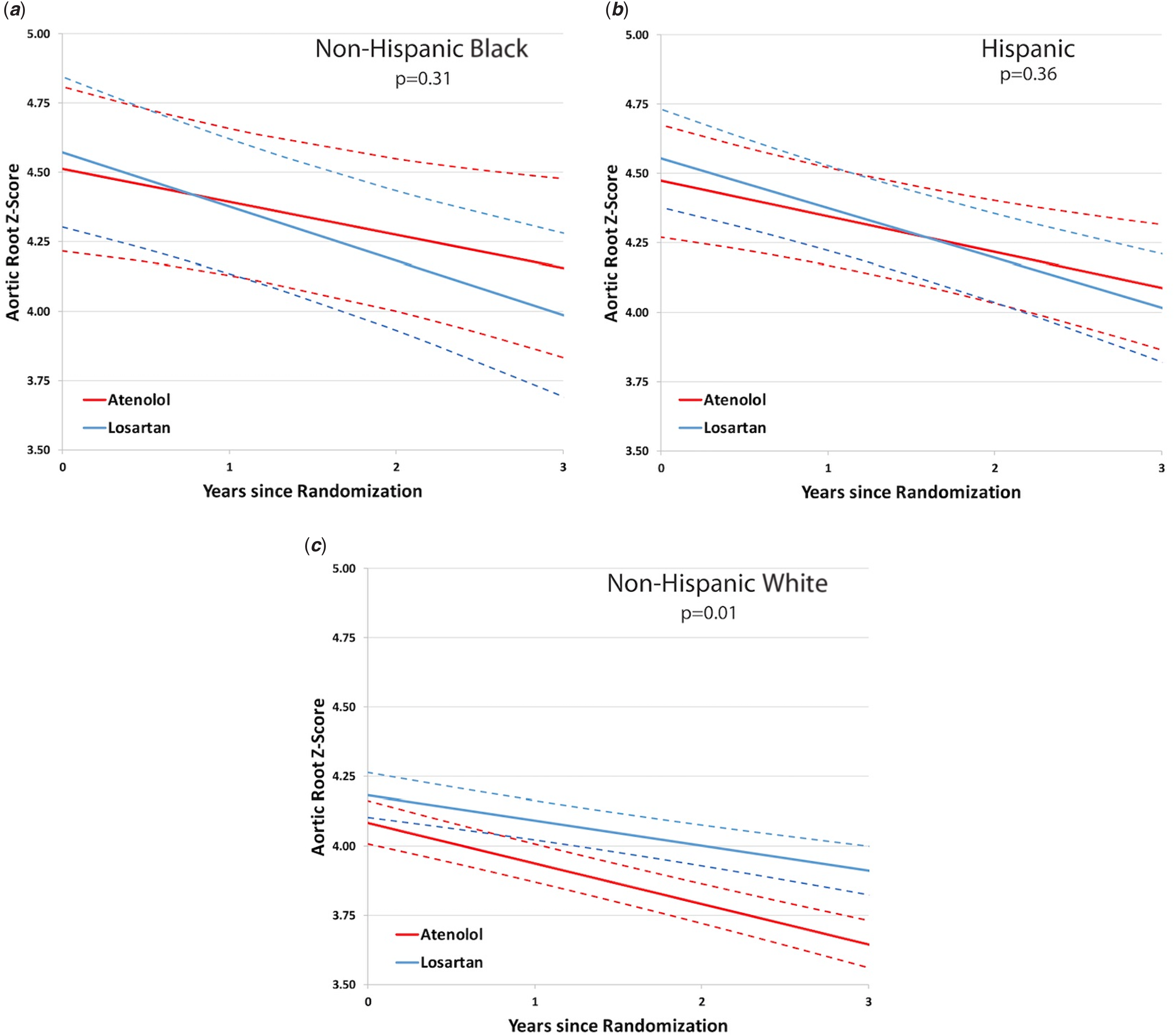
Figure 1. Effects of losartan (red lines) vs atenolol (blue lines) on aortic root z-score in patients with Marfan syndrome stratified by race/ethnicity. There were no significant differences in change in aortic-root enlargement z-score for NH Black (a) or Hispanic patients (b), but among NH White patients (c) there was a small but significant benefit favoring atenolol. Data shown are estimated slopes of z-scores in standard deviation units per +SE and P values are based on a linear regression mixed effects model comparing slopes under compound symmetry, with adjustment for baseline covariates.
Table 2. Annual rate of change of outcomes over 3 years.

* Data shown are estimated slopes of z scores in standard deviation units per ± SE and diameters in centimetres per year ± SE
** p values are based on a linear regression mixed-effects model comparing slopes under compound symmetry with adjustment for baseline covariate
Change in aortic root diameter
For non-Hispanic Black and Hispanic patients, there were no changes in aortic root diameter when stratified by race/ethnicity (Table 2). The change in aortic root diameter for non-Hispanic White patients nearly reached statistical significance favouring atenolol. There was an annual rate of aortic root growth of 0.066 ± 0.004 amongst non-Hispanic White patients taking atenolol compared to 0.077 ± 0.004 for those taking losartan, p = 0.056 (Table 2).
Change in ascending aorta z score
We found no significant differences in change in ascending aorta z score for non-Hispanic Black, Hispanic, or non-Hispanic White patients. Change in ascending aorta z score was –0.142 ± 0.052 for atenolol and –0.130 ± 0.047 for losartan (p = 0.87) for non-Hispanic Black patients; −0.134 ± 0.042 for atenolol and –0.145 ± 0.035 for losartan (p = 0.84) for Hispanic patients; −0.144 ± 0.015 for atenolol and –0.111 ± 0.016 for losartan (p = 0.14) for non-Hispanic White patients (Table 2, Fig. 2).

Figure 2. Effects of losartan (red lines) vs atenolol (blue lines) on ascending aorta z-score in patients with Marfan syndrome stratified by race/ethnicity. There were no significant differences in change in ascending aorta z-score for NH Black (a), Hispanic (b), or NH White (c) patients. Data shown are estimated slopes of z-scores in standard deviation units per +SE and P values are based on a linear regression mixed effects model comparing slopes under compound symmetry, with adjustment for baseline covariates.
Change in ascending aorta diameter
We found no significant differences in change in ascending aorta diameter between non-Hispanic Black, Hispanic, and non-Hispanic White patients when comparing treatment groups (Table 2).
Blood pressure
Importantly, there was no significant difference in the rate of change of blood pressure over the 3 years between treatment groups, when stratified by race/ethnicity. We analysed systolic blood pressure, systolic blood pressure-for-age z score, diastolic blood pressure, diastolic blood pressure-for-age, mean blood pressure, and mean blood pressure-for-age z score and there was no statistically significant difference in the decrease in blood pressure between losartan and atenolol when examined by race/ethnicity (Table 3).
Table 3. Blood pressure differences between treatment groups by race/ethnicity.

* Plus–minus values are means ± SD, except where otherwise noted. The z score was indexed to the body surface area unless otherwise specified. CI denotes confidence interval
** Data shown are estimated slopes of z scores in standard deviation units per ± SE and diameters in centimetres per year ± SE
*** P values are based on a linear regression mixed-effects model comparing slopes under compound symmetry with adjustment for baseline covariate
Discussion
In this study, we found differences by race/ethnicity in response to treatment of losartan compared to atenolol: non-Hispanic White patients indeed showed a reduced response to losartan compared to atenolol. Although non-Hispanic Black and Hispanic patients did not have a statistically significant difference in response to losartan versus atenolol, Figure 1 suggests that there may be a slight benefit with losartan as compared to atenolol in these patients that were not able to be statistically demonstrated due to small sample size. When examining the blood pressure z scores between the two medications, all patient groups had similar blood pressure changes following initiation of medical therapy. This absence of a difference in documented blood pressure response between racial groups might explain why our original hypothesis did not prove to be correct.
Interestingly, another recent ancillary study of the Pediatric Heart Network randomised atenolol versus losartan in Marfan syndrome trial investigated the impacts of genetic variants in response to atenolol or losartan. Reference Franken, den Hartog and van de Ret17 The study objective was to determine if variants in the ADRB1 or CYP2C0 genes affected response to either atenolol or losartan in White, non-Hispanic patients in the Pediatric Heart Network study. They found that one of the variants in the ADRB1 gene, the rs1801253 variant, was associated with response to atenolol. They did not find differences in atenolol response by ADRB1-rs1801252 genotype or in losartan response by CYP2C9 metaboliser status. Reference Van Driest, Sleeper and Gelb16 This study, if confirmed in future studies, could help explain our findings and highlights the need for more studies designed and powered to understand potential racial differences in treatment effects based upon the prevalence of genetic variants affecting drug metabolism that may differ between different groups. Much like the treatment of hypertension or congestive heart failure, there may be specific classes of medication that may be more effective for different patient groups.
Our study is unique in that it examined treatment differences in Marfan syndrome by race/ethnicity. There have been studies that have evaluated racial/ethnic differences in the clinical features of patients with Marfan syndrome. Reference Franken, den Hartog and van de Ret17,Reference Yoo, Woo and Ki18 Franken et al examined clinical features and showed more significant aortic dilatation in those of Asian descent, Reference Franken, den Hartog and van de Ret17 and Yoo et al showed that compared to Western populations, Koreans with Marfan syndrome had a lower frequency of skeletal and ocular manifestations and higher frequency of cardiovascular manifestations. Reference Yoo, Woo and Ki18 However, neither of these studies examined treatment differences.
This study is not without limitations. First, the relatively small sample size of Hispanic and non-Hispanic Black patient groups potentially caused the study to be underpowered. While this trial contains more non-Hispanic Black and Hispanic minorities than other previous studies, there were still only 46 non-Hispanic Black and 80 Hispanic patients. As discussed, Figure 1 and Table 2 show that non-Hispanic black patients receiving losartan had the most improved annual rate of change in aortic root z score, although this did not reach statistical significance. It is possible that some of our findings, especially amongst non-Hispanic Black patients, may have met significance with more patients and hence greater power. The other limitations of our study are similar to the limitations of the original Pediatric Heart Network study. First, in the Pediatric Heart Network study, there was not a placebo group, and there was not a group with combination therapy with both atenolol and losartan as there have been in other studies. Second, the dosing used in the study for losartan was lower than what was used in the studies done utilising mouse models, and some providers do use higher dosing, although the higher dosing is not what is considered standard practice. Third, bias may have been introduced, as it was possible for patients to discover their treatment assignment based on the study drug appearance. Fourth, those with an aortic root z score of 3.0 or less were not included, so our results may not be generalisable to that population. Additionally, the study used aortic dimensions as a surrogate rather than true aortic clinical events, given their rarity.
Given the data on decreased efficacy of angiotensin II receptor blockers for the treatment of hypertension in African Americans, our results showing that treatment with losartan compared to atenolol in non-Hispanic Black patients with Marfan syndrome yielded similar results are surprising and important. Some providers might avoid using angiotensin II receptor blockers in African-American patients due to previously published literature, but this data could help guide management changes. Conversely, in non-Hispanic White patients, our findings suggest that atenolol may be a better choice than losartan. While the other outcomes we examined did not show statistically significant differences in response to treatment based on race/ethnicity, we suspect that this may be due to a lack of power. While it remains to be seen if the findings in our study will be clinically significant, it is a promising finding in the setting of the original Pediatric Heart Network study showing no statistically significant difference between the two treatment groups. These findings may have important implications for future studies on medication selection based on race/ethnicity for those with Marfan syndrome. Additionally, our study highlights the need for future studies directed at investigating treatment differences between racial and ethnic groups with larger sample sizes.
Acknowledgements
We acknowledge those parties involved in the Pediatric Heart Network study database on Marfan syndrome, who made our work possible.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
Not applicable. This is a secondary study of previously published data, and informed consent by the subjects and IRB approval was obtained for the original study.
Research dataset
The National Institutes of Health/National Heart, Lung, Blood Institute Pediatric Heart Network Marfan study dataset was used in the preparation of this work. Data were downloaded from http://pediatricheartnetwork.org/ForResearchers/PHNPublicUseDatasets.aspx on 15 November, 2018. The public-use dataset is available through Pediatric Heart Network upon request.








