Left ventricular hypertrophy in patients with masked hypertension has been shown to be similar to those true hypertensive adults.Reference Liu, Roman, Pini, Schwartz, Pickering and Devereux 1 , Reference Sega, Trocino and Lanzarotti 2 This suggests that patients with masked hypertension are not fundamentally different from their counterparts, but represent a different phenotypic expression of high blood pressure. Left ventricular hypertrophy is easily measurable in children and adolescents. Therefore, it can be a surrogate marker for the hypertensive end-organ damage in children.Reference Lurbe, Torro and Alvarez 3 – Reference Stabouli, Kotsis, Toumanidis, Papamichael, Constantopoulos and Zakopoulos 5
However, little attention has been given to paediatric masked hypertension until recently. The first report on paediatric masked hypertension was published in 2004.Reference Matsuoka and Awazu 6 In previous studies, paediatric masked hypertension was associated with more extensive target organ damage than in true normotensives.Reference Lurbe, Torro and Alvarez 3 – Reference Stabouli, Kotsis, Toumanidis, Papamichael, Constantopoulos and Zakopoulos 5 Higher left ventricular mass in masked hypertension, when compared with normal patients, was reported.Reference Lurbe, Torro and Alvarez 3 – Reference Stabouli, Kotsis, Toumanidis, Papamichael, Constantopoulos and Zakopoulos 5 However, only Lurbe et alReference Lurbe, Torro and Alvarez 3 reported the left ventricular mass index in youth with persistent masked hypertension. The above findings were based on small groups of children with masked hypertension, who were heterogeneous and came from clinical settings. In addition, the information on the persistence of childhood masked hypertension is limited. The importance of demonstrating the reproducibility of masked hypertension has been highlighted in adult studies,Reference Pickering, Davidson, Gerin and Schwartz 7 , Reference Verberk, de Leeuw and Thien 8 both of which considered reproducibility only in the short term, but we identified a study of the reproducibility of paediatric masked hypertension diagnosis over a median follow-up period of 37 months.Reference Lurbe, Torro and Alvarez 3 About 40% of the patients were found to have persistent masked hypertension in this Spanish adolescent study. More research in this area is definitely required.
In our previous study, we found masked hypertension in 165 (11.9%) of 1445 individuals aged 8–17 years from our community-based cross-sectional study according to our local reference.Reference Yip, Li and So 9 The aim of this study then is to assess the left ventricular mass index of persistent masked hypertension in Hong Kong Chinese adolescents from this community cohort.
Materials and methods
The baseline data were collected in a 2011/2012 Hong Kong Chinese children 24-hour ambulatory blood pressure monitoring study.Reference Yip, Li and So 9 All patients with masked hypertension – defined as daytime ambulatory blood pressure ⩾95th percentile according to the local reference – at baseline were invited to recheck ambulatory blood pressure using TM-2430 (A&D Inc., Tokyo, Japan)Reference Yip, So, Li, Tomlinson, Wong and Sung 10 for the persistence of masked hypertension. The patients underwent anthropometric measurements and echocardiography. Blood tests were performed for plasma fasting glucose, lipid profile, and serum insulin. Dietary assessment of all patients was performed using a 3-day food record and a validated physical activity questionnaire.Reference Hui 11 All patients with persistent masked hypertension, defined as masked hypertension on at least two consecutive examinations, last contact included, were matched with normotensive controls for sex, age, and body height. Informed consents were obtained from the participants and their parents before the follow-up.
Blood pressure measurements
Office blood pressure was measured using oscillometric machine three times in each patient after 5 minutes of rest, at least 1 minute apart, using the Datascope Accutorr Plus, which has been validated for use in local Chinese children and adolescents.Reference Wong, Tz Sung and Leung 12
Ambulatory blood pressure was performed using a validated portable non-invasive oscillometric recorder (TM-2430).Reference Yip, So, Li, Tomlinson, Wong and Sung 10 The ambulatory blood pressure monitoring readings were obtained every 30 minutes over a 24-hour period. All readings taken during 24 hour were used to calculate mean 24-hour systolic blood pressure and diastolic blood pressure, mean daytime systolic blood pressure, and mean night-time systolic blood pressure and diastolic blood pressure, in accordance with the method proposed by Soergel et al.Reference Soergel, Kirschstein and Busch 13 Local reference was used for the definition of ambulatory hypertension as mean daytime systolic blood pressure and/or diastolic blood pressure greater than or equal to the 95th percentile for gender and height.Reference Yip, Li and So 9 Patients with both office blood pressure and ambulatory blood pressure within normal range were characterised as confirmed normotensives. Patients with both office and ambulatory blood pressure recordings above normal range were characterised as confirmed hypertensives. Patients with office hypertension and ambulatory normotension were characterised as white-coat hypertensives, and patients with office normotension and ambulatory hypertension were characterised as masked hypertensives.
Echocardiography
An experienced echocardiographer, blinded to the clinical information of the patients, performed the echocardiographic assessment (Vivid E9, GE Healthcare, Chicago, IL, United States of America). Echocardiography was performed according to the standard of the American Society of Echocardiography. Patients were advised to rest for 5 minutes before the test. Two-dimensional M-mode echocardiography was recorded at the tip of the mitral valve leaflets at the parasternal long-axis view. Left ventricular internal diameter during diastole and systole (LVIDd and LVIDs), inter-ventricular septal thickness during diastole and systole (IVSTd and IVSTs), left ventricular posterior wall thickness during diastole and systole (LVPWd and LVPWs), left ventricular ejection fraction, and fractional shortening were obtained by the standard method.Reference Sahn, DeMaria, Kisslo and Weyman 14 The left ventricular mass was thus calculated using the following equationReference Lang, Bierig and Devereux 15 : Left ventricular mass (g)=0.8 [1.04(LVIDd+LVPWd+IVSTd)3−(LVIDd)3]+0.6.
Left ventricular mass index was calculated with the left ventricular mass adjusted by surface area or height2.7. All echocardiographic images were recorded on super-VHS tape. The average of at least three consecutive cardiac cycles was taken. The images were reviewed under the software in the echocardiographic machine. The measurement tools could be checked against with the calibre shown in the M-mode image, and then the specific measurements such as inter-ventricular wall thickness and posterior wall thickness were recorded.
Anthropometry
Standing height without shoes was measured using a Harpenden Stadiometer to the nearest 0.1 cm. Body weight and percentage of body fat were measured using a portable Tanita body fat monitor/scale (model BF-522; Tanita Corporation, Tokyo, Japan). Waist circumference was measured to the nearest 0.1 cm midway between the lowest rib and the superior border of the iliac crest with an inelastic measuring tape.
Data processing and analysis
Data were presented as mean (standard deviation) and frequency (percentage) as appropriate. The demographic data, anthropometric data, laboratory outcomes, and left ventricular mass index among different ambulatory blood pressure statuses were compared using one-way analysis of variance with Bonferroni adjustment and independent t-test, respectively. Categorical data were compared between the groups using the χ2 test. Univariate associations between left ventricular mass index and anthropometric features, together with blood pressure level, masked hypertension status, age, gender, laboratory results, and history of parental hypertension, were examined using Pearson’s correlation or Student’s paired t-test. Multivariate linear regression analysis was performed using the characteristics obtained from univariate analyses (p<0.1) as predictors for left ventricular mass index. Regression model was further refined using a forward stepwise selection method. All statistical tests are two-sided and a p-value<0.05 is considered statistically significant. SPSS for Windows software (version 21.0, SPSS Inc., Chicago, Illinois, United States of America) was used for the statistics.
Results
Baseline
In this study, the baseline data were collected in a 2011/2012 Hong Kong Chinese children 24-hour ambulatory blood pressure monitoring study. Of 1445 patients, 165 (11.4%) had masked hypertension and 1280 (88.6%) were normotensive. All patients were Chinese children and adolescents in Hong Kong. Sex ratio, age, height, and body mass index z-score were similar between these two groups, but all blood pressure parameters were higher in the patients with masked hypertension (Table 1). Body weight (45.4 [13.8] versus 48.4 [16.0] kg, p=0.009) and body fat (20.7 [7.2] versus 22.4 [8.5]%, p=0.005) were lower in normotensive patients.
Table 1 Characteristics of the demographics, anthropometrics, laboratory results, blood pressure, and echocardiographic data in three groups of the patients.

BMI=body mass index; DBP=diastolic blood pressure; HDL=high-density lipid; HOMA=homoeostasis model assessment; LV=left ventricular; MH=masked hypertension; QUICKI=quantitative insulin sensitivity check index; SBP=systolic blood pressure
* Comparisons between patients with and without persistent MH
** Comparisons between patients with persistent MH and control
*** Comparisons between patients without persistent MH and control
Follow-up
Characteristics, laboratory outcomes, blood pressure, and echocardiographic data of patients with and without persistent masked hypertension and the controls are reported in Table 2. Consents were obtained from 144 out of 165 patients (87%) with masked hypertension in 2011/2012 ambulatory blood pressure survey. In all, 21 patients were excluded because of the inability to obtain consents. Of 144 adolescents identified as having masked hypertension who underwent ambulatory blood pressure monitoring and echocardiography from August 2015 to June 2016, 48 adolescents were diagnosed to have persistent masked hypertension by ambulatory blood pressure rechecking and were matched with normotensive controls by sex, age, and body height (Fig 1). None of the patients was found to be primary or secondary hypertensive. Those patients with persistent masked hypertension were older and heavier than the patients without persistent masked hypertension. Significantly more boys had persistent masked hypertension than their female counterparts (Table 1).
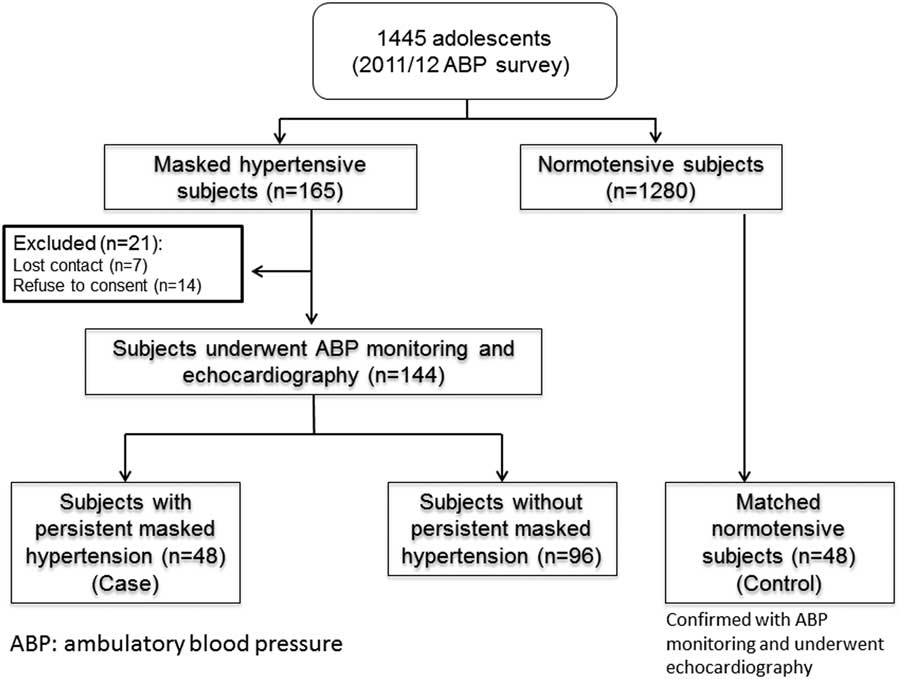
Figure 1 Study flow chart. ABP=ambulatory blood pressure.
Table 2 Activity and dietary data in the three groups.

MH=masked hypertension
* Comparisons between patients with and without persistent MH
** Comparisons between patients with persistent MH and control
*** Comparisons between patients without persistent MH and control
Anthropometric parameters
The patients with persistent masked hypertension were taller (p=0.015) and heavier (p<0.0001) than the patients without persistent masked hypertension (Table 1). Moreover, the rate of obesity doubled in the patients with persistent masked hypertension (22.9%) as compared with those without persistent masked hypertension (11.5%) and the controls (6.3%). However, there was no difference of percentage of body fat and waist circumference z-score among these three groups (Table 1).
Laboratory outcomes
Fasting plasma glucose, insulin, and homoeostatic model assessment were significantly higher in the patients with persistent masked hypertension (Table 1), whereas high-density lipid cholesterol was lower in the patients with persistent masked hypertension. In contrast, low-density lipoprotein cholesterol and non-high-density lipid cholesterol were higher in these patients. No difference was found in terms of total cholesterol and triglycerides across the three groups (Table 1).
Blood pressure
Among the 144 patients with masked hypertension at baseline, 96 (66.7%) became normotensive – without persistent masked hypertension – and 48 (33.3%) had persistent masked hypertension. The casual systolic blood pressure (p=0.001) and diastolic blood pressure (p=0.003) were significantly higher in the patients with persistent masked hypertension compared with those without persistent masked hypertension (Table 1). However, there was no difference in casual blood pressure between the persistent masked hypertension group and the control group. Comparing with the patients in both without persistent masked hypertension and control groups, daytime systolic blood pressure, daytime diastolic blood pressure, night-time systolic blood pressure, and night-time diastolic blood pressure were significantly higher in the patients with persistent masked hypertension.
Assessment of diet and physical activity
Regarding nutrient intake, the control group showed significantly higher energy intake, more from sugar and fat. On comparing nutrient density, three groups showed that there were no significant differences in protein, carbohydrate, fibre, potassium, sodium, vitamin C, calcium, copper, iron, magnesium, manganese, phosphorus, and zinc intake (Table 2). There was no difference in physical activity level (4.3 [2.6] versus 4.4 [2.8] versus 5.3 [3.1]) among the three groups (p=0.152).
Echocardiography
The left ventricular mass – persistent masked hypertension: 117.3 [39.9] versus without persistent masked hypertension: 87.0 [28.2] versus control: 102.0 [28.2] g – and left ventricular mass index – persistent masked hypertension: 30.1 [8.4] versus without persistent masked hypertension: 23.9 [6.3] versus control: 25.1 [5.7] g/m2.7 – were significantly higher in the persistent masked hypertension group (p<0.0001) (Table 1). None of the patients fulfilled the criteria for left ventricular hypertrophy (left ventricular mass index >51 g/m2.7) defined by de Simone et al,Reference de Simone, Devereux, Daniels, Koren, Meyer and Laragh 16 but 11 patients – eight with persistent masked hypertension, two without persistent masked hypertension, and one control – were classified as having left ventricular hypertrophy on the basis of left ventricular mass index ⩾38 g/m2.7 suggested for the diagnosis of left ventricular hypertrophy in children with chronic kidney disease.Reference Matteucci, Chinali and Rinelli 17
Correlation analyses demonstrated that left ventricular mass index significantly correlated with all ambulatory blood pressure parameters, body size, and lipid profile parameters, but not age and parental history of hypertension. Several characteristics that were statistically significantly correlated with left ventricular mass index under univariate analyses were no longer significant when analysed by multivariate linear regression analysis (Table 3); left ventricular mass index was found to be higher in male gender (β=4.874, p<0.0001) and in patients with persistent masked hypertension (β=2.796, p=0.003). Meanwhile, it was positively associated with body mass index z-score (β=3.045, p<0.0001) and low-density lipoprotein cholesterol concentration (β=1.634, p=0.015).
Table 3 Association between left ventricular mass index, gender, body mass index (BMI) z-score, ambulatory blood pressure, persistent masked hypertension (MH), and laboratory results

DBP=diastolic blood pressure; HDL=high-density lipid; HOMA=homoeostasis model assessment; QUICKI=quantitative insulin sensitivity check index; SBP=systolic blood pressure
Discussion
Approximately one-third of the patients with masked hypertension at baseline are confirmed to have persistent masked hypertension in this 4-year follow-up. Therefore, the prevalence of the persistent masked hypertension in this community cohort is around 33%. Left ventricular mass index is higher in males and in patients with persistent masked hypertension, associated with body mass index z-score and low-density lipoprotein cholesterol concentration. Our findings are compatible with those of previous studies.Reference McNiece, Gupta-Malhotra and Samuels 4 , Reference Verberk, Kessels and de Leeuw 18 – Reference de Simone, Devereux, Daniels and Meyer 20 However, to our knowledge, the association between left ventricular mass index and low-density lipoprotein cholesterol concentration is first reported in children with masked hypertension. Recently, Wu et al,Reference Wu, Wu, Fan, Zhou and Xu 21 in a longitudinal study, reported that low-density lipoprotein cholesterol concentration was predictive of the development of elevated left ventricular mass index among elderly women. Dyslipidaemia is recognised as a prominent risk factor for cardiovascular disease. Buono et alReference Buono, Spinelli and Giallauria 22 reported that poor control of low-density lipoprotein cholesterol concentration after myocardial infarction would affect left ventricular remodelling. For this study, low-density lipoprotein cholesterol concentration is positively associated with the left ventricular mass index, but not hypertrophy, in multivariable linear regression.
Persistent masked hypertension is associated with increased left ventricular mass index, which may suggest that masked hypertension increased cardiovascular risk in these adolescents. The number of human cardiac myocytes is determined at the 1st year after birth. Thus, subsequent increases in left ventricular mass reflect cardiac cellular enlargement. According to the studies in normal adults, left ventricular mass is larger in men than in women.Reference de Simone, Daniels and Devereux 23 de Simone et alReference de Simone, Devereux, Daniels, Koren, Meyer and Laragh 16 reported that this difference might be owing to a gender difference in the number of myocytes that was programmed in early life or a hypertrophy of myocytes during development in males. Body mass index z-score and blood pressure are recognised as predictors of cardiovascular disease. The present study further highlighted that body mass index z-score and persistent masked hypertension are independently associated with left ventricular mass index. These findings suggest that effective control of body weight and blood pressure might be crucial in the early prevention of left ventricular hypertrophy. In addition, childhood adiposity has been shown to independently predict higher left ventricular mass in adulthood.Reference Li, Li, Ulusoy, Chen, Srinivasan and Berenson 24
Although left ventricular hypertrophy is the most well-documented end-organ manifestation of hypertensive disease in children, none of the patients in this study had left ventricular hypertrophy with the definition as left ventricular mass index >51 g/m2.7 recommended by de Simone et al.Reference de Simone, Devereux, Daniels, Koren, Meyer and Laragh 16 The prevalence of left ventricular hypertrophy can be different using different cut-offs of left ventricular hypertrophy.Reference Flynn and Falkner 25 The Effect of Strict Blood Pressure Control and ACE Inhibition on the Progression of CKD in Pediatric Patients (ESCAPE) trial defined left ventricular hypertrophy on the basis of left ventricular mass index ⩾38 g/m2.7, the 95th percentile value in healthy children.Reference de Simone, Daniels and Kimball 26 With the use of this left ventricular mass index cut-off, 11 patients – eight with persistent masked hypertension, two without persistent masked hypertension, and one control – in the present study were classified as having left ventricular hypertrophy. However, the use of this cut-off overestimates the prevalence of left ventricular hypertrophy, especially in young individuals, as reported by Mitsnefes et al.Reference Mitsnefes, Flynn and Cohn 19 In addition, one patients in the control group was classified as having left ventricular hypertrophy with this definition. Recently, age-specific reference values for left ventricular mass index ⩾95th percentile was developed in children, but it was recommended for patients aged <9 years.Reference Khoury, Mitsnefes, Daniels and Kimball 27 Percentile curves were better used in children aged <9 years, rather than using a single cut-off value. The left ventricular mass index of 51 g/m2.7 was used for the diagnosis of left ventricular hypertrophy in the present study because this cut-off is associated with cardiovascular morbidity in patients with hypertension.
The strengths of this study include a large community cohort with comprehensive standardised echocardiographic measures, such as demographic, clinical, laboratory data, and longitudinal ambulatory blood pressure monitoring. However, there are some limitations in our study. Left ventricular mass calculated based on echocardiography may be overestimated when compared with the gold standard of MRI.Reference Konstam, Kramer, Patel, Maron and Udelson 28 However, echocardiography is being widely used for observing alterations in left ventricular geometry and structure.Reference Lang, Bierig and Devereux 29 For the convenience and practicability of echocardiography in large-scale investigation, it is the preferred choice for our study design. The patients were identified as having masked hypertension at baseline based on an elevated daytime ambulatory blood pressure. Over a 4-year follow-up period, one-third of these patients with masked hypertension remained hypertensive on daytime ambulatory blood pressure. In comparison with the normotensive controls and patients without persistent masked hypertension, patients with masked hypertension also had an elevated night-time blood pressure and higher left ventricular mass index, which suggests that their blood pressure was truly elevated. Although the present study shows that low-density lipoprotein cholesterol concentration might contribute to the increased left ventricular mass index, the laboratory results were not available at baseline. Therefore, the effect of the change in the low-density lipoprotein cholesterol concentration on left ventricular mass index cannot be determined.
The present study suggests that our ambulatory blood pressure classification scheme might better identify children and adolescents who are at risk for cardiac end-organ damage than casual blood pressure alone. Without ambulatory blood pressure monitoring, those adolescents with masked hypertension cannot be detected. There is diagnostic disagreement between casual blood pressure and ambulatory blood pressure; the target organ damage seems best predicted by ambulatory blood pressure. Our data also provide the information on whether masked hypertension is a reproducible phenomenon and becomes less frequent with repeated ambulatory blood pressure monitoring at follow-up. Given that persistent masked hypertension in adolescents has been linked to higher left ventricular mass index, long-term follow-up will also allow us to evaluate the association of persistent masked hypertension with progression of left ventricular hypertrophy in our cohort.
Conclusions
Persistent masked hypertension in adolescents is associated with higher left ventricular mass index.
Acknowledgements
The authors thank all the patients who participated in the study.
Author Contributions
M.C.Y. had full access to the study data and prepared the initial draft of the article. H.K.S. coordinated the study and assisted in the supervision of data collection. H.K.S. and S.Y.K. took active part in the statistical work. S.Y.K., F.C.L., C.F.M., C.K.L., W.K.Y., and Y.T.S. critically revised the manuscript for important intellectual content. M.C.Y., H.K.S., and Y.T.S. prepared the proposal and supervised the study. All authors contributed to the paper’s submitted form and have read and approved the final paper.
Financial Support
The authors are grateful to the Health and Medical Research Fund, Food and Health Bureau, Hong Kong SAR Government (Ref no.: 12131351).
Conflicts of Interest
None.
Ethical Standards
The study was approved by the Ethics Committee on Clinical Research, The Chinese University of Hong Kong and the Ethics Committee of the participating hospitals. This study was conducted according to the ethical guidelines and principles of the International Declaration of Helsinki.







