Introduction
Managing patients with mental and physical multi-morbidity is a major challenge for modern healthcare systems, and these patients often have poor outcomes (Mercer et al. Reference Mercer, Gunn, Bower, Wyke and Guthrie2012; Smith et al. Reference Smith, Soubhi, Fortin, Hudon and O'Dowd2012). Persons with schizophrenia and bipolar affective disorder have, for example, a two- to three-fold increased risk of premature death (Laursen et al. Reference Laursen, Munk-Olsen, Nordentoft and Mortensen2007; Osborn et al. Reference Osborn, Levy, Nazareth, Petersen, Islam and King2007; Hoang et al. Reference Hoang, Stewart and Goldacre2011; Wahlbeck et al. Reference Wahlbeck, Westman, Nordentoft, Gissler and Laursen2011), which corresponds to a life expectancy gap of 15–20 years compared with the background population (Wahlbeck et al. Reference Wahlbeck, Westman, Nordentoft, Gissler and Laursen2011). Their cause-specific mortality rate ratios (MRRs) are high for almost all causes (Laursen et al. Reference Laursen, Munk-Olsen, Nordentoft and Mortensen2007; Osborn et al. Reference Osborn, Levy, Nazareth, Petersen, Islam and King2007; Wahlbeck et al. Reference Wahlbeck, Westman, Nordentoft, Gissler and Laursen2011), especially for suicide (Laursen et al. Reference Laursen, Munk-Olsen, Nordentoft and Mortensen2007; Nordentoft et al. Reference Nordentoft, Mortensen and Pedersen2011), but most of the excess mortality is explained by physical disorders (Laursen et al. Reference Laursen, Munk-Olsen, Nordentoft and Mortensen2007; Hoang et al. Reference Hoang, Stewart and Goldacre2011). The underlying causal mechanisms for this excess mortality among persons with severe mental illness are not completely understood, but may be associated with suboptimal treatment of somatic diseases (Frayne et al. Reference Frayne, Halanych, Miller, Wang, Lin, Pogach, Sharkansky, Keane, Skinner, Rosen and Berlowitz2005; Hippisley-Cox et al. Reference Hippisley-Cox, Parker, Coupland and Vinogradova2007), co-morbidity (Fleischhacker et al. Reference Fleischhacker, Cetkovich-Bakmas, De Hert, Hennekens, Lambert, Leucht, Maj, McIntyre, Naber, Newcomer, Olfson, Osby, Sartorius and Lieberman2008; Laursen et al. Reference Laursen, Munk-Olsen and Gasse2011), metabolic disorders induced by antipsychotic medication (weight gain, dyslipidaemia, diabetes and the metabolic syndrome) (American Diabetes Association et al. 2004) and unhealthy life-style (sedentary life-style, smoking, obesity and unhealthy diet) (Brown et al. Reference Brown, Birtwistle, Roe and Thompson1999; Vinogradova et al. Reference Vinogradova, Coupland, Hippisley-Cox, Whyte and Penny2010).
Although 10–20% of persons with severe mental illness have type 2 diabetes (Dixon et al. Reference Dixon, Weiden, Delahanty, Goldberg, Postrado, Lucksted and Lehman2000; Galletly et al. Reference Galletly, Foley, Waterreus, Watts, Castle, McGrath, Mackinnon and Morgan2012; Manu et al. Reference Manu, Correll, van Winkel, Wampers and De Hert2012), little is known about the long-term mortality of persons with severe mental illness and diabetes. Diabetes is associated with an increased risk of early death (Carstensen et al. Reference Carstensen, Kristensen, Ottosen and Borch-Johnsen2008; Seshasai et al. Reference Seshasai, Kaptoge, Thompson, Di, Gao, Sarwar, Whincup, Mukamal, Gillum, Holme, Njolstad, Fletcher, Nilsson, Lewington, Collins, Gudnason, Thompson, Sattar, Selvin, Hu and Danesh2011), and this association may be even stronger in persons with severe mental illness who tend to be less likely to meet diabetes performance measures (Frayne et al. Reference Frayne, Halanych, Miller, Wang, Lin, Pogach, Sharkansky, Keane, Skinner, Rosen and Berlowitz2005). Two studies have found a higher mortality among persons with severe mental illness and diabetes than among those suffering from diabetes only (Vinogradova et al. Reference Vinogradova, Coupland, Hippisley-Cox, Whyte and Penny2010) or severe mental illness only (Jackson et al. Reference Jackson, Covell, Drake and Essock2007). However, one study showed no difference in mortality for persons with severe mental illness and diabetes as compared with those suffering from diabetes only (Brown et al. Reference Brown, Leith, Dickerson, Medoff, Kreyenbuhl, Fang, Goldberg, Potts and Dixon2010). No studies have compared these patients' mortality rates with those of the background population or assessed their cause-specific mortality.
The aim of the present study was to study the overall and cause-specific mortality for all persons with severe mental illness with co-occurring incident diabetes in a large population-based cohort with up to 13 years of follow-up.
Method
Study population
A population-based cohort study was conducted by using information from nationwide registries, including the Danish Civil Registration System (CRS) (Pedersen et al. Reference Pedersen, Gotzsche, Moller and Mortensen2006), the Danish Psychiatric Central Register (Mors et al. Reference Mors, Perto and Mortensen2011), the Danish National Diabetes Register (Carstensen et al. Reference Carstensen, Kristensen, Ottosen and Borch-Johnsen2008) and the Danish Causes of Death Register (Helweg-Larsen, Reference Helweg-Larsen2011). In these registries, information on Danish citizens is universally stored with reference to a unique 10-digit CRS number assigned to all Danish residents at birth. This enables accurate linkage of information on a personal level (Pedersen et al. Reference Pedersen, Gotzsche, Moller and Mortensen2006). We included all persons who were born in Denmark and alive on 1 January 1997.
Procedures
Information on date of birth, date of death or date of emigration, and total number of deaths was obtained from the Danish CRS (Pedersen et al. Reference Pedersen, Gotzsche, Moller and Mortensen2006). Information on diabetes was obtained from the Danish National Diabetes Register (Carstensen et al. Reference Carstensen, Kristensen, Ottosen and Borch-Johnsen2008), which was established by the Danish National Board of Health in order to provide information on diabetes for persons treated in primary as well as in secondary care. This register was established by linking information from the following registers: the Danish National Hospital Register (Andersen et al. Reference Andersen, Madsen, Jorgensen, Mellemkjoer and Olsen1999), the Danish National Health Insurance Service Register (Olivarius et al. Reference Olivarius, Hollnagel, Krasnik, Pedersen and Thorsen1997) and the Danish Register of Medicinal Product Statistics (Kildemoes et al. Reference Kildemoes, Sorensen and Hallas2011). The Danish National Diabetes Register does not contain information on values for measured blood glucose, and therefore the identification of persons with diabetes relies on a validated algorithm. Individuals were classified as having diabetes on the day where at least one of the following six criteria was met:
-
(1) A diagnosis of diabetes made at any Danish hospital in conformity with the Danish version of the 8th and the 10th revision of the International Classification of Diseases (ICD-8 and ICD-10) as registered in the Danish National Hospital Register. The ICD-8 (249, 250) was used until January 1994 and was thereafter replaced by the ICD-10 (E10–E14, H36.0, O24, excluding O24.4).
-
(2) A referral to chiropody of diabetic patients as registered in the Danish National Health Insurance Service Register.
-
(3) Five blood glucose measurements within 1 year as registered in the Danish National Health Insurance Service Register.
-
(4) Two blood glucose measurements per year for five consecutive years as registered in the Danish National Health Insurance Service Register.
-
(5) Two redemptions of oral glucose-lowering drugs within 6 months as registered in the Danish Register of Medicinal Product Statistics (except for women aged 20–39 years prescribed metformin alone, since this is also used as medication for polycystic ovarian syndrome).
-
(6) Two redemptions of prescribed insulin as registered in the Danish Register of Medicinal Product Statistics.
The Danish National Diabetes Register has been registering persons with diabetes since 1990. We identified persons in Denmark registered with a diagnosis of diabetes in the Danish National Diabetes Register after 1 January 1997. The proportion of identified persons with diabetes according to the criteria in the algorithm was distributed as follows: diagnosis, 27.9%; chiropody, 7.1%; five blood glucose in 1 year, 40.3%; two blood glucose in 5 years, 0.1%; oral glucose-lowering drugs, 23.9%; and insulin, 0.6%. Individuals registered from 1990 to 1997 were excluded on account of inadequate register validity in the Registry's first years of operation (Carstensen et al. Reference Carstensen, Kristensen, Ottosen and Borch-Johnsen2008).
Information on psychiatric disorders was obtained from the Danish Psychiatric Central Register (Mors et al. Reference Mors, Perto and Mortensen2011), which contains information on all admissions to psychiatric hospitals in Denmark since 1969, and on all out-patient contacts since 1995. Before 1 January 1994, diagnoses were classified according to the Danish version of ICD-8 and from 1 January 1994 according to the ICD-10. All psychiatric admissions in Denmark with a diagnosis of severe mental illness comprising schizophrenia [ICD-8: 295 (excluding 295.79), and ICD-10: F20], schizo-affective disorders (ICD-8: 295.79, 296.89, and ICD-10: F25) and bipolar affective disorders (ICD-8: 296.19, 296.39, and ICD-10: F30, F31) diagnosed after 1 January 1969 were identified at the start of follow-up.
Information on causes of death was obtained from the Danish Causes of Death Register (Helweg-Larsen, Reference Helweg-Larsen2011), which contains information on all deaths of Danish citizens and residents, place of death, and cause of death between 1970 and 2009. Causes of death were classified into 10 categories. Unnatural causes comprised suicide (ICD-10: X60–X84, Y87.0) and accidents (ICD-10: V01–X59, Y10–Y86, Y87.2, Y88–Y89). Natural causes comprised old age and apoplexy (ICD-10: I60–I72, R54, F03.9), malignant neoplasms (ICD-10: C00–D09), myocardial infarction (MI) (ICD-10: I21), cardiac death, non-MI [ICD-10: I00–I25 (excluding I21), I27 and I30–I52], respiratory diseases (ICD-10: J00–J99), endocrine and metabolic conditions (ICD-10: E00–E07, E10–E90), infectious diseases (A00–A09, A15–A99, B00–B99) and a combined group of the remaining causes of death, also including homicide (ICD-10: X85–Y09, Y87.1).
Statistical analysis
Follow-up started on 1 January 1997 and ended on 31 December 2009, the day of emigration or the day of death, whichever came first. MRRs were calculated for overall mortality, for mortality due to natural and unnatural causes, and for cause-specific mortality for persons with severe mental illness and diabetes, persons suffering from diabetes only, and persons suffering from severe mental illness only as compared with persons without either of these diseases. We evaluated whether the overall MRRs varied between the three subgroups of diseases (diabetes only, severe mental illness only or both diseases) by testing for statistical interaction on a multiplicative scale and on an additive scale. The latter was tested using the method described by Andersson et al. (Reference Andersson, Alfredsson, Kallberg, Zdravkovic and Ahlbom2005) for calculation of the synergy index for the possible synergistic action between severe mental illness and diabetes.
Further, we calculated the attributable proportion (AP) due to interaction as a measure of the excess MRR for persons with both diseases not explained by the independent effects of severe mental illness or diabetes. We used adjusted MRRs for these analyses. The AP due to interaction was calculated by subtracting the difference in MRRs between persons with diabetes and persons in the background population without diabetes from the difference in MRRs between persons with severe mental illness and diabetes (smi+dm) and persons with severe mental illness without diabetes (smi) and dividing this result by the MRR for persons with both diseases [e.g. APinteraction = ([MRRsmi + dm – MRRsmi] – [MRRdm – MRRbackground])/MRRsmi + dm] (Andersson et al. Reference Andersson, Alfredsson, Kallberg, Zdravkovic and Ahlbom2005). The AP due to diabetes among persons suffering from both diseases was calculated using the formula: APdiabetes = [(MRRsmi + dm – MRRsmi)/MRRsmi + dm] (Uter & Pfahlberg, Reference Uter and Pfahlberg1999). This proportion estimated the proportion of deaths that would not have occurred if persons with severe mental illness and diabetes had had the same mortality as persons with severe mental illness alone, and thus the number of hypothetically preventable deaths due to diabetes among persons with both diseases were calculated using the formula: n × APdiabetes.
Survival was analysed with time since diabetes diagnosis as a time scale, and cumulative mortality proportions (CMPs) were estimated by Kaplan–Meier curves for overall mortality. CMPs due to natural causes were estimated by the Aalen–Johansen estimator, taking into account the competing risk from unnatural causes of death. The risk of dying during this period was estimated for persons suffering from severe mental illness and diabetes and for persons suffering from diabetes only.
Data were analysed by using the log-linear Poisson regression, with the logarithm to the person years as an offset variable in SAS genmod (SAS Institute Inc., USA) using version 9.2 procedures. The psychiatric diagnoses schizophrenia, schizo-affective disorders and bipolar affective disorders were evaluated combined. MRRs were adjusted for age and calendar period and stratified by age and gender for overall mortality. MRRs were adjusted for age and calendar period and stratified by gender for natural, unnatural, and cause-specific deaths. Age, calendar year, diagnosis of severe mental illness and diagnosis of diabetes were treated as time-dependent variables, whereas the rest were treated as time-independent variables. Tests for differences, 95% confidence intervals (CIs) and p values were based on likelihood ratio tests.
Results
The cohort comprised 4 734 703 persons, of whom 651 080 died during the study period. A total of 37 389 persons had severe mental illness (9540 deaths), 248 176 had incident diabetes (56 858 deaths), and 4284 persons had severe mental illness and diabetes (1083 deaths) (Table 1).
Table 1. Number of deaths according to background variables for a population-based cohort in Denmark, 1997–2009 (n = 4 734 703) a
a Persons with severe mental illnesses comprised persons with schizophrenia, schizo-affective disorders and bipolar affective disorders. Information on severe mental illness since 1969 was obtained from the Danish Psychiatric Central Register. Information on diabetes since 1997 was obtained from the Danish National Diabetes Register.
Overall mortality
Overall, MRRs were higher for persons with severe mental illness and diabetes (men: 4.14, 95% CI 3.81–4.51; women: 3.13, 95% CI 2.88–3.40) as compared with those suffering from diabetes only (men: 1.75, 95% CI 1.72–1.77; women: 1.56, 95% CI 1.54–1.58) and those suffering from severe mental illness only (men: 3.06, 95% CI 2.97–3.15; women: 2.26, 95% CI 2.20–2.32) (Table 2). The interaction was lower than would be expected on a multiplicative scale (men: p < 0.0001; women: p = 0.0089) and higher than would be expected on an additive scale (synergy index for men: 1.12, 95% CI 1.00–1.26; and for women: 1.17, 95% CI 1.03–1.33).
Table 2. Mortality rate ratios for persons with diabetes, severe mental illness and severe mental illness and diabetes as compared with the background population in Denmark 1997–2009

Data are given as mortality rate ratio (95% confidence interval).
The corresponding MRRs for natural deaths were 3.92 (95% CI 3.59–4.29) for men and 3.11 (95% CI 2.86–3.39) for women among persons with severe mental illness and diabetes. The MRRs rose by decreasing age; for example, persons younger than 50 years with severe mental illness and diabetes had a 12- to 14-fold higher risk of death than the background population (Table 2).
The AP due to interaction between severe mental illness and diabetes was estimated to be 14.3% [i.e. ([3.92–2.62] – [1.74–1])/3.92] (95% CI 6.3–22.2%) and 14.8% (95% CI 7.3–22.4%) for natural deaths among men and women, respectively (Table 3).
Table 3. Mortality rates, mortality rate ratios and number of deaths evaluated for natural deaths among persons with severe mental illness and diabetes

CI, confidence interval.
The AP of natural deaths due to diabetes among persons with severe mental illness and diabetes was calculated to be 33.2% [i.e. (3.92–2.62)/3.92] and 33.4% for men and women, respectively. Consequently, the number of natural deaths that would not have occurred if persons with severe mental illness and diabetes had had the same mortality as persons with severe mental illness alone was 162 and 176 among men and women, respectively, or in total 338 out of 1013 natural deaths (33.4%) was attributed to diabetes (Table 3).
The absolute risk of dying within 7 years of the diabetes diagnosis (the CMP) for persons with severe mental illness and diabetes was 15.0% (95% CI 12.4–17.6%) for those younger than 50 years, 30.7% (95% CI 27.8–33.4%) for those aged 50–69 years, and 63.8% (95% CI 58.9–68.2%) for those aged 70 years or older. The corresponding CMPs for persons with diabetes, but no history of severe mental illness, were 5.2% (95% CI 4.9–5.4%), 17.7% (95% CI 17.5–17.9%) and 53.6% (95% CI 53.2–54.0%) (Fig. 1 a).
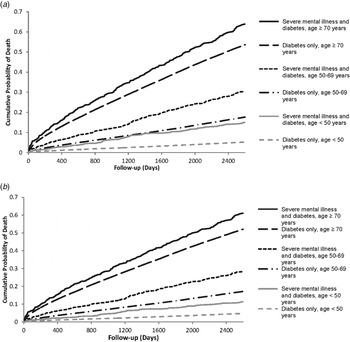
Fig. 1. Age-stratified cumulative mortality curves for persons suffering from diabetes. (a) Estimated cumulative mortality curves for overall mortality by the Kaplan–Meier estimator for up to 7 years (2600 days) after onset of diabetes plotted by applying hazard ratios for death from any cause (specific for age at risk) from the present analyses. (b) Estimated cumulative mortality curves for mortality due to natural causes by the Aalen–Johansen estimator for up to 7 years after onset of diabetes plotted by applying hazard ratios for death from natural causes (specific for age at risk) from the present analyses, taking into account competing risk from unnatural causes.
For natural causes only, the corresponding CMPs within 7 years after the diabetes diagnosis were slightly lower (Fig. 1 b).
Cause-specific death
The MRRs for all causes of death were higher for persons with diabetes, severe mental illness, and severe mental illness and diabetes than for the background population, although the association did not reach statistical significance for suicide among women with diabetes only (Fig. 2 b). The cause-specific MRRs tended to be highest for persons with severe mental illness and diabetes for natural deaths; and the cause-specific MRRs tended to be highest for persons with severe mental illness only for unnatural deaths, although not always statistically significant. For persons with both diseases, the cause-specific MRRs were lowest for malignant neoplasms (women: MRR = 1.98, 95% CI 1.64–2.39; men: MRR = 2.08, 95% CI 1.69–2.56) and highest for suicide among women (MRR = 12.31, 95% CI 6.80–22.28) and accidents among men (MRR = 7.89, 95% CI 5.51–11.29).
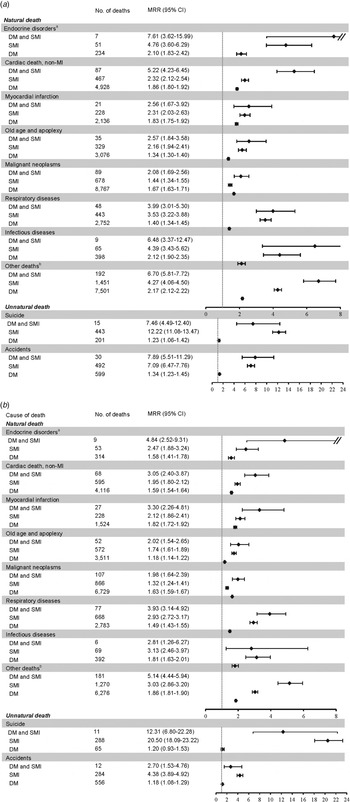
Fig. 2. Mortality rate ratios (MRRs) for cause-specific death among persons with a history of severe mental illness (SMI) and diabetes (DM), diabetes, or severe mental illness compared with persons without such a history, stratified by gender: (a) men; (b) women. a As Seshasai et al. (Reference Seshasai, Kaptoge, Thompson, Di, Gao, Sarwar, Whincup, Mukamal, Gillum, Holme, Njolstad, Fletcher, Nilsson, Lewington, Collins, Gudnason, Thompson, Sattar, Selvin, Hu and Danesh2011), we did not include death from diabetes in the endocrine category. b Other deaths = the remaining causes of death, including homicide. CI, Confidence interval; MI, myocardial infarction.
Discussion
This large population-based cohort study showed that persons with severe mental illness and diabetes had a three- to four-fold higher risk of death than the general population, and also indicated that the MRRs increased with decreasing age. Persons suffering from both severe mental illness and diabetes tended to have higher mortality than would be expected when adding the independent risk of death associated with each of the two diseases, but a lower mortality than would be expected if the risks were multiplied. Not all authors agree upon using the synergy index as an indication of biological interaction (Greenland, Reference Greenland1993; Zammit et al. Reference Zammit, Owen and Lewis2010), as it rests upon the assumption that there is no residual confounding from unmeasured or unknown risk factors (Greenland, Reference Greenland1993). Thus the results regarding synergistic action should be interpreted cautiously.
We estimated that 338 natural deaths among persons with both diseases were attributed to diabetes and would not have occurred if these persons had had the same mortality as persons with severe mental illness only. Further, we estimated that the interaction between diabetes and severe mental illness may account for 14% of the natural deaths among persons with both diseases.
The cumulative risks of death within 7 years of diabetes diagnosis for persons with severe mental illness and diabetes ranged from 15.0% for those younger than 50 years to 63.8% for those aged 70 years or older. The cause-specific MRRs tended to be highest for persons with severe mental illness and diabetes for natural deaths; and the cause-specific MRRs tended to be highest for persons with severe mental illness only for unnatural deaths. For persons with both diseases, the cause-specific MRRs were lowest for malignant neoplasms and highest for suicide and accidents.
Our study has several strengths that count a large, nationwide and population-based cohort which could be followed for up to 13 years virtually without loss to follow-up. Bias due to selection of study participants, loss to follow-up and non-response therefore cannot explain our findings. Information on mortality, psychiatric hospital contacts and diabetes diagnoses enjoyed high validity and completeness, which minimizes any potential information bias. The schizophrenia diagnosis in the Danish Psychiatric Central Register has been shown to have a sensitivity of 93% and a positive predictive value of 87% (Jakobsen et al. Reference Jakobsen, Frederiksen, Hansen, Jansson, Parnas and Werge2005), and the diabetes diagnosis in the Danish National Diabetes Register has been shown to have a sensitivity of 86% and a positive predictive value of 90% (Carstensen et al. Reference Carstensen, Kristensen, Ottosen and Borch-Johnsen2008). The validity and completeness of registration of death in the Danish CRS is considered to be close to 100% (Pedersen et al. Reference Pedersen, Gotzsche, Moller and Mortensen2006), which makes our estimates of overall mortality very accurate. However, the quality of the cause of death registration on death certificates is known to vary (Helweg-Larsen, Reference Helweg-Larsen2011), which makes the cause-specific mortality prone to bias if the quality of the diagnoses for causes of death depended on the type of underlying disease.
However, our study also has some limitations. It has been estimated that at least one-third of all persons with diabetes in the general population may go undiagnosed (American Diabetes Association, 2009), and the proportion of undiagnosed diabetes may be even higher among persons with severe mental illness. This will tend to equalize the difference between the MRRs for persons with severe mental illness and diabetes and persons suffering from severe mental illness only. This potential bias is, however, difficult to avoid because testing all participants for diabetes is not feasible in a cohort with a sufficient sample size to answer the research question raised in the present paper. In order to include only persons with newly diagnosed diabetes, we excluded persons that were registered in the Danish National Diabetes Register between 1990 and 1997, as they may be prevalent cases (Carstensen et al. Reference Carstensen, Kristensen, Ottosen and Borch-Johnsen2008). A few prevalent cases of diabetes may have been included if they were diagnosed before 1990, but did not receive any diabetes care between 1990 and 1997.
Our study was limited by a lack of important clinical information. We did not have sufficient information to evaluate how the severity of the diabetes or the severe mental illness affected the long-term outcome. In addition, we had no information on the metabolic syndrome. It has been shown that approximately 40% of persons with severe mental illness meet the criteria for the metabolic syndrome (McEvoy et al. Reference McEvoy, Meyer, Goff, Nasrallah, Davis, Sullivan, Meltzer, Hsiao, Scott Stroup and Lieberman2005; Vancampfort et al. Reference Vancampfort, Vansteelandt, Correll, Mitchell, De, Sienaert, Probst and De2013), which is the case for only approximately 20% of the background population (Ford et al. Reference Ford, Giles and Dietz2002). The metabolic syndrome is strongly associated with the risk of cardiovascular disease (Alexander et al. Reference Alexander, Landsman, Teutsch and Haffner2003), which may explain at least part of the high mortality among persons with severe mental illness alone. We had no information on potentially confounding factors such as socio-economic factors, general health status, life-style factors, medications and healthcare utilization and therefore cannot exclude residual confounding. However, some of these factors may be intermediate variables and should not be adjusted for, as they may be important steps on the causal pathway between severe mental illness, diabetes and mortality.
To our knowledge, the present study is the first to compare the overall mortality of persons with severe mental illness and diabetes with that of the background population and to estimate cause-specific MRRs. A British register-based study showed that 96 out of 416 (23.1%) persons with severe mental illness and diabetes died during 5 years of follow-up compared with 8603 out of 43 589 (19.7%) persons with diabetes only (Vinogradova et al. Reference Vinogradova, Coupland, Hippisley-Cox, Whyte and Penny2010). An American study found that 41% of 41 persons with severe mental illness and diabetes died during a 12-year follow-up period compared with 10% of 156 persons with severe mental illness alone (Jackson et al. Reference Jackson, Covell, Drake and Essock2007). In contrast, an American study found no difference in the CMPs between persons with severe mental illness and diabetes (n = 201) and persons with diabetes only (n = 99) during 7 years of follow-up (20.9% v. 21.2%) (Brown et al. Reference Brown, Leith, Dickerson, Medoff, Kreyenbuhl, Fang, Goldberg, Potts and Dixon2010). However, the authors emphasized that the lack of association could be due to confounding by factors not accounted for, such as younger age and better control of blood glucose in the group where those investigated had both diseases (Brown et al. Reference Brown, Leith, Dickerson, Medoff, Kreyenbuhl, Fang, Goldberg, Potts and Dixon2010).
The underlying mechanism of the excess mortality for persons with both severe mental illness and diabetes is unclear, but it may have several explanations. The treatment of somatic diseases among persons with severe mental illness is known to be suboptimal (Frayne et al. Reference Frayne, Halanych, Miller, Wang, Lin, Pogach, Sharkansky, Keane, Skinner, Rosen and Berlowitz2005; Hippisley-Cox et al. Reference Hippisley-Cox, Parker, Coupland and Vinogradova2007). At the healthcare-system level, the explanations for suboptimal care management of diabetes may partly be rooted in time constraints that arise because of competing conditions (Frayne et al. Reference Frayne, Halanych, Miller, Wang, Lin, Pogach, Sharkansky, Keane, Skinner, Rosen and Berlowitz2005). At the patient level, diabetes care for persons with severe mental illness may be adversely affected due to communication and adherence difficulties (Frayne et al. Reference Frayne, Halanych, Miller, Wang, Lin, Pogach, Sharkansky, Keane, Skinner, Rosen and Berlowitz2005). Furthermore, patients with schizophrenia are known to have cognitive and social dysfunctions that could hamper self-care and diabetes medication compliance (Dixon et al. Reference Dixon, Weiden, Delahanty, Goldberg, Postrado, Lucksted and Lehman2000). Finally, severe mental illness is known to be associated with substance abuse disorders (Nordentoft et al. Reference Nordentoft, Mortensen and Pedersen2011; Prisciandaro et al. Reference Prisciandaro, Gebregziabher, Grubaugh, Gilbert, Echols and Egede2011), and it has been shown that substance abuse disorders have a significant impact on the mortality of individuals with diabetes, which may stem from their inadequate diabetes care adherence (Prisciandaro et al. Reference Prisciandaro, Gebregziabher, Grubaugh, Gilbert, Echols and Egede2011). The use of antipsychotic medication has been associated with excess mortality among persons with severe mental illness in some (Saha et al. Reference Saha, Chant and McGrath2007; Ray et al. Reference Ray, Chung, Murray, Hall and Stein2009), but not in all studies (Tiihonen et al. Reference Tiihonen, Lonnqvist, Wahlbeck, Klaukka, Niskanen, Tanskanen and Haukka2009). However, little is known about the significance of antipsychotic medication for the prognosis of persons with severe mental illness and diabetes. We found that the MRRs of non-MI cardiac death were particularly high among persons with severe mental illness and diabetes. We do not know of any biological explanation for this association, but antipsychotic medication has been associated with sudden cardiac death (Ray et al. Reference Ray, Chung, Murray, Hall and Stein2009), and future studies should evaluate whether this association is particularly strong among persons with diabetes. Furthermore, although both severe mental illness and diabetes are associated with increased risk of suicide in ours as well as in other studies (Laursen et al. Reference Laursen, Munk-Olsen, Nordentoft and Mortensen2007; Nordentoft et al. Reference Nordentoft, Mortensen and Pedersen2011; Seshasai et al. Reference Seshasai, Kaptoge, Thompson, Di, Gao, Sarwar, Whincup, Mukamal, Gillum, Holme, Njolstad, Fletcher, Nilsson, Lewington, Collins, Gudnason, Thompson, Sattar, Selvin, Hu and Danesh2011), persons with both diseases tended to have a lower risk of suicide than persons suffering from severe mental illness only. This may be explained by the fact that the risk of suicide for persons with severe mental illness is highest within the first years after diagnosis (Nordentoft et al. Reference Nordentoft, Mortensen and Pedersen2011), which often lies several years prior to a possible diabetes diagnosis (Carstensen et al. Reference Carstensen, Kristensen, Ottosen and Borch-Johnsen2008; Laursen et al. Reference Laursen, Agerbo and Pedersen2009). Thus, persons with severe mental illness who survived until they had their diabetes diagnosed may be a selected subgroup with a lower risk of suicide.
Conclusions
In conclusion, persons with severe mental illness and diabetes have high mortality due to severe mental illness, diabetes and the interaction between the two diseases. An interaction between diabetes and severe mental illness increased the mortality beyond that explained by severe mental illness and diabetes acting independently. These findings call for effective intervention from a coordinated and collaborating healthcare system in order to reduce the inequality in outcome. A better understanding of why persons with severe mental illness and diabetes have a high mortality is needed in order to develop effective interventions that can improve care.
Acknowledgements
This study was supported by an unrestricted grant from the Lundbeck Foundation. T.M.L. is funded by The Stanley Medical Research Institute.
Declaration of Interest
None.







