Introduction
Globally, 3 out of 1000 children under the age of five died due to diarrhoea in 2016, accounting for 8% of all under-five deaths. The situation in India was similar, with an under-five mortality rate due to diarrhoea of 4 per 1000 live births in 2016, representing 9% of total deaths among under-five children (UNICEF, 2018). The majority of these deaths occurred in the post-neonatal period, indicating a preponderance of exogenous causes of mortality. Most of these deaths were avoidable and were usually related to poor household conditions, including sanitation and water supply, and also poor access to health care facilities (Saha & van Soest, Reference Saha and van Soest2011). Improved health care access would mitigate this, but prevention would contribute a significant contribution towards reducing deaths due to diarrhoea.
Deaths in under-five children show significant heterogeneity in risk across households (Arulampalam & Bhalotra, Reference Arulampalam and Bhalotra2006; Das Gupta, Reference Das Gupta1990; Ronsmans, Reference Ronsmans1995; Saha & van Soest, Reference Saha and van Soest2011; Shabani et al., Reference Shabani, Lutambi, Mwakalinga and Masanja2010). In particular, Das Gupta (Reference Das Gupta1990) and Ronsmans (Reference Ronsmans1995) noticed that a small proportion of households in India and rural Senegal contributed to a significant proportion of under-five children mortality, which is otherwise termed as ‘death clustering’. This clustering or heterogeneity in the mortality experience across households could be due to many exogenous factors that are common to communities or households. Such factors could be household socioeconomic status and the household’s ability to provide for the survival of children through access to sanitation and safe drinking water (Edvinsson & Janssens, Reference Edvinsson and Janssens2012) or the maternal capability of autonomous and effective functioning through education (Das Gupta, Reference Das Gupta1990; Gupta, Reference Gupta1997). Alternatively, the heterogeneity could be due to the effect of the death of a previous child affecting the subsequent child’s mortality. This effect has been called ‘state dependency’ or ‘scarring’. This process may be operationalized through death of a previous child resulting in shorter birth intervals for the succeeding infant or through maternal depression due to the previous child’s death affecting maternal functioning and therefore care for the subsequent child. Alternatively, death of an infant may also result in a household learning to reduce similar deaths, resulting in a reduction in the scarring effect. A similar clustering effect has been noticed for diarrhoea in pre-school children (Katz et al., Reference Katz, Carey, Zeger and Sommer1993).
For acute conditions such as diarrhoea, the determination of the potential sources of heterogeneity in terms of within-household factors that are common to all children in the household (inter-household heterogeneity) and those due to individual characteristics of the child with diarrhoea (intra-household heterogeneity) may not be possible. Also, it may not possible to chronologically sequester the primary case of diarrhoea within the household to make a determination of its potential transmission to other children, and thus to be able to identify the original case of diarrhoea in a household with multiple cases. Moreover, it has been established that improved water supply and improved sanitary conditions have decisive effects on the prevalence of diarrhoea at the individual level (Cairncross et al., Reference Cairncross, Hunt, Boisson, Bostoen, Curtis, Fung and Schmidt2010). Therefore, a focus on these exogenous factors with respect to diarrhoeal prevalence is still relevant.
Diarrhoeal diseases and their correlates are often conceptualized and measured at the individual level, whereas improved water supply and improved sanitation are shared household attributes that impact the health and well-being of all residents of a household. Children living in the same home environment are exposed to similar risks. This can be explained using the example of a child in a household suffering from diarrhoea. For this child it is possible that the other children in the household are also exposed to similar risks of getting diarrhoea. This child may or may not be a sibling sharing the same genetic factors. Apart from this, there are also the factors of caste, socioeconomic status and place of residence, which are exogenous and have an effect on the occurrence of diarrhoea in the household and its clustering. An understanding of diarrhoea prevalence and its tendency to cluster within households, and the changes likely to be wrought in it through modifiable factors such as safe water and sanitation, will help to provide appropriate, targeted policies. This study aimed to examine the role of improved water supply and sanitation in the occurrence of diarrhoea and the clustering of diarrhoea in households among under-five children in India.
Methods
Data were from the fourth round of the National Family Health Survey (NFHS-4) conducted in India in 2015–2016 (IIPS & ICF, 2017). The NFHS-4 is a nationally representative multistage survey designed to provide estimates of vital indicators at the district, state and national level. A total of 699,686 women were interviewed from 601,509 households. The survey collected data on sanitation and improved source of drinking water using a household questionnaire. Information on diarrhoeal disease in under-five children was obtained using a women’s questionnaire.
Households were classified as having ‘improved sanitation’ or an ‘improved source of drinking water’ using definitions taken from the Joint Monitoring Program (JMP) (WHO & UNICEF, 2018). An added refinement was that water was designated as ‘safe’ if some form of treatment was done before consumption. Having an improved source of drinking water alone will not guarantee protection from infection as it depends on the quality of water and the way it is stored. Treating water before drinking takes care of the quality. This improved drinking water variable has been labelled ‘safe water’.
The information about the occurrence of diarrhoea in a child was matched with the household characteristics. If any child belonging to the same household had reported diarrhoea during the reference period then that household was designated a ‘diarrhoeal household’. The number of children in the household that reported diarrhoea in the 14-day reference period prior to the date of the survey was recorded. Computation of the diarrhoea prevalence for clustering was carried out considering only eligible households, i.e. those with at least two children. This led to the exclusion of households with fewer than two children under the age of five years. Household clustering of diarrhoea was defined as the occurrence of diarrhoea in more than one child in households with two or more children.
The presence of clustering of diarrhoea within households was assessed by examining whether the prevalence of diarrhoea was conditioned by the number of children within a household. In the absence of clustering, the distribution of households with diarrhoea would be binomial and the probability of observing k cases of diarrhoea in a household with n children (0 ≤ k ≤ n) (Ronsmans, Reference Ronsmans1995) is given by:
The average number of children with diarrhoea in households with n children is np, and the variance np(1–p). The value of ‘p’, is estimated from the observed proportion of households with diarrhoea in the sample for each category of number of children in households. The excess of the observed number of households with diarrhoea over the expected number of households would indicate clustering. The difference between the observed and expected number of households with clustering was tested using a χ 2 test to establish the statistical significance of the departure from expected number of children with diarrhoea within households. This helps determine the presence of clustering without ascertaining the exact cause for the departure.
The overall prevalence of diarrhoea in the household and prevalence of diarrhoea clustering were examined by the exogenous variables caste, wealth quintile and the place of residence.
The variables ‘improved sanitation’ and ‘safe water’ were combined to create four categories to manage potential interaction effects: Both present, Only sanitation, Only safe water and Both absent. Adjusted odds ratios for each household characteristic category, i.e. caste, wealth quintile, place of residence and presence of sanitation and safe water, were computed by dividing the odds of diarrhoea in each of the categories by the overall odds of diarrhoea. Similarly, adjusted odds ratios for clustering were computed in the same manner. Standardizing the odds in this way enabled a comparison across the different groups within each of the selected variables. This enabled comparisons across characteristics in terms of the increase or decrease in the odds for a characteristic against the same odds without the characteristic. This standardization procedure is similar to the Prevalence Odds Ratio (POR), but does not lend itself to estimates of the statistical significance of the effect through p-values. The POR is estimated by the cross-product of a 2×2 contingency table, which represents the odds of disease in exposed as against the odds of disease in the unexposed. Because the standardization is not through such a cross-tabulation of each characteristic against the prevalence of diarrhoea or diarrhoea clustering but through the computation of an alternative ratio, it is difficult to discern its equivalence to PORs. However, a parallel can be drawn to make comparisons of the specific mean against the overall mean in ordinary least squares regression.
The use of the Prevalence Odds Ratio (POR) or Prevalence Ratio (PR) has been the subject of debate in epidemiology (Lee, Reference Lee1994; Thompson et al., Reference Thompson, Myers and Kriebel1998), mostly related to the appropriateness of the measure, statistical tools and the availability of software programmes (Lee, Reference Lee1994; Zocchetti et al., Reference Zocchetti, Consonni and Bertazzi1997). The POR is preferred for chronic diseases with long latent periods whereas the PR is used for acute illness. The ideal measure to use in the case of acute diarrhoea would be the PR, because when the prevalence of the outcome is low the POR and PR are almost the same. The choice of the measure used should be made on epidemiological reasoning (Zocchetti et al., Reference Zocchetti, Consonni and Bertazzi1997), and as it was anticipated that the prevalence of diarrhoea would not be very high the POR was used in this analysis.
Multinomial logistic regression analysis was used to predict the effect of the combined categories ‘safe water’ and ‘improved sanitation’ on the occurrence of diarrhoea and clustering of diarrhoea within households. This analysis was done for households with two or more children where clustering was possible. In the first model (Model 1) the outcome variable was divided into three categories, namely ‘no diarrhoea’, ‘one child with diarrhoea’ and ‘two or more children with diarrhoea’, which was then examined with the predictor variable of availability of water supply and sanitation within the household. In the second model (Model 2), the exogenous variables caste, wealth quintile and place of residence were also included. The results are presented as Relative Risk Ratios (RRR) with 95% confidence intervals. Data were analysed using Stata (Version 15) (StataCorp, 2018) and graphs created using the ggplot2 package in R software (Wickham, Reference Wickham2009; R Core Team, 2017).
Results
There were a total of 176,531 households with children under five years of age with information on the occurrence of diarrhoea and 59,103 households were eligible for analysis of clustering wherein there was more than one child available in the household. The household prevalence of diarrhoea was about 12%. Furthermore, the prevalence of clustering (meaning more than one child in the household with diarrhoea during the 2-week reference period before the survey) was 2.4%. Of the 22,500 children with diarrhoea, 12.6% came from just 6.5% of the total households with diarrhoea, clearly indicating the contribution of multiple cases within the same households.
The probability of clustering was evaluated by examining the null hypothesis that there was no difference in the probability of diarrhoeal occurrence by the number of children within a household. The probability of diarrhoea occurrence across households with varying number of children below five years ranging between 2 and 7 was computed and contrasted against the expected probability of diarrhoea based on the overall probability of diarrhoeal prevalence among household (i.e. p=0.1202). The observed and expected probabilities are shown in Fig. 1. The expected probability of diarrhoea was computed for each number of children in households using the binomial distribution given by the formula given in the Methods section for 2 ≤ k ≤ 7. Using these expected probabilities, the expected number of households with diarrhoea clustering was estimated as a product of the specific expected probability of diarrhoea and the number of households with 2–7 children. This was contrasted with the observed number of households with diarrhoea clustering.

Figure 1. Expected and observed probabilities of diarrhoeal occurrence in children across households with 2 or more children, India, 2015–16.
The observed and expected numbers of cases of diarrhoea within households with two or more children were tested using the chi-squared test of independence with five degrees of freedom (to allow for households with 2–7 children). The computed value of the χ 2 statistic was 82.13, which was significant at p<0.001. This served to reject the null hypothesis that there was no possible clustering of diarrhoea across households, indicating the existence of a statistically significant level of clustering. However, it does not necessarily provide causal reasoning for the same.
The overall prevalence of diarrhoea and the prevalence of clustering of diarrhoea in households by household characteristics are shown in Table 1. The overall household diarrhoeal prevalence increased as the number of children in the household increased. A similar trend was observed for clustering, with a higher prevalence occurring when the number of children in the household exceeded five.
Table 1. Overall prevalence of diarrhoea and prevalence of household clustering of diarrhoea in children aged 0–5 by household characteristics, India, 2015–16

a The total number of households for the calculation of clustering of diarrhoea was 59,103.
b The numbers in brackets are weighted percentages.
The prevalences of overall diarrhoea and diarrhoea clustering in rural households were 12.7% and 2.5%, respectively, which were higher than those in urban areas. The ‘Other’ group representing the higher caste groups had a prevalence of 10.6%, which was low when compared with those of Schedule Caste, Schedule Tribe or Other Backward Caste groups. However, the prevalence of clustering was lowest for the Scheduled Tribe group. Scheduled Caste groups had the highest burden of overall diarrhoea (12.6%) and clustering (2.6%), which was higher than the overall prevalence of diarrhoea and prevalence of clustering. The prevalences of diarrhoea and clustering were higher in poorer households than in middle and higher quintile households and lowest in the richest quintile group (13.8% and 2.8%, respectively). This association was in the expected direction. Access to improved sanitation and safe water did have an impact on both the prevalence of diarrhoea and its clustering. When both improved sanitation and safe water were available, the prevalence of diarrhoea was 8.8% and the clustering of diarrhoea in households was 1.7% when compared with the absence of both (13.63 % and 2.7 %, respectively). When it came to clustering, safe water alone had more impact on reducing diarrhoea prevalence than sanitation alone.
The odds ratios (ORs) for overall prevalence of diarrhoea were computed across the different groups of sanitation and safe water, and were adjusted with the overall odds of diarrhoea to derive the Prevalence Odds Ratios (Table 2). A similar exercise was carried out for the household clustering of diarrhoea and the POR was computed against the overall odds of household clustering of diarrhoea (Table 3). The overall OR for diarrhoea in the household was 0.1366 and for household clustering of diarrhoea it was 0.0246. To enable an easy visual comparison, the POR for diarrhoea and diarrhoea clustering within households was represented for the two extreme conditions – when both safe drinking water and sanitation were present and when both were absent (Fig. 2).
Table 2. Prevalence and Prevalence Odds Ratios (PORs) of diarrhoea in households with at least one child by socioeconomic characteristics, India, 2015–16

Table 3. Prevalence and Prevalence Odds Ratios (PORs) of household clustering of diarrhoea in households with at least one child by socioeconomic characteristics, India, 2015–16

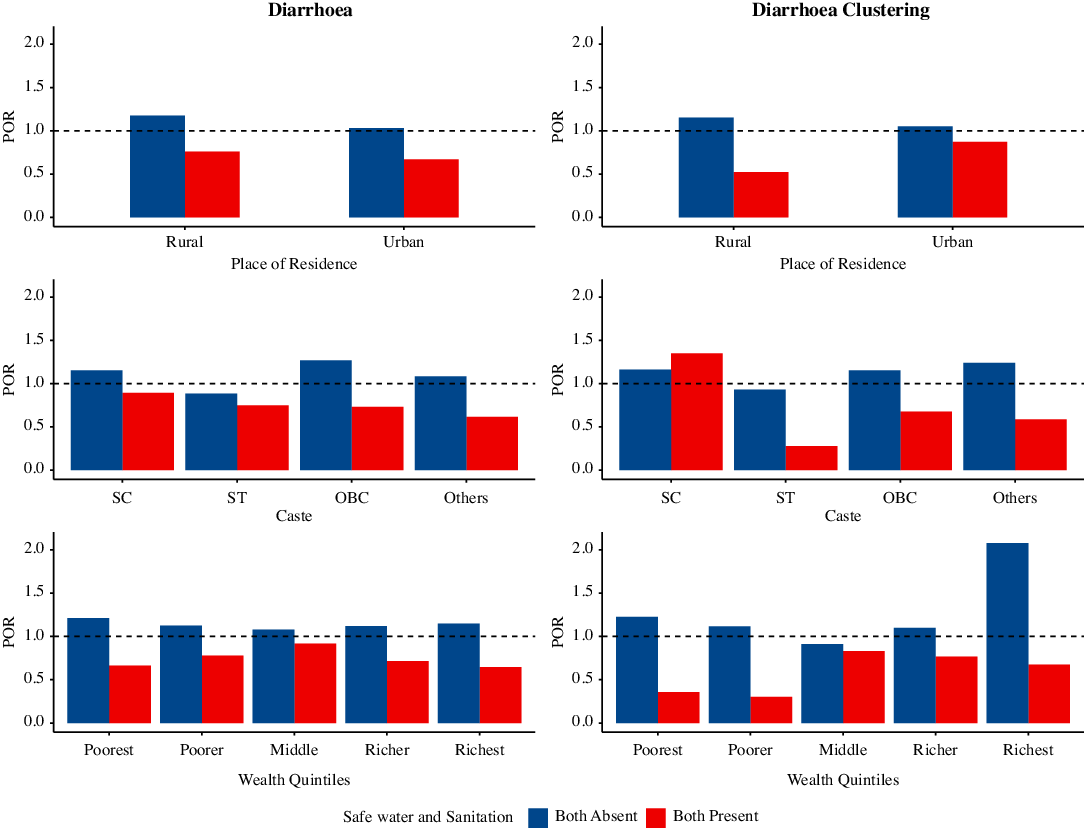
Figure 2. Prevalence odds ratios of diarrhoea and clustering of diarrhoea in households with at least one child by socioeconomic characteristics and presence and absence of sanitation and safe water, India, 2015–16.
The reduced risk in urban and rural areas due to the provisioning of sanitation and safe water was strongest in urban areas. However, the risk of diarrhoea was higher in rural areas when compared with urban areas when both were absent. When both sanitation and safe water were available to the household these tended to protect against the occurrence of diarrhoea. This reduction was observed in all caste groups except the Schedule Caste, where the reduction was only 11%. The reduction ranged from 25.1% in the Scheduled Tribes to 38.4 % in the Other (higher caste) category. However, in households with only sanitation, the risk of diarrhoea reduced by almost 10% in Schedule Caste and Other and 20% among Scheduled Tribes, but such reductions were not evident in Other Backward Class households. Having safe water reduced the risk in only the Other Backward Class and Other (higher caste) category households. Not having both increased the risk in all the groups except Scheduled Tribes.
The risk of household clustering of diarrhoea (Table 3) was reduced when there was provisioning of both improved sanitation and safe water and the reduction was almost 50% in rural areas. When both sanitation and safe water were absent the risk increased by 15% in rural areas compared with 5% in urban areas. In households with only safe water the risk reduction was greater in urban than in rural areas. The protection against clustering of episodes of diarrhoea was stronger in rural areas than urban areas, due to the presence of these two components of public health infrastructure.
The provisioning of safe water and sanitation was not effective among the Scheduled Caste group for the prevention of clustering episodes of diarrhoea. One of the possible reasons for this could be the heterogeneous nature of Scheduled Caste groups. In all other caste groups, the presence of sanitation and safe drinking water had a protective effect. The protective effect ranged from 73% in Scheduled Tribes to 23% in Other Backward Classes. In the Scheduled Tribe group, not having safe water and sanitation did not seem to increase the risk of clustering.
The presence of sanitation and safe water had a protective effect across all income groups with respect to clustering of diarrhoea in the same household. These benefits were to the tune of a decrease in adjusted/prevalence odds from 1.227 to 0.357 and from 1.115 to 0.303 among the poorest and the poorer groups on comparing the absence of sanitation and safe water with their joint presence within the household. A very significant improvement was noticed in the richest households, where the adjusted/prevalence odds declined from 2.077 to 0.674. However, it should be noted that the richest households accounted for 10% of the total households with diarrhoea clustering, and this could be the reason for the relatively larger decline in the odds of clustering depicted.
The benefits of access to sanitation and safe drinking water are nearly universal across rural and urban areas, across almost all caste groups and across all economic status groups (Fig. 2). This provides a definite advantage against clustering of diarrhoea in households compared with the prevalence of diarrhoea within households in rural areas. The presence of sanitation and safe drinking water also serves to depress the prevalence of diarrhoea clustering in Scheduled Tribes and other groups when compared with the prevalence of diarrhoea. This reduction in diarrhoea clustering was stark when both sanitation and safe drinking water were available among the richest households.
The results of the multinomial logistic regression presented in Table 4 using the unadjusted Model 1 indicate that having access to only improved sanitation increased the risk of a single child having diarrhoea in households having two or more children by 33%, and when both improved sanitation and safe water were absent the risk increased by 37%. This was in comparison to having both improved sanitation and safe water in the household. Having access to only safe water increased the risk by 10% but this was not statistically significant. Similar results were observed when two or more children in the household experienced diarrhoea episodes. However, the risk increased by almost 51% when households had access to only improved sanitation, and when both were absent the risk of clustering increased by almost 67% when compared with households that had both. Model 2, which adjusted for socioeconomic characteristics of the household, indicated an adjustment in the risk of clustering of diarrhoea to 44% from 51% (unadjusted risk ratios) when only sanitation was present, 26% from 16% (unadjusted risk ratios) when only safe water was present and 74% from 67% (unadjusted risk ratios) when both were absent. It should be noted that some of the cells for computing the adjusted risk ratios were the result of a very small number of cases and cannot be as robust. This is a serious limitation for the multivariate analysis undertaken. In so far as these adjusted risk ratios did not contradict the emerging patterns from the unadjusted model, the underlying associations indicated held.
Table 4. Multinomial logistic regression of the effect of safe water and sanitation on the clustering of diarrhoea in households with two or more children, India, 2015–16

The reference category for the outcome variable was ‘No diarrhoea in the household’. Model 1 examined the effect of water and sanitation on the occurrence of diarrhoea in a household and Model 2 examined the same effect adjusted for caste, place of residence and wealth quintiles.
***p<0.01; **p<0.05.
Discussion
This study demonstrates the potential for diarrhoea to cluster in households with more than one child in India. While its prevalence in the present sample extended to just 2.4% of households with two or more children, it represents a significant departure from an assumption of uniform prevalence of diarrhoea across households. There is clearly a potential for diarrhoea to cluster in households with multiple children. It may be possible to reduce the prevalence of diarrhoea in households by targeting those households with more than one child in the under-five age group, and by providing them with safe water and improved sanitation.
The presence of both sanitation and safe water has a strong effect in reducing both diarrhoea prevalence and its clustering within households, particularly in rural areas, amongst Scheduled Tribe and Other caste groups and among the poorest and richest households. Safe water alone has a greater impact in reducing the prevalence of diarrhoea and household clustering of diarrhoea in the absence of improved sanitation when compared with the presence of improved sanitation. The effect of the presence of safe drinking water in the household alone is nearly as good as having both sanitation and safe drinking water.
The relevance of universalization of access to safe drinking water to diarrhoea prevention among under-five children has been established in previous studies using other data and methods (Nandi et al., Reference Nandi, Megiddo, Ashok, Verma and Laxminarayan2017; Nilima et al., Reference Nilima, Shetty, Unnikrishnan, Kaushik and Rai2018; Ramanathan & Vijayan, Reference Ramanathan and Vijayan2019). The provision of piped water to rural households planned under the Jal Jeevan Mission of the Government of India (Ministry of Jal Shakthi, 2019) could contribute to the reduction in diarrhoea prevalence and its clustering in rural areas of India. This is not to say that access to improved sanitation is not important. In areas that are yet to receive sanitation improvement schemes there is a need to advocate for the use of safe water for consumption and to continue to emphasize the importance of this, even in areas where there is improved sanitation. When combined with the Swachh Bharat Mission for universalizing sanitation access (Ministry of Drinking Water and Sanitation, 2017), the impact on the household prevalence of diarrhoea among under-five children in India would be very significant because the present analysis indicates a joint potential to reduce diarrhoea clustering within households by about 75%, even after controlling for the socioeconomic conditions of the household.
Acknowledgments
The authors would like to thank Professor Udaya S. Mishra, Centre for Development Studies, Thiruvananthapuram, India, for the idea to work on morbidity at the household level and also for comments on an earlier version of this paper. They would also like to thank the organizers and reviewers of the workshop ‘Population, Health and Society in India through the Lens of the Latest NFHS Round’ for their comments on the findings of this work, which was presented at the Centre de Sciences Humaines, Delhi, on 13th and 14th December 2018. The authors are also grateful to the two anonymous reviewers for their comments, which contributed to the overall improvement in the analysis and discussion.
Funding
This work was facilitated by the funding under the project ‘Impacts of Demand Side Financing Instruments on the Continuum of Care for Maternal and Child Health in India and Bangladesh’ (BT/IN/DBT-MRC/DFID/18/USM/2015-16) jointly sponsored by the Department of Bio-technology, Government of India, Medical Research Council, UK and DFID, UK
Conflicts of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
The data used were from public resources that are anonymized. Such analysis are usually exempt from ethics review.








