INTRODUCTION
Multiple sclerosis (MS) is a neurological disease with typical onset in early adulthood (Compston & Coles, Reference Compston and Coles2008). The MS research literature has few studies of psychological moderators, such as coping style, that could affect functional outcomes. When challenged by stress, people commonly respond by using a set of coping strategies that could moderate the effects of stress on functioning. Although multiple models of coping have been described in the literature, Carver and colleagues (Carver, Scheier, & Weintraub, Reference Carver, Scheier and Weintraub1989) designed the self-regulation model as a theoretically and empirically derived approach. In this model, active coping involves a set of adaptive strategies that best allow the individual to overcome stress and return to a healthy or desired state. This includes strategies for taking action, planning a response, seeking social support, suppressing attention to competing activities, and exercising restraint from acting prematurely. Avoidant coping is comprised of less adaptive strategies associated with denial, focus on and venting of emotions, and behavioral and mental disengagement from goal attainment. The present study assessed the possible role of coping as a moderator in the relationship between fatigue and cognitive performance in MS. Use of an overall more active coping style could reduce stress and protect a highly fatigued person from experiencing cognitive problems.
Cognitive difficulties are a particularly insidious result of MS, affecting about 50% of individuals and contributing to an inability to perform daily activities (Kalmar, Gaudino, Moore, Halper, & Deluca, Reference Kalmar, Gaudino, Moore, Halper and Deluca2008). Research specifically shows impaired performance on executive functioning tasks (Benedict et al., Reference Benedict, Bruce, Dwyer, Weinstock-Guttman, Tjoa, Tavazzi and Zivadinov2007). In addition to primary disease processes, some of the common physical and psychological consequences of MS, such as fatigue, could act as stress that further contributes to cognitive problems (Diamond, Johnson, Kaufman, & Graves, Reference Diamond, Johnson, Kaufman and Graves2008). People with MS often report the experience of fatigue, which affects as many as 75 to 95% of those with MS (Lerdal, Celius, Krupp, & Dahl, Reference Lerdal, Celius, Krupp and Dahl2007), and it can be a major source of stress in their lives, interfering with the ability to engage in physical and social activities and contributing to feelings of negative affect and psychological distress (Multiple Sclerosis Council for Clinical Practice Guidelines, 1998; Thorsteinsson & Brown, Reference Thorsteinsson and Brown2009). Sustained negative somatic experiences, such as fatigue and stress arousal, can lead to biochemical and structural changes in the brain, which in turn may contribute to cognitive problems (Eriksen, Murison, Pensgaard, & Ursin, Reference Eriksen, Murison, Pensgaard and Ursin2005). While patients often report that fatigue impacts cognitive difficulties, empirical studies show mixed results. In cross-sectional analyses of the relationship between fatigue and cognition there have been positive (Diamond et al., Reference Diamond, Johnson, Kaufman and Graves2008; Parmenter, Denney, & Lynch, Reference Parmenter, Denney and Lynch2003) and negative findings (Morrow, Weinstock-Guttman, Munschauer, Hojnacki, & Benedict, Reference Morrow, Weinstock-Guttman, Munschauer, Hojnacki and Benedict2009), while a longitudinal analysis of the relationship was also negative (Morrow et al., Reference Morrow, Weinstock-Guttman, Munschauer, Hojnacki and Benedict2009). The lack of a robust effect may be due in part to the existence of moderators of the relationship between the two variables. In previous research, coping was found to moderate the relationship between cognitive difficulties and depression (Arnett, Higginson, Voss, Randolph, & Grandey, Reference Arnett, Higginson, Voss, Randolph and Grandey2002). As such, we hypothesize that coping style, as an indicator of stress management over time, will interact with fatigue and moderate its effects on cognitive functioning. Importantly, fatigue and coping may be amenable to treatment—physical activity, lifestyle changes, and medications can alleviate fatigue for many people with MS, while psychotherapeutic techniques can teach adaptive coping strategies and stress management.
The present study was based on the hypothesis that participants’ coping style would moderate the relationship between reported levels of fatigue and performance on a battery of cognitive tests. The impact of stress from fatigue over time may be related to later cognitive problems. In this study, we used a longitudinal framework to investigate the impact of coping interacting with the stress of fatigue over time on future cognitive performance. Our primary objective was to explore the development of an interactive relationship of fatigue and coping that could predict later cognitive functioning. Accordingly, we hypothesized that coping at time 1 would moderate the relationship between fatigue at time 1 as a predictor of cognitive performance at time 2. More specifically, we expected that reported levels of fatigue would account for a significant amount of variance in performance on cognitive measures, and patients with relatively high fatigue who used overall more active coping or less avoidant coping would show better cognitive performance.
METHOD
Participants and Data Collection
The study involved a longitudinal investigation of cognitive and psychosocial functioning of persons with MS. Participants were recruited through local neurologists and an MS society chapter. Exclusion criteria included history of alcohol or drug abuse, nervous system disorder other than MS, pre-morbid history of learning disability, motor or sensory impairment that could interfere with cognitive testing, and clinical exacerbation at the time of evaluation. A board-certified neurologist diagnosed each participant with definite MS, except for two participants who were diagnosed with possible MS after confirmation of diagnoses for the present study using updated criteria (Polman et al., Reference Polman, Reingold, Banwell, Clanet, Cohen, Filippi and Wolinsky2010). Participants completed a telephone screen before entering the study to determine eligibility. Participants then completed a comprehensive neuropsychological test battery and were evaluated twice over an interval of 3 years. They received written and verbal feedback as compensation, as well as $75, for each evaluation. All participants gave informed consent in accordance with institutional guidelines.
Fifty-three participants completed testing. Three were excluded from analysis due to missing data on primary measures. The final sample of 50 participants included 38 females, Caucasian 100%, mean age 47 (SD=7.7) and education 14.9 years (2.3). Course types included relapsing-remitting (62%), secondary progressive (26%), primary progressive (10%), and progressive-relapsing (2%), with mean diagnosis duration 7.6 years (6.0) and EDSS 4.5 (1.5).
Measures
Five tests that are sensitive to executive function and processing speed changes that occur with MS were included in a Cognitive Index to provide a comprehensive examination of performance and to increase analytic power. The battery included the Affective Reading Span Test (ARST) total words recalled (Bruce & Arnett, Reference Bruce and Arnett2005; see also Arnett et al. (Reference Arnett, Higginson, Voss, Bender, Wurst and Tippin1999) for a conceptual framework of reading span tests as measures of central executive functioning), Paced Auditory Serial Addition Test (PASAT) 3s version total correct, Oral Symbol Digit Modalities Test (SDMT) total correct, Tower of Hanoi total time for blocks 1 and 2 combined, and Visual Elevator from the Test of Everyday Attention time per correct switch (Robertson, Ward, Ridgeway, Nimmo-Smith, 1994). Z-scores for each of the cognitive tests were calculated using the mean and standard deviation of the sample. The summary Cognitive Index was created by averaging participants’ standardized Z-scores across the five cognitive tests. A positive index score indicated better performance in relation to the sample. The Cognitive Index from time 2 was the outcome variable in the longitudinal analysis.
Six scales of the Coping Orientation to Problems Experienced (COPE) Inventory (Carver et al., Reference Carver, Scheier and Weintraub1989) are related to Active and Avoidant Coping. The individual Active Coping scales include Active Coping, Planning, and Suppression of Competing Activities, while the individual Avoidant Coping scales include Behavioral Disengagement, Mental Disengagement, and Denial.
An individual can use a combination of active and avoidant strategies and will not necessarily score high on one measure and low on the other (Rabinowitz & Arnett, Reference Rabinowitz and Arnett2009). A Coping Style Index was created to model a holistic construct of overall coping style. Items forming the Avoidant Coping scale were reverse coded so that a higher number reflected less avoidant coping. The Coping Style Index was then calculated with an average of the Active and Avoidant Coping scales, resulting in a single score for each participant. Positive values thus reflected the use of mostly active coping whereas negative values on this index reflected mostly avoidant coping. Active Coping, Avoidant Coping, and the Coping Style Index at time 1 were each predictor variables in individual analyses.
The Fatigue Impact Scale (FIS) measures the subjective extent to which fatigue has been a problem for physical, cognitive, and psychosocial functioning over the past month (Fisk, Pontefract, Ritvo, Archibald, & Murray, Reference Fisk, Pontefract, Ritvo, Archibald and Murray1994). The FIS at time 1 was a predictor variable in the analysis.
Data Analytic Strategy
We analyzed moderation effects of coping style on the relationship between fatigue and cognition to test the hypothesis that coping moderates the relationship between fatigue and cognitive performance. Using multiple linear regression forced entry method, the one significant covariate (diagnosis duration) was entered at the step 1, followed by main effects at steps 2 and 3, and the interaction term at step 4 (FIS×coping scale).
RESULTS
Cross-sectional Analysis
The cross-sectional relationship between the FIS, coping scales, and the Cognitive Index were analyzed at time 1. There was a significant main effect of the FIS in predicting the Cognitive Index (∆F(1,48)=4.19; p<.05). There were also significant main effects of the Coping Style Index (∆F(1,47)=7.18; p<.05) and Avoidant Coping (∆F(1,47)=5.08; p<.05), but not Active Coping (∆F(1,47)=2.95; p>.05). There were no significant interaction effects between the fatigue and coping variables in predicting cognitive performance at time 1.
Longitudinal Analysis
Participant mean scores on measures of interest were as follows: FIS 61.24 (SD=34.93), Active Coping 2.88 (0.48), Avoidant Coping 3.20 (0.61), Cognitive Index raw scores: SDMT 50.34 (11.57), Visual Elevator 4.17 (1.41), ARST 19.32 (3.4), Tower of Hanoi 1029.60 (372.60), PASAT 50.72 (9.61). The results of regression analyses are summarized in Table 1. In the test of our central hypothesis for the study, that an overall measure of coping style would moderate a longitudinal relationship between fatigue and cognitive performance on an index of executive functioning measures in MS, we found an interaction effect approaching statistical significance between the FIS at time 1 and the Coping Style Index at time 1 (∆F(1,45)=3.85; p=.06), accounting for 5.3% of independent variance in predicting the Cognitive Index at time 2.
Table 1 Longitudinal regression model: Fatigue and coping at time 1 predicting cognitive functioning at time 2

Note: The dependent variable for all analyses was the Cognitive Index, time 2; n.s.=not significant.
aAvoidant COPE items were reverse coded (1=2, 2=3, 3=2, 4=1) so that higher values indicated less avoidant coping.
In the separate COPE scale analyses, the interaction effect between the FIS and Avoidant Coping was significant (∆F(1,45)=4.16; p<.05), accounting for 6.0% of independent variance in the Cognitive Index. Following procedures for interpreting moderation effects outlined in our previous work (Rabinowitz & Arnett, Reference Rabinowitz and Arnett2009), separate regression lines were calculated for the first and third quartile scores on the Cognitive Index for this significant interaction, and this is illustrated in Figure 1. The interaction of the FIS and Active Coping was not statistically significant (∆F(1,45)=2.67; p>.05).
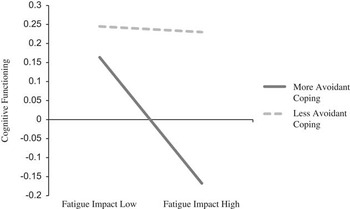
Fig. 1 Moderating effect of Avoidant Coping on the relationship between the Fatigue Impact Scale (FIS) at time 1 and the Cognitive Index at time 2.
DISCUSSION
This study contributes to research examining how coping can impact functional outcomes of disease by exploring how it interacts with fatigue to predict later cognitive problems in a community sample of people with MS. Although the correlational design of our study cannot determine causality, the study’s longitudinal framework shows that high levels of fatigue, combined with reliance on avoidant coping strategies, predict later cognitive problems. In our study, we conceptualize fatigue as stress that some individuals with MS must cope with over time; if their coping is inadequate (e.g., they over rely on avoidant coping), then this stress (fatigue) can be predictive of cognitive difficulties. It is noteworthy that the interactive relationship observed was only evident when fatigue and coping were measured at an earlier time point than cognitive functioning; no significant interaction was found when the variables were assessed cross-sectionally. This lends support to our thesis that the interaction between coping and the stress of fatigue develops over time in predicting cognitive problems. The mechanism by which such a process evolves is unclear, but the present study was designed simply to determine whether these interactive relationships existed, leaving future work to parse out why they may be present.
Our study provides evidence that coping style is associated with the ability to deal with stress, like fatigue. These results could benefit understanding of prognosis and improve treatment for patients with MS. This typically progressive disease leads to impairment for a large proportion of individuals, but there are currently limited treatments that directly target cognition. Cognitive rehabilitation may provide some benefit for executive function, but results of studies examining it have been mixed, with some showing improvement (Plohmann et al., Reference Plohmann, Kappos, Ammann, Thordai, Wittwer, Huber and Lechner-Scott1998) and others no benefit with intervention (Lincoln et al., Reference Lincoln, Dent, Harding, Weyman, Nicholl, Blumhardt and Playford2002). Acetylcholinesterase inhibitors may be beneficial for verbal memory in MS (Christodoulou et al., Reference Christodoulou, Melville, Scherl, Macallister, Elkins and Krupp2006), although its effects on other domains of cognition are not clear. Increased attention to the management of fatigue may be beneficial. Clinical interventions for fatigue could include pharmacological agents, exercise, or psychotherapy. Psychotherapy that helps patients develop adaptive coping strategies, with special attention to decreasing avoidant strategies, may also lessen the impact of high levels of fatigue on cognitive functioning.
One limitation of the study is that avoidant coping was the only coping variable to have a statistically significant interaction effect with fatigue in predicting cognitive performance. However, the amount of variance accounted for was similar for interactions involving fatigue and active coping (∆R2=0.04) as well as fatigue and the overall coping index (∆R2=0.05). A second limitation is that our study sample as a whole had moderate disability. Additional research with a lower functioning sample, including individuals who likely experience higher levels of fatigue and cognitive impairment and potentially different coping strategies, may reveal new relationships among the variables.
A final limitation of our study concerns the correlational nature of the design. The longitudinal framework makes it appealing to conclude that the variable measured earlier in time (fatigue) led to the one measured later in time (cognitive performance). However, only a true experimental design involving the manipulation of chronic fatigue and then the observation of its impact on cognitive performance could allow for causal conclusions to be made.
Taken together, the results of this study indicate that coping can moderate the impact of fatigue in people with MS. Those who reported an elevated impact of fatigue on their functioning were more likely to also show future cognitive problems if they tended to rely on avoidant coping, while those who used less avoidant coping had better cognitive functioning regardless of fatigue levels. These results may inform future research and clinical practice in identifying risk and protective factors for cognitive problems in persons with MS.
Acknowledgments
Special thanks to Christopher Higginson, William Voss, John Randolph, Pamela Freske, Jared Bruce, Dawn Polen, Lauren Strober, Megan Smith, Fiona Barwick, Amanda Rabinowitz, Gray Vargas, Frank Hillary, and Alicia Grandey for their help with various aspects of the project. These data were presented, in part, at the 30th annual meeting of the National Academy of Neuropsychology in Vancouver, British Columbia. This project was also completed in partial fulfillment of the requirements for a Master of Science degree at the Pennsylvania State University granted to the first author. This work received no specific grant from any funding agency, commercial or not-for-profit sectors, and the authors have no conflicts of interest.




